Impetigo - De Anza College
advertisement

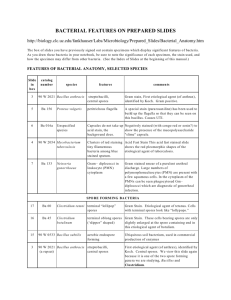
4-c The Bacteria And various pages in additional chapters Relationships Between Bacteria and Clinical Features of Disease 1 Structure/Function Relationships Differences exist between human (eukaryotic) and bacterial (prokaryotic) cells Many of the differences account for disease pathogenesis And, allow exploitation of the differences to develop chemotherapy (antibiotics) 2 Differences Accounting for Pathogenesis Structure Pathogenesis Capsule • K-antigen • All pathogens that cause pneumonia & meningitis have capsules • Haemophilus influenzae, Neisseria meningitidis, Escherichia coli, Streptococcus pneumoniae, Klebsiella pneumoniae, group B streptococci Plasmids • Antibiotic resistance (R-factor) Outer membrane (Gram negative) • Endotoxin (Lipid A) • O-antigens Flagella • H antigen, virulence factor • Attachment to cells Fimbriae • Attachment to cells Pili • Spread of AB resistance genes 3 Toxins Poisonous substances produced by microbes – Transported in blood – Produce fever, cardiovascular disturbances, diarrhea, shock – Inhibit protein synthesis, destroy blood cells & vessels, disrupt nervous system 4 Two Types Exotoxin Endotoxin Gram positive Product of cell Protein Affects cell functions Gram negative Part of LPS Lipid portion (Lipid A) Fever, weakness, aches, shock High toxicity Lethal dose small Gas gangrene, tetanus, botulism, scarlet fever Low toxicity Lethal dose larger Typhoid fever, UTI, meningococcal meningitis 5 Alcaligenes faecalis Enterobacter aerogenes Proteus Azotobacter Enterobacter sakazaki Proteus vulgaris Bacillus Enterobacteriaceae Pseudomonas aeruginosa Bacillus anthracis Escherichia Salmonella Bacillus cereus Escherichia coli Salmonella typhimurium Bacillus megaterium Gram negative Serratia marcescens Bacillus subtilis Gram positive Shigella dysenteriae Borrelia burgdorferi Klebsiella Spirillum Clostridium Klebsiella pneumonia Staphylococcus Clostridium botulinum Lactobacillus plantarum Staphylococcus aureus Clostridium perfringens Micrococcus luteus Staphylococcus epidermidis Clostridium sporogenes Mycobacteria Streptococcus Clostridium tetani Mycobacterium leprae Streptococci mutans Corynebacterium diphtheria Mycobacterium smegmatis Streptococci pneumoniae Corynebacterium xerosis Mycobacterium tuberculosis Streptococcus viridans Enterobacter Neisseria gonorrhoea Treponema pallidum Nocardia Vibrio cholera 6 Alcaligenes faecalis Enterobacter aerogenes Proteus Azotobacter Enterobacter sakazaki Proteus vulgaris Bacillus Enterobacteriaceae Pseudomonas aeruginosa Bacillus anthracis Escherichia Salmonella Bacillus cereus Escherichia coli Salmonella typhimurium Bacillus megaterium Gram negative Serratia marcescens Bacillus subtilis Gram positive Shigella dysenteriae Borrelia burgdorferi Klebsiella Spirillum Clostridium Klebsiella pneumonia Staphylococcus Clostridium botulinum Lactobacillus plantarum Staphylococcus aureus Clostridium perfringens Micrococcus luteus Staphylococcus epidermidis Clostridium sporogenes Mycobacteria Streptococcus Clostridium tetani Mycobacterium leprae Streptococci mutans Corynebacterium diphtheria Mycobacterium smegmatis Streptococci pneumoniae Corynebacterium xerosis Mycobacterium tuberculosis Streptococcus viridans Enterobacter Neisseria gonorrhoea Treponema pallidum Nocardia Vibrio cholera 7 Bacilli, rods Cocci Bacillus anthracis Neisseria gonorrhoea Clostridium botulinum Staphylococcus aureus Clostridium perfringens Streptococci mutans Clostridium tetani Streptococci pneumoniae Corynebacterium diphtheria Escherichia coli Curved Vibrio cholera Klebsiella pneumonia Mycobacterium leprae Spirochete Mycobacterium tuberculosis Borrelia burgdorferi Treponema pallidum 8 Clinically Significant Bacteria Arrangement: rods, bacilli – Bacillus – Clostridium – Corynebacterium – Escherichia coli – Mycobacterium 9 Bacillus anthracis • Gram positive, rods • Spore forming • Aerobe or facultative • Found in soil Disease: • Anthrax – Pulmonary – Cutaneous – GI • Biological warfare – Ch 23, p 680-1 Fig. 11.17b Bacillus germinating 1) 2) 3) 4) 5) Ch / Pg 3 / 71 4 / 96-97 11 / 331 23 / 679-681, 702 LM / 18-9 10 Cutaneous Anthrax • Contact with material containing anthrax endospores • Results in skin lesion covered by a black scab Fig. 4.21 Endospore • Diagnosis – New blood test detection Fig. 23.7 Anthrax lesion 11 Clostridium • Gram positive, rods • Obligate anaerobe • Endospores • Widely found in soil, GI tracts human, animals • Toxins (neuro) Diseases: • Botulism • Tetanus • Gas gangrene • Food borne diarrhea Fig. 23.8 gangrene Ch / Pg 1) 11 / 330 2) 23 / 681-2, 702 3) 15 / 459-464 4) LM / 18-20 12 Gas Gangrene • C. perfringens • If wound is brand new – Prompt cleaning of serious wounds – Antibiotic treatment (penicillin) • Wound is seriously necrotic Fig. 23.9 Hyperbaric chamber – Surgery, amputation 13 Corynebacterium diphtheriae • Gram positive • Club-shaped, pleomorphic • Aerobic or (facultative anaerobic) • Non-spore forming • Toxin (cyto) • Metachromatic granules – Volutin Fig. 24.5 Corynebacterium Disease: • Diphtheria Ch / Pg 1) 2) 3) 11 / 335 24 / 715-6, 718 LM / 24-25 14 Diphtheria • Airborne transmission • Forms a leathery, grayish membrane in the throat – Sore throat, fever, general malaise, swelling of neck • Diagnosis: – Selective & differential media Part of the DPT immunizations for children Fig. 24.6 Diphtheria membrane 15 Escherichia coli • Gram negative, rods • Facultative anaerobe • Toxins - Invasive - Hemorrhagic - Plasmid borne Fig. 4.11 E. coli Diseases: • Foodborne epidemics • Urinary tract infections (‘travelers diarrhea’) Ch / Pg • Gastroenteritis 1) 4 / 83 – E. coli O157:H7 2) 11 / 323 3) 25 / 758-9 16 Gastroenteritis • E. coli (EHEC) • Hemorrhagic colitis (very bloody stools) • Adhere to intestinal mucosa, destroy microvilli • Serotype: O157:H7 • Infective dose 100 bacteria • Diagnosis: rapid methods Fig. 24.6 Enterohemorrhagic E. coli 17 Mycobacterium • Acid fast, slender rod • Obligate aerobe • Non-spore forming Disease: • Tuberculosis • Leprosy (Hanson’s Disease) 1) Mycobacterium tuberculosis 2) M. leprae Fig. 24.9 Mycobacterium Ch / Pg 1) 3 / 70-1 2) 11 / 334-5 3) 22 / 651-2, 665 4) 24 / 719-723 5) LM / 21-22 18 Tuberculosis • Inhale the bacillus – Lodge in the lung alveoli – Can progress to a lung damaging inflammation Fig. 24.2 Lower Respiratory System • Diagnosis: – TB skin test – Sputum smears – Chest X ray, CT Fig. 24.11 TB skin test 19 Leprosy • Invades myelin sheath, peripheral nervous system – Cause nerve damage – 12 day generation time – Never grown in culture • Necrosis of tissue • Diagnosis: – Detect acid-fast rods in patient fluids – Lepromin test Fig. 22.9 Leprosy Also called Hansen’s disease 20 Clinically Significant Bacteria Arrangement: cocci – Neisseria gonorrhoea – Staphylococcus aureus – Streptococci 21 Neisseria gonorrhoea • Gram negative • Diplococcus • Obligate aerobe • Non-spore forming Disease: • STD: Gonorrhea • Meningitis Fig. 22.4 Neisseria meningitis, pharynx Ch / Pg 1) 22 / 645-6 2) 26 / 790-793 22 Gonorrhea • Attaches via fimbriae • Leads to inflammation • Leucocytes move to infected area – Characteristic pus forms • In women, only the cervix is infected • Diagnosis: Fig. 26.7 A smear of pus, patient with gonorrhea – Stained pus smears 23 Staphylococcus aureus • Gram positive, cocci • Grape-like clusters • Facultative anaerobe • Toxin Diseases (many): • Surgical wounds (nosocomial) • TSS (toxic shock syndrome) • Skin infections (impetigo, scalded skin) • Endocarditis Fig. 11.18 Staphylococcus aureus Ch / Pg 1) 11 / 332 2) 21 / 615-20, 633 3) 23 / 674-5 24 4) 25 / 751 Acute Bacterial Endocarditis • Gain access to bloodstream • Leads to infection – Forms fibrin-platelet vegetations • Rapid destruction of heart valves within the endocardium • Diagnosis: Fig. 23.4 Bacterial endocarditis – Echocardiogram 25 Clinical Ramifications, 2 types • S. aureus and S. epidermidis can be divided into 2 groups • Slime layer allows S. epidermidis to colonize catheters Fig. 21.3a, b. Coagulase negative staphylococci Staphylococcus aureus Staphylococcus epidermidis Coagulase positive Coagulase negative Produces enterotoxins Produces slime layer Damage tissue Adhere to surfaces 26 Streptococcus • Gram positive, cocci, chains • Facultative anaerobe • alpha, beta, gamma hemolytic • Secrete toxins Diseases (many): • • • • • Pneumonia Strep throat Scarlet fever Skin infections Rheumatic fever Fig. 11.19 Streptococcus Ch / Pg 1) 11 / 333 2) 14 / 427 3) 21 / 620-1 4) 23 / 674-6 5) 25 / 751 27 Skin Infection - Erysipelas • Most important bhemolytic species – S. pyogenes • Reddish patches on skin - dermal layer – Tissue destruction – Pus generated – Enter bloodstream cause sepsis Fig. 21.6 Lesion of erysipelas 28 Q’s What is seen at the ends of the cells of Clostridium tetani in this micrograph? 1. 2. 3. 4. 5. Very thick flagella Endospores The cells are undergoing division These cells are pleomorphic, accounting for this shaped cell Budding cells 29 Q’s 1. Which of these is NOT correctly matched? 1. 2. 3. 4. Escherichia coli – gastroenteritis Staphylococcus aureus – TSS Clostridia tetani – gangrene Bacillus anthracis – anthrax 2. Which of following is not true about fimbriae? 1. 2. 3. 4. 5. They are composed of protein They may be used for attachment They are composed of pilin They may be used for motility They are found on Gram negative cells 30 Q’s 1. The formation of a tough grayish membrane in the throat is characteristic of: 1. 2. 3. 4. Tuberculosis Scarlet fever Diphtheria Streptococcal pharyngitis 2. A positive tuberculin skin test indicates that an individual: 1. 2. 3. 4. Has an active case of tuberculosis May have been vaccinated with BCG Has immunity to TB due to an earlier infection Any of the above is possible 31 Q’s 1. Which of these is an infection of the lower respiratory tract: 1. 2. 3. 4. Botulism Diphtheria Tuberculosis Streptococcal pharyngitis 2. An acid-fast stain of a patient’s sputum reveals acid-fast rods. This indicates infection with: 1. 2. 3. 4. Staphylococcus aureus Mycobacterium tuberculosis Corynebacterium diphtheria Any of the above is possible 32 Q’s 1. Which of these diseases is also known as Hanson’s disease: 1. 2. 3. 4. 5. Botulism Leprosy Tuberculosis Gangrene Anthrax 2. Staphylococcus aureus is responsible for all of the following except: 1. 2. Acne Impetigo 3. 4. Toxic shock syndrome Scalded skin syndrome 33 Q’s The diagram shows the structure of a: 1. Gram-negative cell wall 2. Gram-positive cell wall 3. Eukaryotic cell wall 34 Q’s The antibiotic Gentamicin binds the 30S ribosome subunit. This will interfere with: 1. 2. 3. 4. Protein synthesis in eukaryotic cells Protein synthesis in prokaryotic cells Cell division in eukaryotic cells Cell division in prokaryotic cells 35 Q’s Disease Bacteria 1. Bacillus 2. Streptococcus 3. Klebsiella 4. Escherichia 5. Neisseria 6. Staphylococcus 7. Mycobacterium 8. Clostridium 9. Corynebacterium a. Leprosy b. Diphtheria c. Anthrax d. Strep throat e. Botulism f. Hemorrhagic colitis g. Pneumonia h. Scarlet fever i. Skin infections j. Tetanus k. Meningitis l. Tuberculosis m.Acute endocarditis n. Food borne diarrhea o. Gas gangrene p. UTI 36