Preparing for a CLER Visit
advertisement

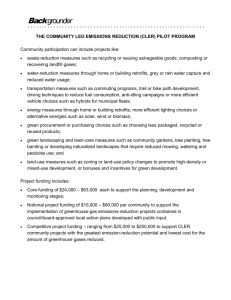
Making CLER “clear” Preparing for the Clinical Learning Environment Review What is CLER? “The Clinical Learning Environment Review (CLER) is a mechanism by which the ACGME assesses a Sponsoring Institution (SI) to evaluate its commitment to developing a culture of quality, patient safety, and performance improvement for both resident education and patient care.” CLER Goals Support national efforts addressing patient safety, quality improvement, and reduction in health care disparities. Monitor Sponsoring Institution maintenance of a clinical learning environment that promotes the six goals. Emphasizes the responsibility of the SI for the quality and safety of the environment for learning and patient care. Increase resident knowledge of and participation in safety activities and quality improvement. Intent to improve physician integration into quality and safety goals after graduation. CLER Focus Areas Supervision Healthcare Quality Patient Safety Professionalism Healthcare Disparities Duty Hours Fatigue Management Transitions of Care CLER: Five Key Questions 1. Who and what form was the hospital/medical center’s infrastructure designed to address the six focus areas? 2. How integrated is the GME leadership and faculty in hospital/medical center efforts across the six focus areas? 3. How engaged are the residents and fellows? 4. How does the hospital/medical center determine the success of its efforts to integrate GME into the six focus areas? 5. What are the areas the hospital/medical center has identified for improvement? Who IS the SI? Who will participate in CLER? Phase 1 focused on “large” program SIs (about 290 institutions) Now moving on to Phase 2: “small” program SI: 2 or fewer core programs, with or without “subs” (about 450 institutions) Who IS the SI? Who will participate in CLER? Hospital-sponsored program: the hospital; possibly the clinic Clinic-sponsored (FQHC) program: the clinic, and likely the hospital as well More than one hospital: either possible, but the most likely is the one where the most rotations are done Non-clinical sponsor: the sponsor will need to be involved, but the clinic and/or hospital will be reviewed CLER Site Visit Process: Materials Intentional short notice (allowance for need to find other times) Limited advance materials to prepare Organizational charts Policies: Supervision, Duty hour, Care transitions Patient safety and Quality protocols/strategies Quality & Safety Committee membership rosters (identifying resident members) CLER Site Visit Process 1 or 2 CLER site visitors Three methods of obtaining information: Interviews of residents, faculty, and program directors using Audience Response System Interviews with SI leadership, and Patient Safety and Quality officers “Walk rounds” Oral report to leadership at end of visit Written report to follow Optional program response to report CLER Site Visit Process: People Health-system Leadership: “C-suite” CEO, COO, CMO, CNO, DIO Patient Safety/Quality Officers Residency/fellowship program personnel (separately by group): Program Directors Core faculty Resident representatives CLER Site Visit Process: People Hospital walk- arounds led by residents Interview hospital staff Observe patient hand-offs Senior Leadershi p Meeting Program Director Meeting Faculty Member Meeting Safety and Quality Leadershi p Meeting Resident Meeting CLER Outcomes Intended to provide: “Aha’s!” Experiences that inform learning A progressive set of activities for higher performance in organizational engagement in GME Not intended to provide: “Gotcha’s” New stealth accreditation requirements CLER Outcome Examples Patient safety: ACGME: resident respondents: 67% aware of safety incident; only 46% reported an incident. WWAMI “mock” visits: hospital patient safety systems highly variable, but many quite robust; residents with only limited engagement. “Aha’s”: All institutions have this as one of their highest priorities, and voiced high level of enthusiasm for engaging more with residents and faculty. Residents enthusiastic when included. CLER Outcome Examples Quality in WWAMI: Education on quality improvement All institutions had systems, but neither residents nor faculty are regularly receiving reports. Residents not aware of Core Measures or hospital QI priorities. Resident engagement in QI activities All residents working on quality-oriented projects. Residents receive data on quality metrics Not consistently occurring. Neither meaningful or usable. IT personnel struggling to keep up. CLER Outcome Examples Quality in WWAMI: Resident engagement in planning for QI All institutions voiced strong support for including residents in QI initiatives. Few residents currently involved. Education on reducing health disparities Limited in scope. Stronger in FQHC-based programs. Resident engagement in initiatives to address health disparities ACGME: almost entirely related to use of interpreters. WWAMI: again stronger in FQHC-based programs. CLER Outcome Examples Supervision: ACGME: resident respondents: 21% perceived an incident of inadequate supervision. SI leadership: 43% reported events related to inadequate supervision, most common on nights/weekends. WWAMI “mock” visits: more positive results in our programs. “Aha’s”: nursing staff “empowerment” to ask questions and use chain of command when deemed important to patient safety. CLER Outcome Examples Fatigue management (duty hours): ACGME: resident respondents: 32% would “power through” 2 hours of shift even when “maximally tired”; underuse of mitigating plans. WWAMI “mock” visits: almost full compliance of programs with duty hours. “Aha’s”: culture of “checking in” near ends of shifts. CLER Outcome Examples Professionalism: ACGME: resident respondents: 15% compromised their integrity to satisfy an authority figure. SI leadership: 63% reported a professionalism issue in past year. Walk rounds: 75% reported incident of disruptive or disrespectful behavior. WWAMI “mock” visits: generally more positive results. “Aha’s”: institutions that demonstrated intolerance of disrespectful behavior. CLER Outcome Examples Transitions of care: ACGME: WWAMI “mock” visits: almost all resident teams using structured protocols, but limited use of interdisciplinary teams. Inpatient/outpatient hand-offs remain challenging. “Aha’s”: Observing effective resident to resident patient care transition. Nurses engaging with residents in transitioning patient care. Approaching CLER: benefits These are ALL critical areas for patient care and resident education Sponsoring institutions in general are highly enthusiastic about increasing engagement with GME programs around mutual goals of importance Important opportunities for resident and faculty innovation and systems improvement Approaching CLER: benefits Sample Quality recommendation themes Form CLER Committee to identify opportunities for resident and faculty engagement, without unduly burdening schedules with committee assignments . Create a Quality Curriculum for residents and faculty. Commit to specific initiatives that address health care disparities. Increase education around Core Measures and other hospital-based measures. Identify mutual goals for inpatient and outpatient activities. Approaching CLER: concerns “One more thing to have to do….” History of limited effective engagement of the SI with its sponsored program. For family medicine, little integration of inpatient and outpatient goals and strategies. Lack of resources (espec IT) locally to facilitate the changed expectations. Burden of CLER visit itself. What to Do Now? Build relationships with Healthcare System Leadership Clinical integration into health system Patient safety/quality promotion Participate in health systems’ goals and initiative development Educate leadership on Institutional Requirements and CLER process Educate residents, hospital staff, and faculty on likely questions and progress meeting health system goals Engage your residents and faculty in strategic planning for including CLER goals What to Do Now? Patient safety: include residents in real, meaningful experiences: Root cause analysis Patient safety reporting Quality: Obtain clinical effectiveness data LEAN/RPIW teams Work with SI leadership, including safety and quality officers (one should be on GMEC) Include residents in SI initiatives in patient safety, quality improvement, and addressing health care disparities What to Do Now? Implement meaningful policies for supervision and duty hours Develop transitions of care protocols Provide fatigue management/mitigation training Develop monitored standards for professionalism Summary: CLER visits CLER “mock” visits can be powerful tools to facilitate collaboration between SIs and programs on mutually beneficial goals and strategies regarding health care quality. CLER discussions can increase value of program to SI. All participants perceived high value in this collaboration, but also expressed significant apprehension about the time and resources required, particularly inadequate data systems. Resources: CLER visits CLER Pathways to Excellence (ACGME): https://www.acgme.org/acgmeweb/Portals/0/PDFs/CLER/C LER_Brochure.pdf CLER Site Visit Instructions (ACGME): https://www.acgme.org/acgmeweb/Portals/0/PDFs/CLER/C LERSiteVisitInstructions.pdf Consider a “mock” CLER visit from the Network!