ECG How to's - CecchiniCuore.org
advertisement
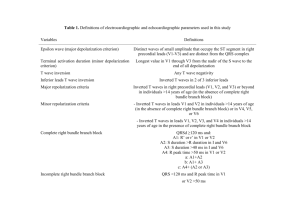
A guide to electrocardiography Reading and Applying Major Confusion!!! Reading an ECG and deciphering what it is telling you can be confusing ECG’s dictate the electrical impulses of the heart Electrical impulses are what make the heart contract This contraction is also known as depolarization A Little Vocabulary •Artifact: A wave that arises from sources other than the heart or brain. •Cardiac Arrhythmia: Any electrical activity of the heart that differs from that of a healthy awake patient. Can be innocuous or life threatening. •Deflection: movement from one side to the other. •Depolarization: Contractions as a result of cells stimulated by electricity. •Ectopic: occurring in an abnormal position. •Lead: A pair of electrodes, connected by an axis that provides a particular view of the of the electrical activity of the heart. •Repolarization: Relaxation of cells after depolarization. Cables Placement Black and white on front limbs (B=Left/W=Right) -Placed at the elbow region Green and red on back limbs (G=Right/R=Left) -Placed at the stifle region. *Alcohol, ECG paste or ECG pads can be used as conduction agents for more accurate readings. If your patient has long hair, it should be shaved at the site of cable placement in order to achieve adequate conduction in addition to the use of a conduction agent. Solid Ground •Placing the patient on a rubber mat and ensuring that the machine is plugged into a grounded outlet as well as checking the ECG machine for loose wires or cracked insulation on wires are steps that can be taken for a good ground. •Having the ECG machine well grounded is an important factor for obtaining an accurate reading. Leads •Lead I: causes right forelimb to become a negative pole and the left forelimb to become a positive pole. •Lead II: causes right forelimb to become negative and left rear limb to become positive •Lead III: the left hind limb becomes a positive pole and the left forelimb becomes a negative pole. •What happened to the Green cable you ask? It is only a reference point. Don’t forget it’s there, but concentrate on the main three! •The cables read the electrical activity of the heart between two points •Selecting specific leads on the ECG machine will cause specific cables to become negative or positive poles. (mildly complicated) Oh, no! Humans, who let them in here? Mind your PQRST’s P wave: represents atrial depolarization Therefore any changes in the P wave could indicate atrial dysfunction, or a degree of heart block QRS wave: represents ventricular depolarization So, any changes in the QRS wave could indicate ventricular fibrillation, lack of a QRS wave could indicate a form of heart block, and a wide QRS wave might indicate Premature Ventricular Contractions. T wave: Represents ventricular repolarization Myocardial hypoxia, and electrolyte disturbances can be evident with changes in the T wave. Fill in the Blanks… •P wave: Created with the depolarization of the sinoatrial node, which spreads electrical activity to the atria. This electrical impulse is spread downwards to the left, in the direction of the positive pole of lead II. Because the electrical activity is moving in a downward deflection away from the negative pole, the ECG tracing inscribes the P wave in an upward direction. Between the Lines… The PR interval is inscribed due to a delay of depolarization at the atrioventricular node (allowing time for the ventricles to fill) and no wave is produced. On your mark…. •Q Wave •The wave of depolarization moves through the Bundle of His and it’s branches, and then the interventricular septum is depolarized. This is the first part of the ventricular myocardium to become depolarized. This depolarization occurs from left to right. The electrical current moves through the thin layered interventricular septum in a downward motion, resulting in the Q wave being inscribed on the ECG. The Q wave is aimed downward because the current moves toward the negative pole. Get ready… R wave From the downward inscription of the Q wave on the ECG, depolarization spreads along the ventricular conduction system and depolarization occurs in both ventricles simultaneously. Because the Left Ventricle has greater mass than the right ventricle, most of the electrical impulse travels in a left and downward direction. This electrical activity moving in an upward deflection towards the positive pole of Lead II results in the inscription of the large R wave. Set… S wave Electrical impulses move from the apex to the base of the heart, continuing ventricular depolarization. This results in the ECG inscription of the S wave. Almost there…. ST interval After the ventricle is completely depolarized, few impulses take place during this time before repolarization (also called ventricular relaxation). This time is inscribed on the ECG as the ST interval. At this time the heart is susceptible to any electrical impulse and somewhat unstable. *This is the point where defibrillators are placed during human CPR. Go! T wave Ahhhh! Repolarization. This occurs from the endocardium to the epicardium. Because the left ventricle has more mass than the right ventricle or atria, electrical impulses travel downward to the left. This produces an upward T wave in Lead II. A period of electrical inactivity follows repolarization, and is inscribed as a flat line until the SA node begins all over again! Panic at the T Wave Sometimes the T wave can deflect downwards depending on the patient, so do not be alarmed if it looks like this on your reading. Making sense? Or do you feel like this? So What? •Now that we know how the ECG of a normal, healthy heart is produced and what it should look like, we can detect abnormalities. •Excited? •Some cardiac disturbances which can be detected are PVC’s, myocardial hypoxia, electrolyte disturbances, fibrillation, sinus bradycardia, atrial dysfunction, and other arrhythmias. Interference Remember that rubber mat and how you checked the machine for any causes of a bad ground to the machine? Interference can be caused by other machinery such as a pulseox, or BP monitor that is hooked to the animal, even fluorescent lighting. This is what interference looks like on the reading. Make a mental picture of how fuzzy it looks. Muscle Tremor •If your patient is not calm and comfortable, or just really nervous and shaky… the reading may look like this. Also caused by happy, purring feline friends. • Reapplying or readjusting the clips may help. •A towel or blanket can be placed on top of patient to help calm them. •You can also place a hand on the chest of your patient. Be careful not to apply too much pressure or it will interfere with the reading. •Looks much different than interference right? Wandering Baseline Resistance between the patient and the electrode can cause a wandering baseline. An example would be respiratory movement. Placing the patient in sternal recumbancy or a standing position will help to reduce this resistance. Holding the patient’s mouth closed for a few seconds could also help reduce resistance. Atrial Premature Contraction •The P wave of a Atrial Premature Contraction is different from that of a normal sinus rhythm. •The origin of a Atrial Premature Contraction is the sinoatrial node or displaced locations in the atria, and may or may not conduct to the ventricles; this depends on when the impulse reaches the AV node. •If depolarization occurs in the ventricles, the QRS wave will be normal. •If depolarization does NOT occur in the ventricles, and reaches the AV node before repolarization, a premature P waves w/o QRS waves will read on the ECG. Ventricular Premature Contraction Seen on ECG as wide, bizarre QRS complexes w/o associated P waves. (So this is going to be a weird and bizarre explanation.) This is because the origin of depolarization is a cell-to-cell depolarization and repolarization from the ventricular myocardium, not the SA node. In addition, if the impulse originated in the left ventricle, the wave of depolarization will be travel up, and the Ventricular Premature Contraction would be a downward deflection on the ECG. However, if the impulse originated from the right ventricle, the Ventricular Premature Contraction would travel downward and left. The ECG tracing will read an upward deflection. Escape Beats Escape Beat is a safety mechanism in the heart which functions when the SA node fails to fire an impulse. They are the result of depolarization in other locations of the heart which cause the escape beat. When the AV node depolarizes, the current travels upward into the atria and then downward to the ventricles along the normal conduction system. Escape Beats cont’d Depolarization through the ventricles produces a normal QRS complex. Depolarization through the atria causes a downward tracing of the P wave in lead II on the ECG. Depending on the speed of the upward wave of polarization, it may appear before, after or during the QRS complex. If the AV node fails to depolarize, the ventricles will take over and resemble a VPC as a wide, bizarre QRS complex w/o an associated P wave. The difference between the two is that an escape beat is life-saving, and a VPC disturbs an otherwise healthy rhythm. A B Tachycardia Can result from the use of drugs: ketamine, atropine, or epinepherine. Also due to surgical stimulation, but may not mean that anesthetic depth is too shallow unless accompanied by increased respiration, movement, or reflex reaction. Anesthetic complication? Hypoxia, hypotension, or hypercapnia Preexisting condition? Hyperthyroidism, anemia, circulatory shock, septicemia, cardiac dz,, or excitement in an awake patient Direct digital pressure can be applied to the eyeballs, or propranolol can be administered to slow the heart Sinus Tachycardia Normal sinus rhythm. Characterized by a rhythm faster then 160 beats/min in dogs and faster than 240 beats/min in cats. Ventricular Tachycardia Three or more ectopic ventricular complexes at a rate of 140 beats/min. May appear and then disappear during normal rhythm (paraxysmal ventricular tachycardia) or be present throughout. If the arrhythmia is present at all times, it indicates an irritable ventricular myocardium, and may precede ventricular fibrillation. How are you feeling? A little green? Atrial Flutter Seen as uniform, saw-tooth shaped wavelengths between QRS complexes. Can be difficult to identify. An atrial flutter is a rapid atrial depolarization which occurs at the rate of 250 -350 beats/min. The AV node becomes flooded with depolarizations from the atria. The ventricular rate varies from the atrial rate because it takes time for the AV node to catch up with all the impulses being fired at it by the atria. The ventricular rates for this arrhythmia are generally 140-150 beats/min and bizarre P waves my appear between QRS complexes. Sinus Bradycardia A normal sinus rhythm. Originated from the SA node. Characterized by a rhythm less then 60 beats/min in dogs and 70-80 beats/min in cats. Based on an individual patient basis, and may be normal for some such as athletic dogs. Atrial Fibrillation Lacking P wave Constant irregular rhythm Fast rhythm for the atria (350-600 beats/min) and ventricles (220-240 beats/min) Decreased cardiac output due to insufficient atrial contractions which lead to inadequate filling of the ventricles. Ventricular Fibrillation Chaotic depolarization of the ventricles results in disorganized contractions Inscribed on ECG as small or large undulations of the baseline, but lacking true QRS complexes Ventricular Fibrillation WILL lead to cardiac arrest!!! Heart Block: Electrical impulse is not transmitted throughout the heart First degree heart block The interval between the P wave and the QRS complex is prolonged, but the sequence is normal Second Degree heart block P waves sometimes not followed by QRS complexes Third Degree heart block P wave, QRS complex pattern is irregular 2nd and 3rd degree heart block lower the ability for the heart to contract fully. Can be caused by Alpha-2 Agonists, increased vagal tone, hyperkalemia, and cardiac dz. Heart Block cont’d Created by Emily L. Dzek Fall 2007 With MUCH help from: McKelvey, Diane and Hollingshead, Wayne K. Veterinary Anesthesia and Analgesia. 3rd ed. St. Louis: Mosby, 2003. Glaze, Kathy. “Basic Electrocardiography Part I”. Veterinary Technician 17(1996):661-667. Glaze, Kathy. “Basic Electrocardiography Part II”. Veterinary Technician 17(1996):719-725. Glaze, Kathy. “basic Electrocardiography Part III”. Veterinary Technician 18(1997). Many pictures from online sources Rhythm strip examples from Veterinary Technician magazine listed above.