Case Presentation
advertisement

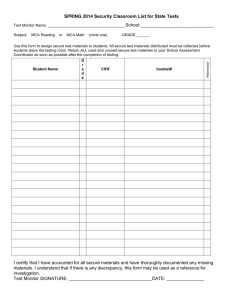
Complex issues in dementia for adults with learning disability; breaking bad news, capacity and best interest decisions. Natasha Patel, CT3 Samantha Riches, principal clinical psychologist Ba Min Ko, ST5 Lambeth MHLD RCP/BPS Dementia Guidance Epidemiology: • People with intellectual disabilities have a higher risk of developing dementia compared to the general population, with a significantly increased risk for people with Down’s syndrome and at a much earlier age. • Life expectancy of people with Down’s syndrome has increased significantly and the number of older people with Down’s syndrome has been increasing. • The incidence and prevalence of Down’s syndrome is relatively stable. Dementia Prevalence by age Prospective assessments – should we or shouldn’t we? • The evidence does not currently indicate a need for prospective screening for people with intellectual disabilities without Down’s syndrome. • Screening for people with Down’s syndrome needs to be justified in terms of likely gain, the demands placed on the service, and there needs to be consideration of the issue of informed consent. • Some services may decide against it for reasons of intrusion, commissioning intentions and/or resource limitations. • Apparent changes in scores on cognitive assessments do not in themselves indicate dementia but do require further investigation. Background • • • • • 48 year old Down’s syndrome and mild LD Supported accommodation Parents deceased, 2 sisters, 1 brother First referred in 2008 to OT personal safety group • Referred in 2010, support workers concerned about short term memory Past psychiatric and medical history • 1999 – forgetful, referred to psychiatry, diagnosed depression. Resolved without treatment • Neutropenia • Gout Initial assessment • From Wayne – unsure why referred, reported forgetting to put watch on or take glasses out • Support worker – 6-8/12 hx of forgetfulness, slower walking, disorientated. Presentation fluctuates • Sister - slowed up in his cognitive processing and motor skills in the last 6-8 months, quieter Initial assessment • • • • MSE – unremarkable No significant physical health concerns Bloods – neutropenia ? Cause MRI head/neurology review - previous significant hypoperfusion • No medication, NKDA • DLD - cognitive scores: 24 (problems reported in ST and LT memory, orientation. ocial scores: 9. • DSQuid – 16 Local Dementia Protocols • • • • Borough specific pathways – GSTT/SLaM Regular Dementia pathway meetings Dementia case coordination Provider training: – Estia – Bespoke Assessment Process • • • • ‘Trigger’ questions – aim for multi-disciplinary Consider NTG-EDSD (vs. DSQIID) Physical health checks Baseline Direct & indirect assessment: – Psychology – CAMDEX-DS – OT – AMPS • Discussion at Dementia pathway meetings • Timescale for follow ups agreed • Clinical psychologist &/or psychiatrist, plus key disciplines involved, review MDT assessments and arrive at diagnosis. National Task Group – Early Detection Screen for Dementia See http://aadmd.org/ntg/screening Other possible reasons for cognitive decline • The common differential diagnoses for individuals with Down’s syndrome presenting with loss of skills are depressive illness, sensory impairments (hearing or visual), hypothyroidism, obstructive sleep apnoea and dementia. • Sometimes conditions can co-exist. • Do not forget about the following causes of apparent functional decline as these are often missed: – iatrogenic causes of cognitive impairment particularly when the individual is taking multiple medications, – impact of the environment particularly in relation to occupational deprivation and under stimulation, – impact of abuse on the individuals with ID. Wider role psychiatry / CPN • Rule out mental health issues • Confirm final diagnosis to GP & recommend medication • Review medication as required • Psychiatrists are often the professional who make the diagnosis explicit to the family/carers Follow-up • 6/12 follow-up • Remained stable until Feb 2014 – Slower in speech and movement – More forgetful – Behavioural changes: aggressive towards other residents – Deterioration in all areas of CAMDEX-DS • Diagnosis of Alzheimer's dementia made • Recommended Donepezil • WB assessed to not have capacity Follow-up • Oct 2014 started donepezil 5mg OD • Dec 2014 dose increased to 10mg OD, no SE’s reported • Feb 2015 no deterioration in cognitive function, no SE’s. – Sister keen to stop as no improvement – Feels causing depression, no affective symptoms on review – Agreed to continue but not increase for further 3/12 then stop if no improvement • Medication stopped May 2015, discharged. Breaking the news (from RCP/BPS guidance) • People with intellectual disabilities, their families and carers need to be given opportunities to understand the nature of the intellectual disability and information about any associated health risks from an early point in their life and particularly from transition to adulthood onwards. • People with intellectual disabilities need to be told about their diagnosis of dementia and given ongoing opportunities to understand their diagnosis and their experience of dementia. • Family members and carers need to be informed about the diagnosis and involved as much as possible in support and management plans and, as appropriate, be given opportunities for education and training. • The person’s peers and friends are also important people to involve in giving information about the diagnosis and this will both help them cope and help them support the person affected by dementia. • People with intellectual disabilities and their families and carers may need psychological interventions to enable them to feel emotionally supported and to begin to understand the diagnosis. Recent experience in Lambeth • Family members / carers disagreeing with results of assessment • Concerns regarding medication side effects • Worries about ‘best interest’ process Mental Capacity Act A turning point in the statutory rights of people who may lack capacity. Lack of capacity may be because of LD, ASD, senile dementia, brain injury or temporary impairment. How was it developed? It was quite a lengthy process – long process of consultation 1989 - the law commission undertook a study – decision making on behalf of people who lacks capacity. 1995 – recommended there should be a single comprehensive piece of legislation making provisions for people who lack capacity 1997 – Green Paper 1999 – White Paper June 2003 – Draft Mental Incapacity Bill November 2003 - Pre-legislative scrutiny – widespread support June 2004 – MCA Bill introduced 2005 – In practice The five principles of the Mental Capacity Act 1) Presumption of capacity 2) Attempt all practical steps to help the patient understands 3) Unwise decision does not mean lack of capacity 4) Best interest 5) Least restrictive MCA assessment 1) UNDERSTAND – pros and cons of decision in question 2) RETAIN – information for a reasonable length of time 3) WEIGH – all the information given 4) COMMUNICATE – the decision Understanding the patient’s safety issues for people with ID National safety agency, 2004 Informed consents were not taken properly Consents were being sought from a carer rather than taking time to gain consent from people with ID Death by Indifference; MCA 2007 Look into the death of 6 cases of ID Areas to be improved which include MCA Made a number of recommendations - There should be more training for NHS staff around the MCA One of 6 Cases EM – severe ID + challenging behaviour + very poor communication Died of cancer at the age of 26 Hospital delayed treatment – as she would not cooperate with the treatment – could not consent to treatment In pain all the time Repeated attendance to hospital Mother gave notice to the team via solicitor Took them to High Court – only then treatment started One of 6 cases Very detrimental and distressing to the patient and family This distressing experience could have been avoided or reduced if the professional had a better understanding and appropriate use of MCA Six Lives; Progress Report on Healthcare for people with ID, July 2013 - DOH After the inquiry into the death of the six patients with ID, DOH monitored the progress of the recommendations which included MCA Reported in 2009, 2010, 2013 Doing well – People in the hospitals do what the law says in the MCA. Involving people with LD and their families/carers. Not doing well – People with LD are not given information in a way they can understand. People are not included in decision about their care. The Mencap survey showed that some of the recommendations were better. People were being asked to make decisions when they are able to. But this did not always happen. A Population based Study: The Confidential Inquiry into Premature Death of people with ID in UK – Dec, 2013 Causes of death are avoidable Amenable to change with good quality of care More common in people with ID than general population Contributory factors – problems in Advanced care planning Adherence to MCA Living in inappropriate accommodations Adjustment of care as needs changed and carers feeling not listened to Consistent pattern in the findings A Population based Study: The Confidential Inquiry into Premature Death of people with ID in UK – Dec, 2013 A number of Recommendations MCA advice – needs to be easily available 24 hr a day. MCA training and regular updates - to be made mandatory for staff involved in the delivery of health or social care. Post-legislative Scrutiny on MCA (2005)– 2013 - 2014 House of Parliament established a committee in May 2013 Whether the act is working as the Parliament intended 15 Public evidence hearings with 61 witnesses A large number of written submissions – 216 written evidence, 206 were accepted Delegation of the committee met adults with ID Attended a special meeting of (Forget-Me-Not, a peer support and advocacy group for people with dementia in East Kent) Visited Court of Protection Results The implementation of MCA has not met the expectation. Lack of adherence to different levels or stages of MCA. Lack of awareness Lack of understanding Lots of people and services do not follow it. Many services think people can’t make decisions when they can. They do not check to see if someone can make a decision. The checks that are done are not very good People do not get support to make their own decisions. Health services still think they know best for people they think cannot make their own decisions Complex issues… • Breaking bad news… • Do we talk to service users ourselves? Expect families or carers to do so? • Capacity to consent to treatment • Best interest decisions about care • What if we don’t all agree?!