PT Notes
advertisement
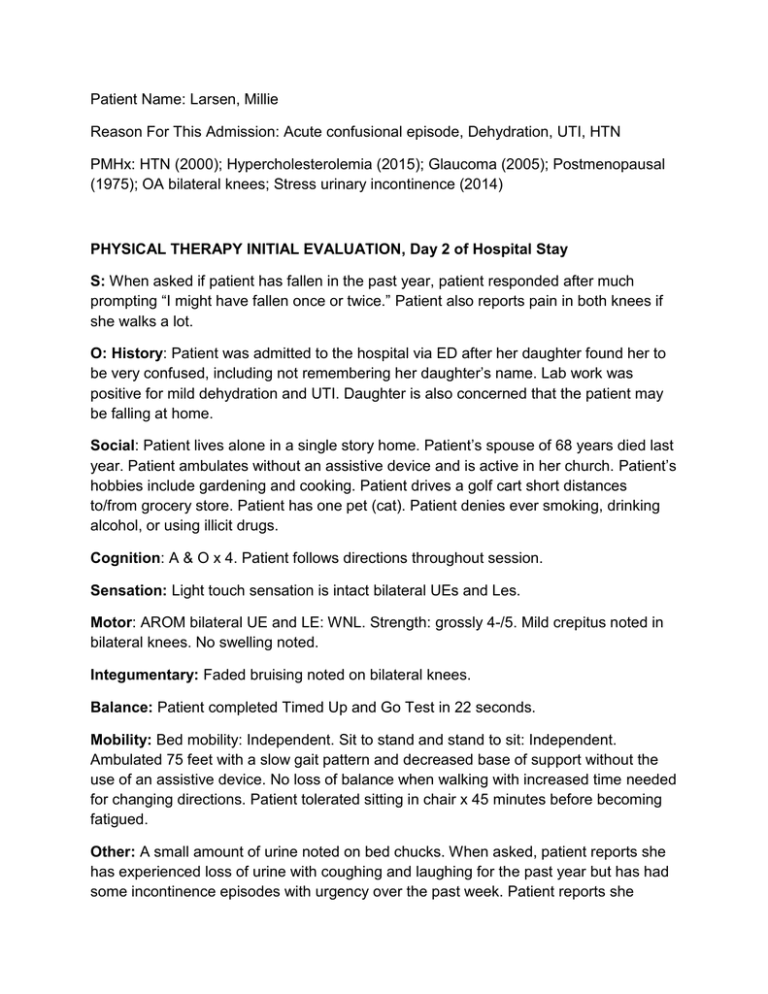
Patient Name: Larsen, Millie Reason For This Admission: Acute confusional episode, Dehydration, UTI, HTN PMHx: HTN (2000); Hypercholesterolemia (2015); Glaucoma (2005); Postmenopausal (1975); OA bilateral knees; Stress urinary incontinence (2014) PHYSICAL THERAPY INITIAL EVALUATION, Day 2 of Hospital Stay S: When asked if patient has fallen in the past year, patient responded after much prompting “I might have fallen once or twice.” Patient also reports pain in both knees if she walks a lot. O: History: Patient was admitted to the hospital via ED after her daughter found her to be very confused, including not remembering her daughter’s name. Lab work was positive for mild dehydration and UTI. Daughter is also concerned that the patient may be falling at home. Social: Patient lives alone in a single story home. Patient’s spouse of 68 years died last year. Patient ambulates without an assistive device and is active in her church. Patient’s hobbies include gardening and cooking. Patient drives a golf cart short distances to/from grocery store. Patient has one pet (cat). Patient denies ever smoking, drinking alcohol, or using illicit drugs. Cognition: A & O x 4. Patient follows directions throughout session. Sensation: Light touch sensation is intact bilateral UEs and Les. Motor: AROM bilateral UE and LE: WNL. Strength: grossly 4-/5. Mild crepitus noted in bilateral knees. No swelling noted. Integumentary: Faded bruising noted on bilateral knees. Balance: Patient completed Timed Up and Go Test in 22 seconds. Mobility: Bed mobility: Independent. Sit to stand and stand to sit: Independent. Ambulated 75 feet with a slow gait pattern and decreased base of support without the use of an assistive device. No loss of balance when walking with increased time needed for changing directions. Patient tolerated sitting in chair x 45 minutes before becoming fatigued. Other: A small amount of urine noted on bed chucks. When asked, patient reports she has experienced loss of urine with coughing and laughing for the past year but has had some incontinence episodes with urgency over the past week. Patient reports she remembers having a strong urge to urinate while in bed but didn’t realize she had leaked urine. Patient asked if there is anything she can do to stop leaking urine. A: Major impairments and activity limitations include: 1. 2. 3. 4. 5. Impaired balance. Reduced gait speed High risk for falls given past history of falls and TUG score of 22 seconds Decreased endurance Stress urinary incontinence x 1 year and more recent episodes of incontinence not associated with stress, which may be due to UTI. Goals: 1. Ambulate 150 feet with no rest breaks. 2. Ambulate 100 feet while frequently changing directions and negotiating obstacles without loss of balance with or without assistive device (TBD). 3. Tolerate sitting in bedside chair for at least 1 hour. 4. Increased LE strength by 1/4 grade to 4/5 for increased use in ADLs. 5. Completed Timed Up and Go Test in 14 seconds. P: Therapeutic exercise and gait training QD-BID x 2-3 days. Progress sitting tolerance and distance walked. Gait training with focus on balance, especially with turns and negotiating obstacles. Patient and family education on reducing fall risks in the home. Will also assess whether patient would benefit from an assistive device. Discharge planning to include possible home health to decrease fall risk at home. Patient may also benefit from outpatient pelvic floor physical therapy to address urinary incontinence. Marilyn Schwarz, PT, DPT Progress Note, Day 3 of hospital stay S: “I don’t want to use a cane or walker. I don’t fall that much and when I do, I always catch myself and don’t get hurt.” Patient reports she has not had any urinary incontinence episodes today. O: Patient went from supine to sitting edge of bed independently. Patient educated on stress urinary incontinence and how strengthening the pelvic floor muscles can improve continence. Performed pelvic floor awareness exercises to help patient identify pelvic floor muscles. Patient instructed to contract these muscles before coughing and laughing (aka “The Knack”) to decrease leakage. Patient transitioned from sit to stand independently. Patient shown how to use a largel base quad cane. Patient initially reluctant to use cane; however once patient was told it may help her knees feel better, patient agreed to try using the cane. Patient ambulated 175 feet without using an assistive device and once using large base quad cane. No loss of balance noted either time. Patient ambulated faster with cane. Patient performed seated lower extremity strengthening exercises, including glut sets, quad sets, hip flexion, knee extension, and ankle pumps, 10x/set, 1 set each. After treatment, patient tolerated sitting up in chair for lunch x 60 minutes. A: Patient did well with identifying pelvic floor muscles and contracting. Patient also ambulates with a faster gait using a large base quad cane, though patient reports she does not know whether she wants a cane for home. P: Continue gait training, pelvic floor exercises, balance activities, and lower extremity strengthening exercises QD-BID. Will reassess assistive device needs. Marilyn Schwarz, PT, DPT Progress Note, Day 4 of hospital stay (Discharge Day) S: Patient reports performing The Knack helps her leak less urine with coughing. Patient states she no longer leaks urine in bed, leakage now only happens with coughing and laughing. At beginning of session patient reported she does not want a cane to take home but by end of session patient agrees to using a large base quad cane. O: Patient went from supine to sitting edge of bed independently. Patient educated on contracting the pelvic floor muscles slowly (hold 5 seconds) and quickly (hold 2 seconds) to strengthen the pelvic floor. Patient instructed to perform exercises while in bed and when sitting up in chair 10x/set, 3x/day. Patient transitioned from sit to stand independently. Gait training focused on higher level balance activities, including stepping over small objects, turning corners quickly, and walking backwards. Patient was unsteady and loss of balance x 1 with PT needed to prevent fall. Discussed fall risk and what happens when people fracture their hip. Patient performed same balance challenges with a large base quad cane and no loss of balance noted. Patient completed Timed Up and Go Test in 16 seconds without an assistive device. After treatment, patient tolerated sitting up in chair for lunch x 75 minutes. A: Patient did well with identifying pelvic floor muscles and contracting. Patient would benefit from using a large base quad cane. Patient was much steadier when ambulating using the cane when her balance was challenged. P: Recommend patient is discharged home with large base quad cane and home health PT to assess the home environment and mitigate fall risks. Once patient is discharged from home health physical therapy, if patient is still having urinary incontinence episodes, recommend patient to see outpatient pelvic floor physical therapist to address further treatment for urinary incontinence. Marilyn Schwarz, PT, DPT