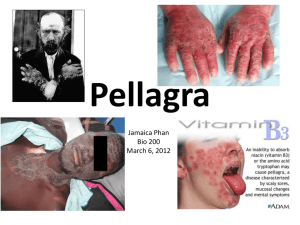
Vitamin B3 Niacin
advertisement

Vitamin B3 Niacin History • The term niacin (vitamin B3) is considered a generic term for nicotinic acid and nicotinamide (also called niacinamide). • The vitamin was once called the anti–black tongue factor because of its effect in dogs. • Pellagra was especially prevalent in the Southern United States where corn (which contains a relatively unavailable form of niacin) was a main dietary staple in the early 1900s. • In 1937 Elvehjem isolated the vitamin, which was shown then to cure both pellagra and black tongue. Niacin (nicotinamide) Vitamin B3 • The vitamin activity of niacin is provided by both nicotinic acid and nicotinamide. • Structurally, nicotinic acid is pyridine 3carboxylic acid, whereas nicotinamide is nicotinic acid amide. Sources • The best sources of niacin include: fish such as tuna and halibut, and meats such as beef, chicken, turkey, among others. Enriched cereals and bread products, whole grains, fortified cereals, seeds, and legumes. • Contain appreciable amounts of niacin in coffee and tea. • lesser amounts in green vegetables and milk. • In supplements, niacin is generally found as nicotinamide (niacinamide). Sources • In animals, niacin occurs mainly as nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP). • But, after slighting of animals, NAD and NADP are thought to undergo hydrolysis; thus, meats provide niacin as free nicotinamide. • In their oxidized forms, NAD and NADP possess a positive charge and therefore may alternatively be written NAD+ and NADP+. Sources DIGESTION, ABSORPTION, TRANSPORT, AND STORAGE • NAD and NADP may be hydrolyzed within the intestinal tract or enterocyte by glycohydrolase to release free nicotinamide. Glycohydrolase • NAD & NADP Nicotinamide • Nicotinamide and nicotinic acid can be absorbed in the stomach, but they are more readily absorbed in the small intestine DIGESTION, ABSORPTION, TRANSPORT, AND STORAGE • In the small intestine, if niacin concentrations is low, its absorbed by sodium-dependent, carrier-mediated (facilitated) diffusion. • At high concentrations (as with 3–4 g pharmacological doses), niacin is absorbed almost completely by passive diffusion. • In the plasma, niacin is found primarily as nicotinamide, with little nicotinic acid. Up to ~1/3 of plasma nicotinic acid is bound to proteins. • Nicotinamide and nicotinic acid move across cell membranes by simple diffusion. • Then, nicotinic acid transport into the kidney tubules and red blood cells requires a carrier. DIGESTION, ABSORPTION, TRANSPORT, AND STORAGE • Nicotinamide is primary precursor of NAD in all tissues. • Nicotinic acid may be used to synthesize NAD in the liver which influenced by various hormones. • Vitamin is trapped within the cell as NAD or NADP. • Intracellular concentrations of NAD typically predominate over those of NADP. DIGESTION, ABSORPTION, TRANSPORT, AND STORAGE • In the liver, excess niacin and tryptophan are converted to NAD and stored in small amounts not bound to enzymes. • NAD may be degraded to yield nicotinamide, which then is available for transport to other tissues. • NAD is found primarily in its oxidized form (NAD+), whereas NADP is found in cells mainly in its reduced form (NADPH). FUNCTIONS AND MECHANISMS OF ACTION • Approximately 200 enzymes, primarily dehydrogenases, require the coenzymes NAD and NADP, which act as a hydrogen donor or electron acceptor. • Niacin functions as a substrate in nonredox roles as a donor of adenosine diphosphate ribose (ADP-ribose). FUNCTIONS AND MECHANISMS OF ACTION Coenzymes • NAD and NADP are very similar and undergo reversible reduction in the same way, their functions in the cell are quite different. • The major role of NADH is to transfer its electrons from metabolic intermediates through the electron transport chain thereby producing adenosine triphosphate (ATP). • NADPH: acts as a reducing agent in many biosynthetic pathways such as (fatty acid, cholesterol, and steroid hormone synthesis). FUNCTIONS AND MECHANISMS OF ACTION Coenzymes • NAD and NADP are tightly bound to their apoenzymes and can easily transport hydrogen atoms from one part of the cell to another. • These reactions occur in the mitochondria and in the cytoplasm. FUNCTIONS AND MECHANISMS OF ACTION Coenzymes • Oxidative reactions in which NAD participates and is reduced to NADH include: • Glycolysis • oxidative decarboxylation of pyruvate • oxidation of acetyl CoA in the TCA cycle • β-oxidation of fatty acids • oxidation of ethanol • NAD is required for catabolism of vitamin B6 as pyridoxal to its excretory product, pyridoxic acid. FUNCTIONS AND MECHANISMS OF ACTION Coenzymes • NADPH is generated from NADP by reduction which occurs as part of the hexose monophosphate shunt by the mitochondrial. • The NADPH producedin is used in some reductive biosynthesis: • fatty acid synthesis • cholesterol and steroid hormone synthesis • oxidation of glutamate • synthesis of deoxyribonucleotides (precursors of DNA) • regeneration of glutathione, vitamin C, and thioredoxin • conversion of folate to active forms, dihydrofolate (DHF) and tetrahydrofolate (THF) and synthesis of 5-methyl THF and 5,10methylene THF. METABOLISM AND EXCRETION • NAD, generated from nicotinamide or produced in the liver from tryptophan, and NADP can be degraded by glycohydrolase into nicotinamide and ADP-ribose. • The released nicotinamide is methylated and is then oxidized in the liver into a variety of products that are excreted in the urine. • Typically, little nicotinic acid or nicotinamide is excreted, because both compounds may be actively reabsorbed from glomerular filtrate. METABOLISM AND EXCRETION • The primary metabolites of nicotinamide are: • N' methyl nicotinamide (~20% to 30% of niacin metabolites). • N' methyl 2-pyridone 5-carboxamide (~40% to 60%). • N' methyl 4-pyridone carboxamide (4-pyridone) in small amounts. • Nicotinic acid is metabolized mainly to N‘ methylnicotinic acid. RDA’s • Recommendations for niacin intake include calculations of niacin derived from the amino acid tryptophan (about 60 mg of tryptophan thought to generate 1 mg of niacin). • Total niacin thus is provided to the body as nicotinic acid and nicotinamide and from 1/60 mg of tryptophan. • The term niacin equivalent (NE) is used to account for the provision by tryptophan. • Assuming that: • 1 g of high- quality protein in diet = 10 mg of tryptophan. • Intake 60 g complete protein = 600mg tryptophan. • 60mg tryptophan /1mg of NE • 60g protein = 10 NEs RDA’s • • • • • The RDA’s for niacin (as niacin equivalents) 14 mg/day for women 16 mg/day for men 18 mg/day for pregnancy 17 mg/day for lactation DEFICIENCY: PELLAGRA • Pellagra is a serious deficiency of niacin. • Pellagra can easily remembered as the four Ds— dermatitis, dementia, diarrhea, and death—are often used as a mnemonic device for remembering. • The dermatitis sunburn in face and neck then in hands, wrists, elbows, knees, and feet. • Neurological: headache, loss of memory, peripheral neuritis and dementia or delirium. • Gastrointestinal: glossitis, stomatitis, nausea, vomiting, and diarrhea or constipation. • If untreated, death occurs. Pellagra TOXICITY • Large doses of nicotinic acid (up to 6 g/day in divided doses) are used to treat hypercholesterolemia (high blood cholesterol). • These pharmacological doses: • significantly lower total serum cholesterol, triglycerides, and low-density lipoproteins (LDLs) and increase high-density lipoproteins (HDLs). • Inhibits lipolysis in adipose tissue and decreases hepatic VLDL secretion from the liver and LDL production. • Diminish triglyceride synthesis and increases HDL in liver. TOXICITY • These dose of vitamin has some undesirable side effects, especially in doses of 1 g or more per day. • Vasodilatory effects: including uncomfortable flushing and redness alongnwith burning, itching (pruritus), tingling, and headaches • gastrointestinal problems such as heartburn, nausea, and possibly vomiting. • liver injury (hepatic toxicity) elevated hepatic enzymes, jaundice, hepatitis and liver failure. • Hyperuricemia (raising serum uric acid levels). • Elevation of plasma glucose concentrations (i.e., glucose • intolerance).