Posterior Pituitary Disorders: SIADH & Diabetes Insipidus
advertisement

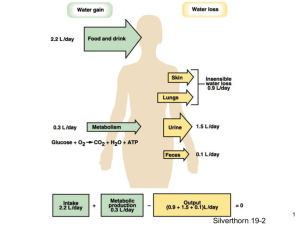
2 Disorders of the Posterior Pituitary Diabetes Insipidus Syndrome of Inappropriate Antidiuretic Hormone (SAIDH) Posterior Pituitary • Posterior pituitary hormones are actually produced in the hyopthalamus and only stored in the posterior pituitary • Posterior pituitary hormones – Antidiuretic hormone (ADH) – Oxytocin • The hormones secreted by the posterior pituitary are – Antidiuretic hormone (ADH) (Also call vasopressin) – and oxytocin. • ADH contributes to fluid balance by – Controlling renal reabsorption of free water – It also has potent vasoconstrictive properties. Posterior Pituitary • Antidiuretic hormone (ADH) (Also called vasopressin) – Excess: Syndrome of • Disorders/diseases resulting from dysfunction – Deficiency: Diabetes Inappropriate ADH secretion (SIADH) Insipidus SIADH Posterior Pituitary Hypersecretion SIADH - Syndrome of Inappropriate Hormone Secretion • ADH (anti-diuretic hormone) is a hormone made in the pituitary gland. • ADH does what the name says it stops urination - diuresis • Slowing or stopping urine production leads to fluid retention. • That in turn causes a dilution of body sodium SIADH - Syndrome of Inappropriate Hormone Secretion • Depending on the rapidity & the extent of the sodium drop, a battery of S/S appear. • Lethargy, weakness, & foggy thinking are common. Personality changes can happen. • Low sodium levels often make pt nauseated • If the situation is not corrected, seizures, coma, & even death can follow. Syndrome of Inappropriate Antidiuretic Hormone Secretion - SIADH • Results from many • SIADH occurs when there is too much vasopression (ADH) with inappropriate water retention and decreased blood Na levels different conditions and drugs • May be produced by certain tumors such as lung cancer or may result from chronic lung diseases. Medicines associated with SIADH include common meds as antidepressants, antianxiety agents, antipsychotic agents, seizure meds, and desmopressin (DDAVP) Syndrome of Inappropriate Antidiuretic Hormone Secretion - SIADH • Results from – – – – Inability to produce & secrete dilute urine Water retention Increased extra cellular fluid volume Hyponatremia Diseases that affect the hypothalamus Dx of SIADH • The following criteria should be fulfilled before a diagnosis of SIADH can be made: • persistent excretion of concentrated urine with no reason for ADH release • normal renal and adrenal function • no edema or hypovolaemia should be present • the urine osmolarity should be greater than the serum osmolarity Physical Assessment of SIADH • Initially, S/S are R/T retention of water. • Most common complaints – GI disturbances-loss of appetite, N,V • Nurse – Weighs pt & documents any recent weight gain – Checks pt extremities for presence of edema • Pt with SIADH have free water, not salt, that is retained & edema is not usually present due to intracellular free water Assessment-Clinical Manifestations of SIADH • Water retention, hyponatremia, & resulting fluid shifts have an effect on CNS function, especially when serum sodium level drops. Normal serum Na 135-145. S/S occur when serum Na level drops below 125, and especially below 115 • Clinical S/S • Lethargy, headaches, hostility, uncooperativeness, disorientation • Early sign -Change in LOC • Neurological S/S can progress from lethargy and headaches to decreased responsiveness, seizures, and coma. • Nurse assess deep tendon reflexes, which are often < or sluggish • V/S changes-tachycardia associated with increased fluid volume & hypothermia associated with CNS disturbance Normal Lab Values serum osmolality (285-295 mOsm/kg) sodium (Na 135-145 mEq/L) Urine osmolality -24 hr specimen 500-800 mOsm/kg H20 chloride (95-105 mEq/L) -Random specimen: 50-1200 mOsm/kg/H20 Osmolality is measures in milliosmoles per kilogram of water (mOsm/kg). The major determinants of plasma osmolality are Na, glucose, & urea Urine specific gravity 1.003-1.030 1.002-1.035 High=dehydration Low=diabetes insipidus concerntrated urine > than 50-100 mOsm/kg with normal vascular volume and normal renal function Lab Assessment in SIADH • Extracellular fluid volume expansion affects electrolyte levels in the serum and the urine • Elevated urine sodium levels and specific gravity reflect an increased concentration of the urine • Serum sodium levels are decreased, often as low as 110 mEq/L (normal serum sodium 135-145 mEq/L) due to extracellular volume expansion and increased Na excretion • Fluid retention causes changes in both plasma and urine osmolality • Plasma osmolality is decreased, and the urine is hyperosmolar in relation to the plasma Osmolality Urine osmolality -24 hr specimen 500-800 mOsm/kg H20 Random specimen: 50-1200 mOsm/kg/H20 • Osmolality is measures in milliosmoles per kilogram of water (mOsm/kg). The major determinants of plasma osmolality are Na, glucose, & urea. • The Kidneys are mainly responsible for maintaining the concentration of body fluids within this range of osmolality. • When the plasma osmolality becomes abnormal, changes in the level of antidiuretic hormones (ADH) cause the kidneys to conserve or increase the excretion of water to return the osmolality to normal Posterior Pituitary hypersecretion - SIADH Symptoms - fluid retention low serum osmolality (normal285-295 mOsm/kg) dilutional low sodium (normal Na 135-145 mEq/L) low chloride (normal95-105 mEq/L) Causes Diseases effect the hypothalmus pneumonia TB positive pressure ventilation Trauma concerntrated urine (> than 50-100 mOsm/kg) with normal vascular volume and normal renal function muscle cramps & weakness cerebral edema, lethargy, anorexia, headache, seizures, coma. AIDs delirium tremens Ectopic ADH secreting tumor SIADH - Diagnostic Tests • Blood & Urine tests • Must have – low serum sodium – low plasma osmolality level – Inappropriated concentrated urine (increased urine osmolality level) • These tests indicate – excess of body water relative to the amount of body sodium. • In other words, ADH is inappropriately holding onto too much water. • Important to eliminate other causes of a low sodium level, such as hypothyroidism or adrenal insufficiency, before settling on a dx of SIADH • Rx- removing the offending drug or tumor, & treat the Posterior Pituitary: SIADH,DI • *Affect kidney’s ability to concentrate urine* • Measured by urine specific gravity – Measures number and size of particles – Normal: 1.003 - 1.030 – High = dehydration – Low = Diabetic Insipidus 1.001-1.005 – Concentrated urine: SIADH – Dilute urine: DI Posterior pituitary: SIADH • ADH excess = water intoxication • water is reabsorbed, so assess for – increased blood volume, fluid retention – concentrated urine, low urine output – dilutional hyponatremia (same Na, more H20) • muscle cramps and weakness • anorexia, n/v, irritable, confused, disorient, seizure SIADH and Hyponatremia • Hyponatremia- a lower than normal concentration of sodium in the blood • Caused by inadequate excretion of water of by excessive water in the circulating bloodstream • In a severe case the pt may experience water intoxication, with confusion and lethargy, leading to muscle excitability, convulsions, and coma. • Treatment: Fluid and electrolyte balance may be restored by IV infusion of a balanced solution or a fluid restricted diet. SIADH Diagnosis & Treatment Diagnosis measure urine volume and osmolality Na < 134mmol/L se osmol >280mmol/kg SG>1005 low BUN, creatinine, Hb, Hct. Treatment If Na<125 Restrict fluids 800 - 1000 ml/day. Daily weigh Monitor 3% - 5% Saline solution IV Lasix if Na<105 (cardiac symptoms) SIADH • Diagnostic Study – Hyponatremia – Decreased plasma osmolality – Urine sodium and urine osmolality elevated – Elevated ADH levels++++++ – Normal renal, adrenal, & thyroid functions • Nursing Assessment • Headache,Personality change, Confusion,Irrritability, Dysarthria(difficult, poorly articulated speech), Lethargy,Impaired memory • Restless, weakness, fatigue, gait disturbances • Weight gain+++++ SIADH Treatment • Water Restriction is the cornerstone of treatment • Decreased water intake allows serum sodium level to rise normally. • The maximum amount of water that pt with SIADH are allowed to drink is just slightly more that the amount of urine they produce • Pt must have regular serum sodium measurements to ensure that the water restriction has been effective • Dehydration- The most concerning potential side effect from treatment is dehydration. SIADH treatment • • • • Restrict fluid intake (800-1000 cc/day) Daily weight Strict I & O Monitor urine specific gravity 0.9 NS infusion(to raise the serum Na level if water intoxication is severe) • Monitor for hyponatremia • Lasix may be admin to block circulatory overload • Drugs-demeclocyclin HCL & lithium-may be admin to block renal response to ADH, intereferes with action of ADH • Drugs - Phenytoin - inhibits ADH release • Surgery & Chemo -to remove or destroy neoplasms that may be the underlying cause of this syndrome SIADH treatment • Demeclocycline (Declomycin) • Lithium • Used for: – Excess secretion of ADH or SIADH • Action: – Inhibits ADH action in kidney – Blocks renal response to ADH, interferes with action of ADH • Therapeutic outcome: – Decreased urine specific gravity Analysis - Nursing Diagnosis - SIADH • 1. Fluid Volume Excess R/T compromised regulatory mechanism, excess ADH • 2. High Risk for Injury R/T an altered level of consciousness, confusion, & the possibility of seizures • 3. Altered Nutrition: Less than Body Requirements R/T an inability to ingest or digest food or absorb nutrients because of biologic factors (ex-anorexia, N/V) • 4. Altered Thought Processes R/T physiologic changes within the central nervous system Planning & Implementation • Planning: Pt Goals • The primary goal is that the pt’s fluid balance will be restored • Interventions to treat SIADH (Pt Care Plan) consists of • Restriction water intake • Using diuretics to promote the excretion of water • Administering drugs that interfere with the action of ADH • Replacing lost sodium • Fluid Restriction • Any excessive free water intake will further dilute the serum sodium concentration • Strict I&O, daily weights, guides the determination of the degree of fluid restriction necessary. A wt gain of 2 pounds (or 1 Kg) or more per day or a gradual increase during several days is cause for concern. • A 1 Kg weight increase is equivalent to 1000ml fluid retention (1Kg = 1 L) Planning & Implementation • Hypertonic saline (3% NaCl) may be used to treat SIADH – Helps correct serum sodium level – Raises Na osmolality in the blood – Removes excess intracellular fluid – Cells shrink in hypertonic solution • Drug Therapy • Diuretics are sometimes used to treat pt with SIADH, to rid the body of excessive fluid, especially if CHF • IV saline is given cautiously because it results from fluid overload may contribute to the fluid overload already present & precipitate an episode of CHF. • If diuretics are used, be aware of potential effect of electrolyte losses; • If the pt needs routine IV fluids, the MD sodium loss can be orders a solution in saline (5% dextrose potentiated, which further in saline) rather than a solution in water. contributes to the clinical picture of SIADH Planning & Implementation • • • • High Risk for Injury Promote safety Monitor pt neuro status Subtle Changes, such as muscle twitching before neuro S/S progress to seizures or coma. Check LOC to time, place, & person because disorientation may be present. • Confusion is another neuro sign. Nurse reduces environmental stimuli & explain interventions in simple terms. • Flow sheets contain ongoing info about LOC, motor & sensory neuro assessment, & pertinent lab data helpful in detecting trends. • Decreased LOC and seizures are complications of the low serum sodium level R/T SIADH Nursing issues • Monitoring fluid balance(s/s fluid retention): • Cardiac problems (water reabsorbed so >bld volume): • Neurological problems coma,): • Energy limitations (headache seizures,cerebral edema, (muscle cramps, weakness): • Allied health problems (anorexia): • Risk for injury: (confusion, muscle tremors, etc.) Nursing issues • Fluid Volume Excess R/T inability to excrete water • Hyponatremia with plasma hypo-osmolality • Weight gain • Potential for Injury – Institute seizure precautions and safety measures – Reorient confused pt • Prevent complications of immobility • Recognize decreased gastric motility due to hyponatremia, combined with fluid restriction and decreased mobility - >constipation Diabetes Insipidus Posterior Pituitary Diabetes Insipidus • Uncommon syndrome of posterior pituitary hypofunction • S/S – Increased thirst - polydipsia – Increased urination - polyruia • Results from – ADH (Vasopression) deficiency, which prevents the kidneys from reabsorbing water – Inability to conserve water Posterior pituitary : DI • Diabetes insipidus: “to pass through” • Decreased ADH = diuresis • Water is lost, so assess for: – Kidneys produce large amts of dilute urine (5L-10L in 24hrs) – low urine specific gravity (1.001-1.005) – polyuria (>urine output), polydipsia (>thirst) – fluid deficit • weight loss, turgor,dehydration, hypotension, constipation, shock Posterior Pituitary hyposecretion Diabetes Insipidus • Symptoms- • Thrist & polyuria 5 - 20L/day • • SG < 1005 Urine osmol < 100 mmol/L • Se osmol > 295 mmol/kg • Urine specific gravity low (1.001-1.005) • Urine osmolality decreased (50-200 mOsm.kg) • Nocturia • Urine less concentrated than plasma • Weakness => weight loss, hypotension, tachycardia, constipation, shock. • Plasma osmolality elevated (>295 mOsm/kg) • Sleep deprivation-due to interrupted by need to drink fluids & urinate • Hypernatremia in blood Diabetes Insipidus Etilogy • Familial or idiopathic • Head injury • Neuorsurgery • Damage to the hypothalamic areas that produce ADH • Cause • Lesion of hypothalmus interferes with ADH synthesis/transport/relea se • brain tumour • pituitary/cranial surgery • head trauma • CNS infection • vascular disease. Diabetes Insipidus Etilogy • Drug Related • Ethanol & Phenytoin (Classification: Antiarrhythmic, Anticonvulsant): – Inhibit ADH secretion • Lithium (Classification: Antimanic) & Demeclocycline(Classification:anti-infective-Tetracycline): – Inhibit ADH action in kidney 4 Types of Diabetes Insipidus • 1) Neurogenic -also known as – – – – – central hypothalamic pituitary neurohypophyseal Caused by a deficiency of the Antidiuretic hormone, vasopressin • 2) Nephrogenic-also known as – Vasopressin - resistant – Caused by insensitivity of the kidneys to the effect of the antidiuretic hormone, vasopressin • 3) Gestagenic-also known as – Gestestional – Caused by a deficiency of the antidiuretic hormone, vasopressin, that occurs only during pregnancy • 4) Dipsogenic, a form of primary polydipsis – Caused by • Abnormal thirst and the • Excessive intake of water or other liquids • Diagnosis D.I. Diagnosis & Rx • History and examination Diabetes Insipidus • Water deprivation test (see next slide) • Vasopressin challenge test (see next slide) • 24 hours urine • High sodium in blood • MRI of pituitary, hypothalmus and skull to see damaged areas • Treatment • Intravenous fluids Hypertonic saline IVExtracellular solution to pull fluid from outside the cell to inside the cell • Vasopressin SC/IM/IV, nasal prep • Long term DDAVP (Desmopression) nasal prep. (analog ADH) Diagnosis - Fluid Deprivation Test (To identify cause of polyuria) • Baseline VS, then check hourly-allows RN to detect changes, esp postural hypotensin & tachycardia • Deprive pt of fluid-Observe for compliance with fluid restriction • Hourly- urinary output, specific gravity, & osmololity • Urine test results determine whether testing can proceed. – Testing can proceed if urinary osmolality stabilized for 3 samples and 3% wt loss is noted Dx- Vasopressin challenge • Order for 5 Units of aqueous vasopressin sc • Continue hourly urinary measurements • Vasopressin triggers and ongoing assessment detects Changes in urinary specific gravity and osmolality – Specific gravity & osmolality decrease with primary and secondary diabetes insipidus – No response is seen with nephrogenic diabetes insipidue Diabetes insipidus treatment • Vasopressin (Pitressin) : is ADH • Classification: Hormone (antidiuretic) • Uses: Treatment of central diabetes insipidus sue to deficient antidiuretic hormone. • Route/Dose: IM, sc, nasal spray • Nsg Implications: • replace fluid: saline and glucose • monitor I & O • check specific gravity • observe electrolytes • Monitor adverse reactions-abdominal cramps, angina, MI Diabetes insipidus treatment • Desmopressin (DDAVP) • Classification: Hormone (andiuretic) • Indication: Management of primary nocturnal eneuresis unresponsive to other treatment modalities • po, sc, IV, Intranasal • Action: An anologue of naturally occuring vasopressin (antiuretic hormone). Primary action is enhanced reabsorption of water in the kidneys • Therapeutic Effects: Prevention of nocturnal enuresis. Maintenace of appropriate body water content in diabetes insipidus. • Nsg Implication: Monitor urine & plasma osmolality & urine volume frequently. Assess pt for symptoms of dehydration (excessive thirst, dry skin & mucous membranes, tachycardia, poor skin turgor) Weigh pt daily & assess for edema Observe for Water Intoxication with all agents • ADH excess = water intoxication • water is reabsorbed, so assess for – increased blood volume, fluid retention – concentrated urine, low urine output – dilutional hyponatremia (same Na, more H20) • muscle cramps and weakness • anorexia, n/v, irritable, confused, disorient, seizure Diabetes Insipidus • Fluid Volume Deficit R/T inability to conserve water – Thirst, dry mucous membranes – Decreased skin turgor – Hypotension, tachycardia – Hemoconcentration, plasma hyperosmolality, hypernatremia – Increased urine output – Dilute urine-monitor specific gravity Nursing Issues • Fluid and electrolyte imbalance: • • • • • • • • R/T >diuresis, monitor urine and plasma osmolarity monitor specific gravity (usually will be low with >diuresis) monitor urine volume (usually will be high 5-10L in 24 hr) Therapy successful when urine output and specific gravity begin to return to normal monitor s/s dehydration weight pt daily & assess for edema Fluid volume deficit Nurse will monitor for hypotension, constipation, shock • Sleeping problems: R/T nocturia & increased thirst • • Education: