Basic Nursing: Foundations of Skills and Concepts Chapter 24
advertisement

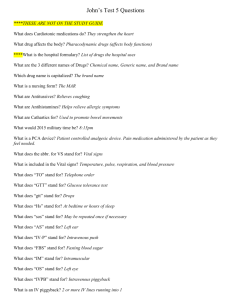
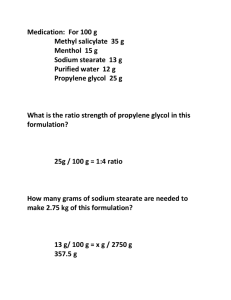
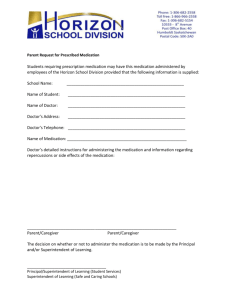
MEDICATION ADMINISTRATION Prepared by: Hikmet Qubeilat RN,MSc Medication or Drug is a chemical substance intended for use in the diagnosis, treatment, cure, mitigation, or prevention of a disease. When a drug is given to a client, there is an intended specific effect. An assumption made by nurses before administration of any medication is that the drug will be safe for the client to consume if the dose, frequency, and route are within the therapeutic range for that drug. Prescription: The written direction for the preparation and administration of a drug. Medication Names • Official name: name under which drug is listed in official government publications of drug standards( US Pharmacopeia). • Chemical name: name that describes the chemical composition of the drug. • Generic name: shortened name given to the drug by the developer; generic names are not capitalized before become official. • Brand name, trade name, or proprietary name: name given to and registered by the manufacturer The brand name is always capitalized and may have a trademark symbol (™ or ®) A drug has only one generic name but may have many trade names, depending on how many companies manufacture it Drug Action A drug’s ability to combine with a cellular drug receptor. Depending on the location of the cellular receptor, the drug can have a local effect, a systemic effect, or both. Medication Management Its purpose is to produce the desired drug action by maintaining a constant drug level. Drug action is based on the drug’s half-life (the time it takes the body to eliminate half of the blood concentration level of the original drug dose). Terms Relating to Drug Action Onset of action (the time it takes for the body to respond to a drug after administration). Peak plasma level (the highest blood concentration of a single drug dose before the elimination rate equals the rate of absorption). Plateau (maintenance of a certain level). The 4 Properties of Drug Action Absorption (passage of a drug from the site of administration into the bloodstream). Distribution (the movement of drugs from the blood into body fluids and tissues). Metabolism (the physical and chemical processing of a drug by the body). Excretion (the elimination of drugs from the body. Dissolution: is the rate at which a drug becomes a solution. After ingestion, a pill, capsule, or caplet must disintegrate before it can be dissolved and then absorbed by the body for therapeutic use. The more rapid the rate of dissolution, the more quickly the drug can be absorbed. Drug Interaction The effect one drug can have on another drug. Side Effects and Adverse Reactions Drug Allergy. Drug Tolerance. Toxic Effect. Idiosyncratic Reaction. Factors Influencing Drug Action Genetic factors. Age. Height. Weight. Physical conditions. Mental conditions. Medication Orders All medication orders should contain: Client’s name Date & Time Name of Drug to be administered Doasage Route of administration Time & frequency signature of person ordering Example: Ahmad Ali -------------12\3\2009----7pm (1) (2) Demerol 100 mg IM q 4 hrs (3) (4) (5) (6) Dr. Saeed Mohammed Types of Orders Stat (those that should be administered immediately). Single-Dose (one-time medications). Scheduled (administered routinely until order is canceled by another order). PRN (on as-needed basis). Examples of Medication Orders • Standing Example: Synthroid 0.1mg po qd • Standing PRN Example: Tylenol i or ii po q 4 hr for H/A • Short-series order Example: Prednisone 5 mg po tid x 3 days, then 5 mg bid x 2 days then 5 mg qd x 5 days Categories of Medication Orders, • One time Example: Demerol 50 mg IM @ 0800 in am • Stat Example: Valium 5 mg IV now Five “Rights” of Safe Drug Administration Right drug. Right dose. Right client. Right route. Right time. REALLY…THERE ARE 2 MORE! RIGHT TO KNOW – must explain each drug to patient RIGHT TO REFUSE – cannot make patient take meds Three Systems of Weight and Measure Metric (simple system based on units of 10). Apothecary (based on the weight of one grain of wheat). Household (drops, teaspoons, tablespoons, etc.). Metric System • Weight • Volume • Length gram (g) liter (L) meter (M) • Smaller and larger units in the metric system can be indicated by attaching prefixes to the basic units Kilo- is used to enlarge the basic unit 1000 times Metric System, continued • centi (cm) is used to diminish the basic unit by 100 • milli (mm), (mL), and (mg) diminishes the basic unit by 1000 • The symbol µ micro (micrometer or 0.001 millimeter) • The terms milliliter (ML) and cubic centimeter (CC) are used interchangeably Metric System, continued • The metric system uses the Arabic numerals that we all know, e.g., 1, 2, 3 • Abbreviations are placed after the number, as in 50 mg or 500 mL • Quantities less than 1 and fractions are written in decimal form as in 0.25 mg, 1.25 mg, and 1.5 g Basic Dimensional Analysis Review The doctor ordered Rocephin 750 mg IM x 1 dose. You have available a 5 mL vial labeled “Rocephin 1 gram/2.5 mL” How many mL will you administer? _________ We are looking for (calculating) mL The order is 750 mg Available concentration is 1 gram/2.5 mL (Conversion) 1 gram = 1000 mg (the question doesn’t tell us this; we have to know it) The 5 mL tells us the size of vial (Extra info) Basic Dimensional Analysis Review The doctor ordered Rocephin 750 mg IM x 1 dose. You have available a 5 mL vial labeled “Rocephin 1 gram/2.5 mL” How many mL will you administer? _________ 2.5 mL 1 gram 750 mg mL = ---------- X ------------ X ----------- = 1 gram 1000 mg Basic Dimensional Analysis Review 1st, reduce commons 3 2.5 mL 1 gram 750 mg mL = ---------- X ------------ X ----------- = 1 gram 1000 mg 4 Basic Dimensional Analysis Review 2nd, do the math (follow UAMS rounding rules) 3 2.5 mL 1 gram 750 mg 7.5 mL = ---------- X ------------ X ----------- = ------ = 1.875 = 1.9 1 gram 1000 mg 4 4 So, you would administer 1.9 mL mL/hr Calculation IVF: 1000 mL D5 ½ NS at 24 hour rate 1st, what are we looking for? We do have an infusion pump, so it is mL/hr. Infusion pumps always run in mL/hr!! Remember Total Volume Ordered mL ------ = hr to use UAMS rounding rules 1000 mL ------------ = 41.66666 = 42 mL/hr 24 hr Time to infuse total volume over mL/hr round to whole number mL/hr Calculation Now, what happens if the doctor orders an amount of fluid to run over minutes rather than 1 hour? Remember, the pumps are calibrated for mL/hr so you will need to plug the conversion for hours/minutes into your formula 60 min = 1 hour mL/hr Calculation The doctor orders 100 mL IVPB to infuse over 30 minutes. How many mL/hr do you set the pump? Total Volume to Infuse mL 100 mL 60 min ------ = ---------- X --------- = hr 30 min 1 hr Conversion factor Time to infuse total volume over mL/hr Calculation The doctor orders 100 mL IVPB to infuse over 30 minutes. How many mL/hr do you set the pump? 2 mL 100 mL 60 min 200 ------ = ---------- X --------- = ----- = 200 mL/hr 1 hr 30 min 1 hr 1 gtt/min Calculation You will use this formula when you don’t have a pump to infuse the ordered IV fluids!! You will have to locate the drop factor (found on the IV tubing package) Drop factor = how many drops does it take to equal 1 mL gtt/min Calculation Standard macrodrip calibration 10, 15, or 20 gtt/mL • Used for most adult IV sets Microdrip calibration set 60 gtt/mL • Used in pediatrics or critical medication drips Remember, the drop factor tells you how many drops needed to equal 1 mL gtt/min Calculation 1000 mL D5W with 40 mEq KCL is to infuse over 12 hours. The IV drop factor is 10 gtt/mL. How many drops per minute will be given? We calculate drops/minute because we don’t have a pump and it doesn’t make sense for the nurse to stand at the bedside and count drops for one hour; the nurse counts drops for 1 minute and then a second minute to verify that the correct drops are infusing to deliver the ordered amount over 1 hour gtt/min Calculation 1000 mL D5W with 40 mEq KCL is to infuse over 12 hours. The IV drop factor is 10 gtt/mL. How many drops per minute will be given? What we’re looking for Doctors Order Conversion Factor Remember, this is not in the question, we have to know it gtt 10 gtt 1000 mL 1 hr ----- = -------- X ------------ X ---------- = min 1 mL 12 hr 60 min 10 gtt/mL is the tubing that we have on hand gtt/min Calculation 1000 mL D5W with 40 mEq KCL is to infuse over 12 hours. The IV drop factor is 10 gtt/mL. How many drops per minute will be given? Use UAMS rounding 5 rules; round gtt/min to nearest whole number 100 gtt 10 gtt 1000 mL 1 hr 500 ----- = -------- X ------------ X ---------- = ------- = 13.888 = 14 min 1 mL 12 hr 60 min 36 6 6 gtt/min Calculation The doctor orders furosemide (Lasix) 20 mg in 50 mL of NS. Infusion time is 30 minutes. Drop factor is 60 gtt/mL. How many gtt/min will you give? What we’re looking for Doctors Order gtt 60 gtt 50 mL ----- = -------- X --------- = min 1 mL 30 min Note that the 20 mg dose doesn’t matter and we don’t need the hour/minute conversion factor 60 gtt/mL is the tubing that we have on hand gtt/min Calculation The doctor orders furosemide (Lasix) 20 mg in 50 mL of NS. Infusion time is 30 minutes. Drop factor is 60 gtt/mL. How many gtt/min will you give? 2 gtt 60 gtt 50 mL 100 ----- = -------- X --------- = ----- = 100 gtt/min min 1 mL 130 min 1 gtt/min Calculation 250 mL D5W is to infuse at 10 mL/hr. The IV drop factor is 60 drops per mL. How many drops per minute will this IV run? 1 gtt 60 gtt 10 mL 1 hr 10 ----- = -------- X -------- X --------- = ---- = 10 gtt/min min 1 mL 1 hr 60 min 1 1 mL/hr Calculation The doctor ordered 1000 mL D5NS to infuse over 8 hours. The drop factor is 15 drops per mL. How many mL/hr will the IV run? This is what the question ask us to calculate This is what the mL 1000 mL doctor ordered ---- = ------------ = 125 mL/hr hr 8 hr Note that we did not need the drop factor or hour/minute conversion Unit Calculation The doctor ordered Heparin 4000 units SQ. Available is Heparin 5000 units per mL. How many mL will the nurse administer? Use basic calculations to do this problem; Heparin is ordered in units but is available in mL, so we will calculate mL Note: you must spell 1 mL 4000 units mL = -------------- X ------------- = 5000 units out the word unit, it is no longer acceptable to use the abbreviation “u” Unit Calculation The doctor ordered Heparin 4000 units SQ. Available is Heparin 5000 units per mL. How many mL will the nurse administer? 4 1 mL 4000 units 4 mL = -------------- X ------------- = ----- = 0.8 mL 5000 units 5 5 What type of syringe will you use to administer the Heparin? Units—Heparin The doctor ordered Heparin 2000 units SC NOW. Pharmacy sends a vial labeled, Heparin 5000 units per mL. How many mL do you administer? 2 1 mL 2000 units 2 mL = -------------- X --------------- = ---- = 0.4 mL 5000 units 5 5 Units—Insulin Use Insulin syringes to administer insulin Do not use tuberculin syringes Insulin syringes 1 mL in size Some are ½ mL in size (if the dose of insulin is less than 50 units) • This makes it easier to see the small lines Calibrated in units (1 unit) = hundredths (0.01 mL) Marked U-100 • This means there are 100 units of insulin in each mL of the medicine Make sure that the bottle of insulin is also marked U-100 Insulin is available in a 10 mL vial That means there are 1000 units of insulin in the entire bottle Units—Insulin Note the large numbers (20, 30, 40 and so on) These represent units, not mL The doctor will order insulin doses in units, not mL The orange cap covers the You have to rotate the syringe to needle; the white cap on the its side to see the small lines. other end must be taken off in Each line represents “1 unit”. order to expose the plunger There are a total of 100 units or 1 mL in this syringe Unit Calculation You have Humulin -R insulin available in a bottle labeled U-100. The doctor orders Humulin-R insulin 16 units. How many units will you administer? 16 units, (that’s what the doctor ordered) Now, what if the question asked, how many mL will you administer? Unit Calculation You have Humulin -R insulin available in a bottle labeled U-100. The doctor orders Humulin-R insulin 16 units. How many mL less than 1 mL, round will you administer? to the nearest hundredth 1 mL 16 units 16 mL = ------------ X ----------- = ----- = 0.16 mL 100 units 100 Medication Forms Routes for Administering Medication •PO •Sub-ling - SL •Topical •Inhalants Oral Under the tongue Sprays, creams, suppositories Nebulizers Routes for Administering Medication Parenteral: Intramuscular (IM) Intravenous (IV) Subcutaneous (SQ) Intradermal (ID) Transdermal ROUTES ORAL OR PO DO NOT GIVE TO PATIENTS WHO: ARE VOMITING ARE COMATOSE LACK A GAG REFLEX ARE NPO HAVE FEEDING TUBES HAVE NG TUBES (UNLESS NG TUBE CAN BE CLAMPED) INTRADERMAL SITES USUALLY CHOSEN SO THAT LOCAL REACTION CAN BE OBSERVED… LIGHTLY PIGMENTED HAIRLESS USUALLY FOREARM THINK TB TESTING INTRAMUSCULAR INJECTIONS NO MORE THAN 4ml IN SINGLE INJECTION SITE (ADULT WITH WELL DEVELOPED MUSCLES) CHILDREN & ELDERLY – MAY LIMIT TO 1 – 2ml USUALLY 1&1/2 INCH, 21 TO 23 GAUGE NEEDLE Peripheral IV Access Hand veins Superficial dorsal Basilic Cephalic Arm veins Radial (wrist) Cephalic Basilic Median cubital Median Common IV Sites Metacarpal, cephalic, basilic, and median veins and their branches More distal sites should be used first, with more proximal sites used subsequently. Feet / leg sites require MD order Avoid arm on mastectomy side Selecting the Site Consider Condition of the vein Type of fluid or medication to be infused Duration of therapy Patient’s age and size Whether patient is left or right handed Patient’s medical history and current health status Skill of the person performing the venipuncture Selecting the Site Avoid areas • • • • • that are painful to palpation where the vein is hard or lumpy below an infiltrated IV site Veins too small for the selected IV catheter That interfere with ability to perform ADL’s Choosing the correct size catheter Smaller the gauge* (diameter) = less trauma Catheters that are too big invite complications Gauge must match the type of fluid to be administered * the larger the #, the smaller the diameter (gauge) Tips for Success Having difficulty finding a good vein? Apply warm moist soaks Apply warm towel or washcloth (DO NOT microwave) Let gravity help you! Have patient hang arm over side of bed. Patient Education Explain the procedure PRIOR to venipuncture Have patient report: Burning, bleeding, swelling at site IV dressing becomes wet or leaks Pump alarms Complications Infection Infiltration Phlebitis Fluid volume excess Bleeding IV Push and IV Bolus • IV Push: method of giving concentrated doses of medication directly into the vein( is administered over 1 to 5 minutes) • IV Bolus: concentrated dose of medication or fluid, frequently given intravenously • Admixture: The result of adding a medication to a container of intravenous fluid Speed Shock Rapid infusion of medication of fluid into the circulation causes toxic concentrations to accumulate Drugs can cause a shock-like syndrome Slower-than-ordered Infusion Rates Deprives the patient of fluids and medications Always check infusion rates against orders at beginning of shift, and after secondary infusions (I.e., antibiotics) to insure proper rate is maintained Blood Component Therapy Products Whole blood PRBCs / Washed PRBCs Plasma / FFP Platelets Cryoprecipitates Albumin Blood Administration – Nursing Responsibilities Knowledge of correct administration techniques Possible complications Agency polices & procedures Correct administration Patient / family education Blood Administration – Nursing Responsibilities Assessment Patient history • Reactions • # of pregnancies • Comorbidities • Culture, religion Physical assessment • Vital signs • Respiratory – auscultation • Cardiac – edema / HF symptoms Patient Education s/s transfusion reaction Risk of infection Frequency of Administration • Each hospital maintains a schedule of hours for administration of medications that is set up by the hospital nursing service • You are required to learn the hours that are standard for your hospital • Note: Standard prn orders are never assigned a time, because the drugs are administered as they are needed by the patient Qualifying Phrases • When a doctor wishes a drug to be administered only for specific conditions, a qualifying phrase will be part of the medication order • Not all orders contain qualifying phrases • Examples of commonly used phrases: For severe pain For stomach spasms For N/V While awake For insomnia The Importance of Monitoring The nurse must always carefully monitor client reactions to medications and ensure that clients are appropriately educated as to the actions, side effects, and contraindications of all medications they are receiving. Clients receiving IV therapy or blood transfusions require constant monitoring for complications. Responsibilities of Nurses Regarding Drug Administration Nurses are both legally and morally responsible for correct administration of medications.They must: Follow institutional policy. Consider clients’ desires and abilities. Foster compliance. Correctly document all actions related to medication administration and medication errors. BEHAVIORS TO AVOID DURING MEDICATION ADMINISTRATION DO NOT BE DISTRACTED DO NOT GIVE OR HOLD MEDS DISPENSED BY OTHERS DO NOT POUR FROM CONTAINERS WITHOUT LABELS OR DIFFICULT TO READ LABELS DO NOT GIVE EXPIRED DRUGS DO NOT GUESS ABOUT DOSAGES OR DRUGS DO NOT LEAVE BY THE BEDSIDE, OR UNATTENDED ANYWHERE DO NOT GIVE IF THE CLIENT STATES ALLERGIES OR HAS CONCERNS ABOUT THE DRUG DO NOT MIX WITH FOOD OR LIQUIDS IF CONTRAINDICATED YOUR RESPONSIBILITIES AS A STUDENT NURSE PROPER TECHNIQUE – SEE SYLLABUS RESEARCH – MUST LOOK UP ALL DRUGS PRIOR TO GIVING TO PATIENT SOURCES OF INFORMATION: DRUG HANDBOOK, DRUG CARDS, PHARM BOOK, MICROMEDIX (on hospital intranet) Documentation of Drug Administration A critical element of drug administration is documentation. The standard is “if it was not documented it was not done.” The nurse should document that a drug has been given after the client has received the drug. Never sign a medication out before you give it. Serious Medication Errors: EXAMPLES: Overdose Medication given to the wrong client Medication given via the wrong route Inform your supervisor Call the doctor as soon as possible. Strictly observe the client Document what happen, actions and interventions taken Remember a few important points: Always wash your hands before giving medication. NO ORDERS = DO NOT GIVE MEDICINE Medication is ALWAYS to be kept in a locked area.