ECG Interpretation
advertisement

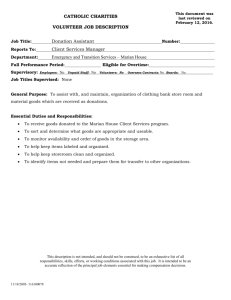
BASIC ECG INTERPRETATION Marian Williams RN BN CEN CCRN CFRN CTRN Marian Williams RN Heart Anatomy Layers Pericardium Myocardium Endocardium Four Chambers Atria Left Right Ventricles Left Right Marian Williams RN Marian Williams RN Heart Valves Atrioventricular Bicuspid Tricuspid Semi-lunar Pulmonic Aortic Marian Williams RN Marian Williams RN Major Vessels Superior Vena Cava Inferior Vena Cava Coronary Sinus Aorta Pulmonary Vein Pulmonary Artery Marian Williams RN Heart Blood Flow Marian Williams RN Cardiac Cycle Atrial Systole Atrial Kick Atrial Diastole Ventricular Systole Ventricular Diastole Marian Williams RN Marian Williams RN Coronary Arteries Right Coronary Artery Posterior Descending SA Node (60%) Right Atrium Right Marginal Right Ventricle AV node (85%-90%) Proximal portion Bundle of His Part of Left Bundle Branch Marian Williams RN Marian Williams RN Coronary Arteries Left Coronary Artery Left Anterior Descending Anterior – Left Ventricle Right Bundle Branch Part – Lateral Left Ventricle Most Interventricular Septum Left Bundle Branch Marian Williams RN Coronary Arteries Circumflex Left Atrium Lateral – Left Ventricle Inferior–Left Ventricle (15%) Posterior-Left Ventricle SA Node (40%) AV Node (10%-15%) Marian Williams RN Cardiac Muscle Syncytium Network of cells – Electrical impulses Atrial Ventricular Sarcolemma Membrane enclosing cardiac cell Marian Williams RN Cardiac Muscle Sarcolemma Holes in Sarcolemma T-(transverse) tubules Go around muscle cells Conduct impulses Sarcoplasmic Reticulum Series of tubules Stores Calcium Calcium moved from sarcoplasm into sarcoplasmic reticulum by pumps Marian Williams RN Cardiac Muscle Sarcomeres Made of thick and thin filaments Thin Troponin Thick Myosin Contraction Thin/thick filaments slide over each other Marian Williams RN Cardiac Muscle Marian Williams RN ION Concentrations Extracellular Sodium and Chloride Intracellular Potassium and Calcium Cardiac Muscle Channels Openings (pores) in cell membrane Sodium – Na+ Potassium – K+ Calcium – Ca++ Magnesium – Mg++ Marian Williams RN EFFECTS ON HEART RATE 1. Baroreceptors (Pressure) Internal Carotids Aortic Arches Detects changes in BP 2. Chemoreceptors Internal Carotids Aortic Arches Changes in pH (Hydrogen Ion, Oxygen, Carbon Dioxide) Marian Williams RN Autonomic Nervous System Parasympathetic SA Node Atrial Muscle AV Node Vagus Nerve Acetycholine is released and binds to parasympathetic receptors Slows SA node rate Slows AV Conduction Decreases atrial contraction strength Marian Williams RN Autonomic Nervous System Sympathetic Electrical system Atrium Ventricles Norepinephrine release Increased force of contraction Increased heart rate Increased BP Marian Williams RN Autonomic Nervous System Sympathetic Receptor Sites Alpha Receptors Constriction of blood vessels Skin Cerebral Splanchnic Beta 1 Receptors Heart Beta 2 Receptors Lungs Skeletal Muscle Blood Cells Marian Williams RN Dopaminergic Receptors Coronary arteries Renal Blood Vessels Mesenteric Blood Vessels Visceral Blood Vessels CARDIAC OUTPUT Stroke Volume x Heart Rate = CO (4-8 L/min) Stroke Volume approx. 70 ml/beat Increased by: Adrenal medulla Norepinephrine; Epinephrine Pancreas Insulin; Glucagon Medications Calcium; Digitalis; Dopamine; Dobutamine Marian Williams RN CARDIAC OUTPUT Decrease in Force of Contraction Severe hypoxia Decreased pH Elevated carbon dioxide Medications – Calcium channel blockers, Beta Blockers Marian Williams RN BLOOD PRESSURE Definition Force exerted by circulating blood on artery walls Equals: Cardiac output x’s peripheral vascular resistance CO x PVR Marian Williams RN STROKE VOLUME Stroke Volume determined by Preload Force exerted on ventricles walls at end of diastole Increased volume means increased preload Afterload Pressure or resistance against which the ventricles must pump to eject blood Marian Williams RN Marian Williams RN STROKE VOLUME Afterload influenced by: Arterial BP Ability of arteries to stretch Arterial resistance Marian Williams RN STROKE VOLUME Frank Starling’s Law The greater the volume of blood in the heart during diastole, the more forceful the cardiac contraction, the more blood the ventricle will pump (to a point) Marian Williams RN CARDIAC CELLS Two Types Myocardial Cells Mechanical Can be electrically stimulated Cannot generate electricity Pacemaker Cells Electrical cells Spontaneously generate electrical impulses Conduct electrical impulses Marian Williams RN CARDIAC CELLS Current Electrical charge flow from one point to another Voltage Energy measurement between positive and negative points Measured in millivolts Marian Williams RN CARDIAC CELLS Action Potential Five Phase cycle reflecting the difference in concentration of electrolytes (Na+, K+, Ca++, Cl-) which are charged particles across a cell membrane The imbalance of these charged particles make the cells excitable Marian Williams RN Cardiac Cell Action Potential Phase 0 Depolarization Rapid Na+ entry into cell Phase 1 Early depolarization Ca++ slowly enters cell Phase 2 Plateau-continuation of repolarization Slow entry of Sodium and Calcium into cell Cardiac Cell Action Potential Phase 3 Potassium is moved out of the cell Phase 4 Return to resting membrane potential CARDIAC CELLS At rest K+ leaks out Protein & phosphates are negatively charged, large and remain inside cell Polarized Cell More negative inside than outside Membrane potential is difference in electrical charge (voltage) across cell membrane Marian Williams RN CARDIAC CELLS Current (flow of energy) of electrolytes from one side of the cell membrane to the other requires energy (ATP) Expressed as volts Measured as ECG Marian Williams RN CARDIAC CELLS Depolarization When interior of cell becomes more positive than negative Na+ and Ca+ move into cell and K+ and Cl- move out Electrical impulse begins (usually) in SA node through electrical cells and spreads through myocardial cells Marian Williams RN CARDIAC CELLS Repolarization Inside of cell restored to negative charge Returning to resting stage starts from epicardium to endocardium Marian Williams RN CARDIAC CELLS Action Potential Phase 0 – rapid depolarization Na+ into cell rapidly Ca++ into cell slowly K+ slowly leaks out Phase 1 – early rapid repolarization Na+ into cell slows Cl- enters cell K+ leaves Marian Williams RN Phase 2 – Plateau Ca++ slowly enters cell K+ still leaves Phase 3 – Final rapid repolarization K+ out of cell quickly Na+ & Ca++ stop entering VERY SENSITIVE TO ELECTRICAL STIMULATION CARDIAC CELLS Phase 4 – Resting membrane potential Na+ excess outside K+ excess inside Ready to discharge Marian Williams RN CARDIAC CELLS Properties Automaticity 1. 1. Cardiac pacemaker cells create an electrical impulse without being stimulated from another source Excitability 2. 1. 2. Irritability Ability of cardiac muscle to respond to an outside stimulus, Chemical, Mechanical, Electrical Marian Williams RN CARDIAC CELLS 3.Conductivity Ability of cardiac cell to receive an electrical impulse and conduct it to an adjoining cardiac cell 4.Contractility Marian Williams RN Ability of myocardial cells to shorten in response to an impulse CARDIAC CELLS Refractory Periods Period of recovery cell needs after being discharged before they are able to respond to a stimulus Absolute Refractory Relative Refractory Supernormal ERP – Effective refractory period Marian Williams RN CARDIAC CELLS Absolute refractory Cell will not respond to further stimulation Relative refractory Vulnerable period Some cardiac cells have repolarized and can be stimulated to respond to a stronger than normal stimulus Marian Williams RN CARDIAC CELLS Supernormal Period A weaker than normal stimulus can cause cardiac cells to depolarize during this period Marian Williams RN CONDUCTION SYSTEM Sinoatrial Node (SA) Primary pacemaker Intrinsic rate 60- 100/min Located in Rt. Atrium Supplied by sympathetic and parasympathetic nerve fibers Blood from RCA-60% of people Marian Williams RN CONDUCTION SYSTEM Three internodal pathways Anterior tract Bachmann’s Bundle Left atrium Wenckebach’s Bundle Thorel’s Pathway Marian Williams RN CONDUCTION SYSTEM Atrioventricular Junction Internodal pathways merge AV Node Non-branching portion of the Bundle of His Marian Williams RN CONDUCTION SYSTEM AV Node Supplied by RCA – 85%-90% of people Left circumflex artery in rest of people Delay in conduction due to smaller fivers Marian Williams RN CONDUCTION SYSTEM Bundle of His Located in upper portion of interventricular septum Intrinsic rate 4060/min Blood from LAD and Posterior Descending Less vulnerable to ischemia Marian Williams RN CONDUCTION SYSTEM Right & Left Bundle Branches RBB Right Ventricle Marian Williams RN CONDUCTION SYSTEM LBB – Left Bundle Branch Anterior Fasicle o Anterior portion left ventricle Posterior Fascicle Posterior portions of left ventricle Septal Fasicle Mid-spetum Marian Williams RN Marian Williams RN CONDUCTION SYSTEM Spread from interventricular septum to papillary muscles Continue downward to apex of heart- approx 1/3 of way Fibers then continuous with muscle cells of Rt and Lt ventricles Marian Williams RN CONDUCTION SYSTEM Purkinje Fibers Intrinsic pacemaker rate 20-40/min Impulse spreads from endocardium to epicardium Marian Williams RN ECG Records electrical voltage of heart cells Orientation of heart Conduction disturbances Electrical effects of medications and electrolytes Cardiac muscle mass Ischemia / Infarction Marian Williams RN ECG Leads Tracing of electrical activity between 2 electrodes Records the Average current flow at any specific time in any specific portion of time Marian Williams RN ECG Types of leads Limb Lead (I, II, III) Augmented (magnified) Limb Leads (aVR, aVL, aVF) Chest (Precordial) Leads (V1,V2,V3,V4,V5,V6) Each lead has Positive electrode Marian Williams RN ECG Each lead ‘sees’ heart as determined by 2 factors 1. Dominance of left ventricle 2. Position of Positive electrode on body Marian Williams RN Marian Williams RN ECG Lead I Negative electrode Right arm Positive electrode Left arm Marian Williams RN ECG Lead II Negative Electrode Right Arm Positive Electrode Left Leg Marian Williams RN ECG Lead III Negative Lead Left Arm Positive Lead Left Leg Marian Williams RN ECG PAPER Graph Paper Small boxes 1mm wide; 1 mm high Horizontal axis Time in seconds 1 mm box represents 0.04 seconds ECG paper speed is 25 mm/second One large box is 5 (1 mm boxes or 0.04 sec)=.20 seconds Marian Williams RN Marian Williams RN ECG PAPER Vertical Axis Voltage or amplitude Measured in millivolts 1mm box high is 0.1 mV 1 large box is (5 x 0.1=0.5 mV) However, in practice the vertical axis is described in millimeters. Marian Williams RN ECG PAPER Waveforms Movement from baseline Positive (upward) Negative (downward) Isoelectric –along baseline Biphasic - Both upward and downward Marian Williams RN Marian Williams RN ECG P Wave First waveform Impulse begins in SA Node in Right Atrium Downslope of P wave – is stimulation of left atrium 2.5 mm in height (max) O.11 sec. duration (max) Positive in Lead II Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG QRS Complex Electrical impulse through ventricules Larger than P wave due to larger muscle mass of ventricles Follows P wave Made up of a Q wave R wave S wave Marian Williams RN ECG Q wave First negative deflection following P wave Represents depolarization of the interventricular septum activated from left to right Marian Williams RN ECG R wave First upright waveform following the P wave Represents depolarization of ventricles Marian Williams RN ECG S wave Negative waveform following the R wave Normal duration of QRS 0.06 mm – 0.10 mm Not all QRS Complexes have a Q, R and S Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG T wave Represents ventricular repolarization Absolute refractory period present during beginning of T wave Relative refractory period at peak Usually 0.5 mm or more in height Slightly rounded Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG U wave Small waveform Follows T wave Less than 1.5 mm in amplitude Marian Williams RN Marian Williams RN ECG J Point Point where the QRS complex and ST-segment meet Marian Williams RN Marian Williams RN Marian Williams RN ECG PR Interval Measurement where P wave leaves baseline to beginning of QRS complex Activation AV Node Bundle of His Bundle Branches Purkinje Fibers Atrial repolarization 0.12 - .20 sec. Marian Williams RN Marian Williams RN Marian Williams RN ECG QT interval Begins at isoelectric line from end of S wave to the beginning of the T wave - 0.44 sec. Represents total ventricular activity Measured from beginning of QRS complex to end of T wave Marian Williams RN Marian Williams RN Marian Williams RN ECG Artifact Distortion of electrical activity Noncardiac in origin Caused by Loose electrodes Broken cables/wires Muscle tremor Patient movement 60 cycle interference Chest compressions Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG Analysis Rate Six Second Method Two – 3 second markers Count complexes and multiply x 10 Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG Analysis Regularity Atrial Rate Measure distance between P waves Ventricular Rate Measure distance between R-R intervals 0.04 mm ‘off’ is considered regular Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG Analysis Measure P wave length Measure PR Interval Measure QRS wave duration Measure QT interval Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG Analysis ST segment Elevated? Depressed? T wave Normal height Upright? Marian Williams RN Marian Williams RN Marian Williams RN ECG Normal Sinus Rhythm Electrical activity activity starts in SA node AV Junction Bundle Branches Ventricles Depolarization of atria and ventricles Rate: 60-100 /Regular PR interval / QRS duration normal Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG Sinus Bradycardia Sinus Node fires at a rate slower than normal Conduction occurs through atria, AV junction, Bundle Branches and Ventricles Depolarization of atria and ventricles occurs In adults – rate is slower than 60 / minute Rate is regular Why? Athletes; Medications Vagal Stimulation Cardiac disease Treatment: TCP; Atropine 0.5 mg IVP if symptomatic (maybe); Epinephrine or Dopamine 2-10 mcg/kg/min infusion Marian Williams RN ECG Sinus Bradycardia Causes H’s and T’s Hypoxia Hypovolemia Hydrogen Ion (acidosis) Hypo-Hyperkalemia Hypoglycemia Hypothermia Marian Williams RN Toxins Tamponade, cardiac Tension Pneumothorax Thrombosis (coronary or pulmonary) Trauma (Increased ICP; hypovolemia) Marian Williams RN Marian Williams RN Marian Williams RN ECG Sinus Tachycardia SA node fires faster than 100-180/minute Normal pathway of conduction and depolarization Regular rate Why? Coronary artery disease Hypoxia Treatment: Treat Cause Beta-Blockers Marian Williams RN Fear; anger; exercise; Fever Marian Williams RN Marian Williams RN Marian Williams RN ECG Sinus Arrhythmia The SA node fires Irregularly / Rate 60-100/min. Normal pathway of electrical conduction and depolarization PR and QRS durations are normal Why? Respiratory- Increases with inspiration; decreases with expiration Often in children; Inferior Wall MI; Increased ICP; Medications: Digoxin; Morphine Treatment: Often None Marian Williams RN Marian Williams RN Marian Williams RN Marian Williams RN ECG Sinus Arrest SA node fails to initiate electrical impulse for one or more beats May see no beats on monitor or other pacemaker cells in the heart may take over Rate: Variable ; Rhythm: Irregular Why? Hypoxia; Coronary artery disease; Hyperkalemia Beta-Blockers; CA channel blockers; Increased vagal tone Treatment Pacemaker; Marian Williams RN Atropine; Epinephrine or Dopamine Marian Williams RN Marian Williams RN Marian Williams RN ECG Premature Atrial Complexes An electrical cell within the atria fires before the SA node fires Rate: Usually closer to 100; Irregular rhythm P wave usually looks abnormal and complex occurs before it should Why? Emotional stress; CHF; Acute coronary syndromes Stimulants; Digitalis Toxicity; etc. Treatment Reduce stress; Reduce stimulants; Treat CHF; Beta-blockers Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Supraventricular Tachycardiac (SVT) Fast rhythms generated ‘Above the Ventricles’ Paroxysmal SVT (starts or ends suddenly) Rate – usually 130-250 Why? Stimulants; Infection; Electrolyte Imbalance MI Altered atrial pathway (WPW)-Kent S&S Lightheadedness; Palpitations; SOB; Anxiety; Weakness Dizziness; Chest Discomfort; Shock Treatment Vagal maneuvers; Adenosine 6 mg fast IVP; Repeat with 12 mg Adenosine; Cardioversion Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Atrial Flutter Irritable focus within the atrium typically fires at a rate of about 300 bpm Waveforms resemble teeth of a saw AV node cannot conduct faster than about 180 beats/minute Atrial vs ventricular rate expressed as a ratio Why: Re-entry- Hypoxia Pulmonary embolism MI Chronic Lung disease Pneumonia etc. S & S: SOB; Weakness; Dizziness; Fatigue; Chest discomfort Treatment: Ca Channel Blocker; Beta Blockers; Amiodarone; Cardioversion – anticoagulants; Corvert Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Atrial Fibrillation Irritable sites in atria fire at a rate of 400-600/minute Muscles of atria quiver rather than contract (fibrillate) No P waves – only an undulating line Only a few electrical impulses get through to the ventricles – may be a lot of impulses or a few A lot of impulses (ventricular rate high- then called atrial fibrillation with rapid ventricular response) A few impulses (ventricular rate slow – then called atrial fibrillation with slow ventricular response) Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG AV Block Delay or interruption in impulse conduction Classified accordi8ng to degree of block and/or to site of block First Degree Block Impulses from SA node to the ventricles is DELAYED but not blocked Why? Ischemia Medications Hyperkalemia o Inferior MI Treatment? Marian Williams RN Increased Vagal Tone Usually None ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Second Degree Block Type I - Wenckebach Lengthening of the PR interval and then QRS wave is dropped Why? Usually RCA occlusion (90% of population) Ischemia Increase in parasympathetic tome Medications Treatment If slow ventricular rate o Atropine o Pacing Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Second Degree AV Block – Mobitz Type II Why Ischemia LCA – Anterior MI Organic heart disease Important: Ventricular Rate QRS duration How many dropped QRS’s in relation to P waves? What is the ratio? Treatment Atropine Pacing Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Third Degree AV Block (Complete Block) No P waves are conducted to the ventricles The atrial pacemakers and ventricle pacemakers are firing independently Why? Inferior MI; Anterior MI Serious Treatment Atropine 0.5 mg IV Epinephrine 2-10 mcg/kg or Dopamine 2-10 mcg/kg/min Pacing Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Ventricular Rhythms Are the heart’s least efficient pacemakers Generate impulses at 20-40/min Assume pacemaking if: SA nodes fail, very slow (below 20-40) or are blocked Ventricles site(s) is irritable Marian Williams RN Irritable due to ischemia Depolarization route is abnormal and longer, therefore QRS looks different and is wider. T wave is opposite in direction to QRS ECG Premature Ventricular Contractions May be from One Site and all look the same Called Unifocal (from one focus or foci) Marian Williams RN ECG May be from Different sites (Foci) and are called Multifocal PVC’s Marian Williams RN ECG May occur every other beat – Ventricular Bigeminy Marian Williams RN ECG May occur every third beat – Ventricular Trigeminy Marian Williams RN ECG R on T PVC Marian Williams RN ECG Marian Williams RN ECG Couplets (2 PVC’s in a row); Triplets (3 PVC’s in a row) Marian Williams RN ECG Couplets also known as ‘Salvos’. Marian Williams RN ECG Run of PVC’s Marian Williams RN ECG Ventricular Tachycardia Defined as Three or more PVC’s occurring in a row at a rate > 100/min Wide QRS No P waves No T waves Why? Ischemia; Infarction; Congenital Usually lethal S & S: Weakness, Dizziness, Shock, Chest Pain; Syncope Treatment: Lidocaine or Amiodarone; Cardioversion –if pulse; Defibrillation – if no pulse (see Ventricular Fibrillation) Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Torsades de Pointes (Twisting of the Points) Ventricular Tachycardia in which the QRS changes in shape, amplitude and width Causes: Hypomagnesium; Hypokalemia; Quinidine therapy S & S: Altered mental status; shock; Chest pain; SOB; Hypotension Treatment: Magnesium Sulfate 2 Grams diluted in 20 cc D5W and given IV Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Ventricular Fibrillation Chaotic rhythm of the ventricles Lethal if not treated Causes: MI; Electrolyte Imbalance; Drug OD’s; Trauma Heart Failure; Vagal Stimulation; Increased SNS Electrocutions etc. Treatment: Defibrillation and CPR; AICD Defibrillation: 360 Joules (monophasic defibrillators) 150 Joules (biphasic defibrillators) Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG CPR 5 cycles (interrupt if defibrillator is there) Defibrillate Continue CPR for 5 cycles (2 minutes) Epinephrine 1 mg of 1:10,000 IVP OR Vasopressin 40 Units IV for 1st or 2nd dose of Epinephrine. Repeated every 3-5 minutes CHECK PT/Monitor CPR Shock CPR Amiodarone 300 mg IV or Lidocaine 1 mg/kg IV CHECK PT/Monitor Consider Magnesium Sulfate (Torsades) Marian Williams RN ECG Marian Williams RN ECG Marian Williams RN ECG Pulseless Electrical Activity – PEA Rhythm on monitor but no corresponding pulse Why? Look for Cause! H’s and T’s Hypoxia Hypovolemia Hydrogen Ion (acidosis) Hypo-Hyperkalemia Hypoglycemia Hypothermia Toxins Tamponade, cardiac Tension Pneumothorax Thrombosis (coronary or pulmonary) Trauma (Increased ICP, hypovolemia) ECG Pulseless Electrical Activity – PEA What do we do? CPR for 5 cycles Epinephrine 1 mg of 1:10,000 IVP OR may give Vasopressin 40 Units IV for 1st or 2nd dose of Epinephrine Give Epinephrine 1 mg of 1:10,000 IVP every 3-5 minutes If Rate is below 60/min. on monitor may give Atropine 1 mg IV up to 3 doses Always give a bolus of Normal Saline (1000 cc) Continue CPR Always check rhythm in 2 leads Check Patient ECG Marian Williams RN ECG Asystole No electrical activity on monitor No pulse Why? Look for Cause! H’s and T’s Hypoxia Hypovolemia Hydrogen Ion (acidosis) Hypo-Hyperkalemia Hypoglycemia Hypothermia Marian Williams RN Toxins Tamponade, cardiac Tension Pneumothorax Thrombosis (coronary or pulmonary) Trauma (Increased ICP, hypovolemia) ECG What do we do? CPR for 5 cycles Epinephrine 1 mg of 1:10,000 IVP OR may give Vasopressin 40 Units IV for 1st or 2nd dose of Epinephrine Give Epinephrine 1 mg of 1:10,000 IVP every 3-5 minutes If Rate is below 60/min. on monitor may give Atropine 1 mg IV up to 3 doses Always give a bolus of Normal Saline (1000 cc) Continue CPR Always check rhythm in 2 leads Check Patient Marian Williams RN ECG Marian Williams RN