02 M301 Spec Exam&Cult 2011
advertisement

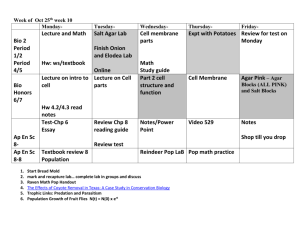
Specimen Cultivation How do you grow these bugs? Clinical Microbiology Diagnosis “Gold Standard” – culture isolation and identification of viable pathogen Future trend - rapid, non growth dependent detection of MO Microbial antigen (specific antibody, i.e. ELISA) Microbial nucleic acid - sensitive, need 1 copy, amplification of DNA, i.e. PCR; RT-PCR (RNA reverse transcribe to DNA) Diagnosis: Require Pure Culture Identify MO by biochemical methods Antimicrobial sensitivity testing In the clinical lab - streak original sample out on primary isolation media to get isolated colonies MO Isolated Each isolated colony pure culture, progeny of single cell Each bacteria forms a characteristic colony: shape, size, color, texture, adherence to medium Colonial characteristics often used as first step in identification of bacteria Bacterial Colonial Morphology Culture Media Artificial media on which bacteria and fungi grown Some bacteria never successfully grown on artificial lab media Treponema pallidum – grown in testes of rabbits Mycobacterium leprae – grown in armadillo or foot-pad of mice Obligate Intracellular Parasite Some bacteria – Rickettsia, Chlamydia All viruses (non-cellular) Cultured in living host - whole organism or tissue cell culture Identify virus grown in tissue cell culture by: Electron microscope - see virus in cell Cytopathic effects (damage or change in cell) Inclusion body (viral products) Syncytia formation (cell fusion) Rounding up of cell (death) Cytopathic Effect: Inclusion Body (Rabies virus) Cytopathic Effect: Syncytia Formation (Herpesvirus) Cytopathic Effect: Cell Rounding (Poliovirus) Diagnosis: Obligate Intracellular Parasite Growth time consuming and expensive Detect MO by immunological methods Direct assay - antigens of MO, usually in tissues (use specific antibody as a reagent) Indirect assay - host immunological response (antibody) against MO (use specific microbial antigen as a regent) Diagnosis: Antibody Assay Serology – diagnose infection by assaying for antibodies in patient’s serum against causative agent: Take both acute (patient most ill) and convalescent (patient recovering) phase specimen One looks for a 4-fold rise in antibody titer between acute and convalescent specimens ELISA – Enzyme linked immunosorbent assay: Use microbial antigen (specificity) Enzyme detection (sensitivity) Rapid testing Diagnosis: Parasites Not easily grown on artificial media or in living hosts Detection based on visual microscopic identification of: Parasite (trophozoite, free-living stage) Ova or cyst stage of parasite Entamoeba histolytica (ameba): Trophozoite Entamoeba coli (ameba): Cyst Taenia solium (tapeworm): Scolex Taenia solium (tapeworm): Proglottids Enterobius vermicularis (roundworm): Ova Ascaris lumbricoides (roundworm): Ova Culture – When? Specimen plated immediately Delay may result in: Loss of fastidious or anaerobic MOs Overgrowth by normal flora - change of total number and relative number of MOs Culture Media Diagnostic labs vary in choice of routine plating media used for growing different types of specimens Take into account what pathogens anticipated in specimen Also consider: Growth requirements CO2 Temperature requirements (RT, 37ºC) General Purpose Culture Plating Media Supports growth of most common pathogens, non-selective Permits isolation and differentiation of wide variety of bacteria Differences: colony size, shape, color, texture, adherence to culture media Nutrient Agar Plate Columbia Blood Agar (CBA) Plate: Differential Allows differentiation based on bacteria hemolysin that destroy red blood cells in the agar Alpha () hemolysis incomplete hemolysis and appears as green halo surrounding the colony Beta () hemolysis complete hemolysis and appears as clear area surrounding the colony Gamma () hemolysis - no hemolysis Chocolate Agar (Choc) Plate Essentially same as blood agar, except RBCs lysed Releases hemin and NAD for fastidious MOs Gives medium chocolate brown color CBA and Choc termed “enriched media” because of blood nutrients in media Selective Media Special nutrients that support growth of certain pathogens and/or inhibitors that suppress growth of competing NF Columbia Blood agar with antibiotics (Columbia CNA) – select for G(+): Sheep blood Antibiotics Colistin & Nalidixic Acid Why does it inhibit G(–) bacteria? MacConkey, Salmonella-Shigella, Hektoen Enteric agar – select for G(-) Bile salts to inhibit MOs Why does it inhibit G(+) ? Selective/Differential Media Selective media is also usually differential Addition of a carbohydrate (CHO) and a pH indicator differentiate MO that ferment the CHO and those that do not Mannitol Salt Agar (MSA): Selective - 7.5% NaCl to suppress MOs not halophilic Differential - Mannitol (CHO) and pH indicator phenol red MSA Plate MO grows on media ferments mannitol, acid is produced and lowers pH At low pH, phenol red = yellow MO that ferments mannitol turn media yellow MacConkey Agar (Mac) Plate Selective - Crystal violet and bile salts inhibit G(+) bacteria, fungi Differential – Lactose, pH indicator neutral red (red or pink at acid pH) Mac plates example of enteric agar plates which facilitate isolation and differentiation of enteric pathogens Mac Agar Plate MO able to grow on media and ferment lactose produce pink colonies (acid pH) i.e. E. coli MO that grow and don’t ferment lactose produce colorless colonies (neutral pH) i.e. Salmonella, Shigella Reducing Media Used for cultivating anaerobes Contains compounds that chemically combine with dissolved oxygen in media to deplete O2 Sodium thioglycolate broth: Thioglycolic acid - reducing agent to create anaerobic atmosphere deeper in tube Resazurin - oxygen-reduction indicator; in presence of O2, resazurin = pink Growth of MOs in Thioglycolate Broth Enrichment Media To prevent missing bacteria present in small number Usually liquid, provides nutrients and environmental conditions favor growth of one type MO while unsuitable for others Enrich stool culture for enteric pathogens found in low numbers relative to NF: Gram negative broth - bile & citrate salts inhibit G(+); mannitol enrich for Salmonella, Shigella) Tetrathionate broth - bile salts, thiosulfate, tetrathionate inhibit most G(+) & G(-) rods, except Salmonella Selenite broth - selenite inhibits G(-) rods, enterococci; allows recovery of Salmonella, Shigella Blood Culture Collected specimen inoculated into blood culture media directly at bedside of patient Two bottles of liquid media inoculated: Aerobic growth - Tryptic Soy Broth (TSB) Anaerobic growth – Thioglycolate Broth Bottles examined for turbidity, 7-14 days If turbidity develops, some media removed for Gram staining and subculture onto solid media Blood Culture Blood culture may routinely be Gram stain and subculture at specific intervals (24 hrs,48 hrs, etc.) even in absence of turbidity Bactec machines automatically detect growth in blood cultures by radioactive C14O2 production Quantitative Culture Often done on urine specimens A known volume of specimen plated on agar medium via calibrated loop and number of colonies counted Caution – this represents number of bacteria present at time of plating For clean catch urine specimen: >100,000 colonies/ml considered significant and indicative of disease For bladder or kidney specimen >10,000 colonies/ml considered significant and indicative of disease. Why? Quantitative Urine Culture Counts Culture: Unusual MO Some rarely encountered pathogens need special media and/or procedure for isolation If physician suspects one of these MO, must notify lab so appropriate media prepared and proper precautions taken, if necessary Brucella Bordetella Legionella Culture Incubation: Temperature Inoculated media incubated at 35-370 C, optimum growth temperature for most human pathogens Fungi often grown room temperature Many fungi dimorphic growth: Yeast at 370 C Mold at RT Candida albicans different growth: Yeast at RT Mold at 370 C, in the presence of serum (Germ tube test) Culture Incubation: Atmosphere Most pathogenic bacteria grow best in 2-10% CO2 Clinical Micro Labs routinely use 5% CO2 incubators Some bacteria require 5-10% CO2 in order to grow or to grow well (Neisseria, Streptococcus, Haemophilus) In the lab, we will grow these MOs in a “candle jar” to provide higher CO2 needed for growth Anaerobic Culture Reducing media may be used Plates may be incubated in special jar or pouch in oxygen free atmosphere (nitrogen gas) In an anaerobic jar, oxygen free atmosphere generated by chemical reaction Anaerobe Jar Envelopes of sodium bicarbonate and borohydride placed in jar and water added Chemical reaction generates CO2 and H2 H2 combines with O2 in presence of catalyst (palladium): 2H2 + O22H2O Thus O2 removed Indicator strip – methylene blue: Colorless in absence of oxygen Blue in presence of oxygen Culture Incubation: Time Most routine cultures: 16-18 hrs (overnight), before report negative CSF and blood cultures: one week, before report negative Wound cultures: 48 hrs, before report negative Fungal cultures: 3-4 weeks, before report negative Mycobacterium : 6-10 weeks, before report negative Class Assignment Textbook Reading: – Chapter 7 Microscopic Examination of Infected Materials – Chapter 8 Use of Colonial Morphology for the Presumptive Identification of Microorganisms Key Terms Learning Assessment Questions