(synovial) fluid
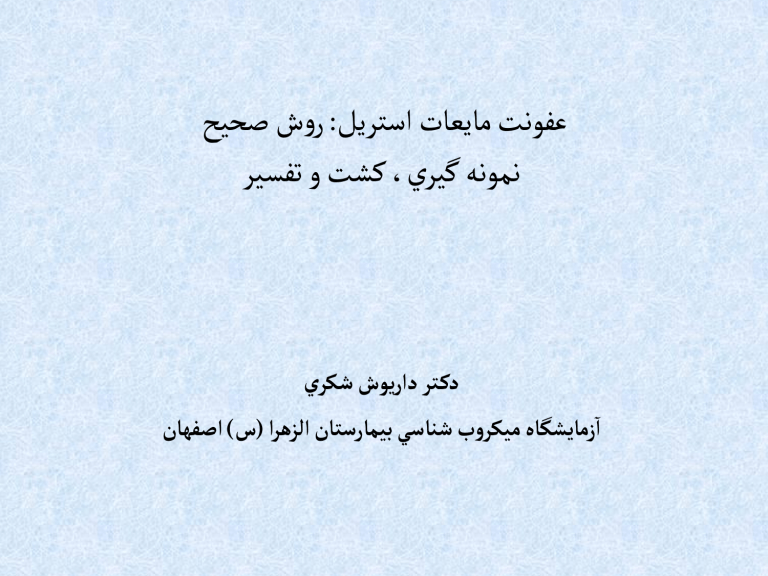
حيحص شور : ليرتسا تاعيام تنوفع
ريسفت و تشك ،يريگ هنومن
يركش شويراد رت كد
ناهفصا ) س ( ارهزلا ناتسراميب يسانش بورکيم هاگشيامز ا
• severe morbidity and mortality resulted by
Infection of normally sterile body fluids
• therefore, rapid and accurate microbiological assessment of these samples is important for successful patient management.
• any microorganism that is not flora should be considered significant and some flora that may inter.
Body Sterile Fluids
1. Cerebrospinal, CSF
2. Serous (pleural, peritoneal, pericardial),
3. Synovial fluids.
Cerebrospinal fluid (CSF): fluid within the membranes surrounding the brain and spinal cord.
Collected by lumbar puncture .
Joint (synovial) fluid: fluid at the union of two bones
Pleural fluid: fluid within the membrane surrounding the lungs
Empyema : any purulent body cavity fluid; usually refers to purulent pleural fluid
Thoracentesis : pleural space fluid collected by transcutaneous puncture of the chest wall
Peritoneal (abdominal) fluid: fluid within the membrane lining the abdominal cavity
Ascites : abnormal accumulation of fluid within the abdominal cavity
Paracentesis : abdominal fluid collected by transcutaneous puncture of the abdominal cavity.
Pericardial fluid: fluid within the membrane surrounding the heart
Body fluid in blood culture bottles
Collection & Transport
Basic Concepts
Collect the specimen from the actual site of infection, avoiding contamination from adjacent tissues or secretions.
Collect a sufficient quantity of material.
Use appropriate collection devices: sterile, leak-proof specimen containers. Use appropriate transport media
Whenever possible, collect specimens prior to administration of antimicrobial agents.
Properly label the specimen and complete the test request form.
The specific source of specimen is required.
Minimize transport time.
Maintain an appropriate environment between collection of specimens and delivery to the laboratory.
If appropriate, decontaminate the skin surface.
Use 70-95% alcohol (ALC) and 2% chlorhexidine or 1-2% tincture of iodine (TIO) to prepare the site. Allow a contact time of two minutes to maximize the antiseptic effect.
A sterile collection tube must be used for microbial studies.
ensure that the proper transport is utilized. (For example, anaerobic culture requests need to be submitted in anaerobic transport media; bacteriology requests should not be in viral media; AFB requests should not be in anaerobic transport media.
The use of anticoagulants is not recommended.
Use heparin if necessary.
Do not refrigerate body fluid samples, especially CSF, since organisms such as
Haemophilus species, Neisseria species, and
Streptococcus pneumoniae are sensitive to cold temperatures.
Process samples as soon as they are received.
If possible, submit at least 10 ml of fluid for culture.
The volume of peritoneal effluent sent for culture should be at least 50 mL because larger volumes increase the yield of positive culture.
Cerebro Spinal Fluid
)
CSF
(
Collection of CSF sample → Lumbar puncture (LP)
CSF Fluid usually collected from arachnoid space. A sterile needle is inserted between 3th and 4th lumbar vertebrae and the CSF is allowed to drip into a dry sterile container
CSF must collected in three sterile tube:
Tube1 : for biochemical examination
Tube2 : for microbiological examination
Tube3 : for cytology examination
► S.pneumoniae, H.influenzae & N.meningitidis are fastidious and fragile bacteria.
► CSF should be examined as soon as possible, with in 1 hour from the time of collection.
► Don ’ t exposed the CSF to sunlight or extreme heat or cold.
Synovial fluid
• Synovial is formed as an ultrafiltrate of the plasma across the synovial membrane, which mucopolysaccharide containing hyaluronic acid and a small amount of protein is secreted by the cells of the synovial membrane.
Synovial fluid may be collected by syringe in a procedure termed arthrocentesis , also known as joint aspiration.
The normal amount of fluid contained in the knee cavity is less than 3.5 ml, this amount increases in disorders of the joints.
Recommended specimen containers include:
Plain, sterile tube for microbiologic testing and crystal examination.
Classification
Synovial fluid may be classified into normal, noninflammatory, inflammatory, septic, and hemorrhagic: septic:
WBC /mm 3 : >50,000
Polys (%): > 70
Clarity: Opaque
Specimens collected using a sterile syringe and needle must not be transported with the needle on the syringe.
Needles must be carefully removed and properly discarded and the syringe cap aseptically replaced on the syringe tip.
All specimens must be properly labeled with the patient's name, medical record number, location and the time and date the specimen was collected.
•
Specimens are transported at room temperature and must reach microbiology as soon as possible.
• Native body fluid samples for anaerobic culture must be received within 2 hours of collection.
Pleural Fluid
•
Pleural fluid is found in the pleural cavity and serves as a lubricant for the movement of the lungs during inhalation and exhalation.
•
It is derived from a plasma filtrate from blood capillaries and is found in small quantities between the layers of the pleurae – membranes that cover the chest cavity and the outside of each lung.
Processing & Culture
Initial processing
1) If >2 ml of sample is received, centrifuge at
3000 rpm (1800 x g) for 5 minutes or 10-20 min at 2000 rpm.
2) Remove all but a small portion of the supernatant. Reserve supernatant from CSF
samples for antigen testing.
3) Gently re-suspend the pellet using a sterile transfer pipette.
Direct smear
Label a glass microscope slide with the laboratory identification number.
Clean the slide with alcohol and allow to dry.
Place one drop of the re-suspended pellet onto the clean slide. Smear the drop over a small area of the slide using the tip of the transfer pipette.
Heat- or methanol-fix the dried smear and gram-stain.
Note the presence and quantity of WBC’s,
RBC’s, and any microorganisms.
Issue a written preliminary report.
For CSF samples, make a verbal report of the
Gram’s stain findings to the submitting provider or ward.
Culture
Media
Blood agar
Chocolate agar
MacConkey agar (or EMB)
CDC anaerobic blood agar (or Blood agar incubated anaerobically)
Thioglycollate broth
BHI advised when recovering a few bacteria is aimed
QC of media
All media QC must be performed by standard
Bacteria (ATCC)
Incubate Blood agar, MacConkey agar, and
Thio at 35-37C in an ambient air.
Incubate Chocolate agar at 35-37C in a candle jar or CO
2 incubator.
Incubate anaerobic plates at 35-37C in an anaerobe jar with gas pack.
Interpretation
1) Examine all aerobic media after overnight incubation. If there is no growth on the plates and the thioglycollate broth and BHI is clear, reincubate and examine for a total of 4 days.
2) Examine anaerobic media after 48 hours of incubation. If there is no growth, discard the plates.
Growth on Blood agar, Chocolate agar &
MacConkey agar (or EMB) show a gram negative bacteria ( Enterobacteriaceae and other gram negative bacilli )
Growth olny on Blood agar, Chocolate agar show a gram positive bacteria
Only growth on Chocolate agar show a fastidious bacteria such as Haemophilus influenzae
• Identification must be done based on biochemical test based on kind of bacteria growth condition and gram smear
If the morphologies observed do not match growth on the plates (if any), subculture the broth to solid media .
If the original specimen was cultured anaerobically, also subculture the broth to anaerobic plates.
c) If organisms are growing on the anaerobic plates:
1] Correlate growth on aerobic and anaerobic plates
– most clinical isolates grow both aerobically and anaerobically (facultative growth)
2] Perform a Gram’s stain of each colony type present
3] Subculture each colony type to a BAP incubated aerobically and a second BAP incubated anaerobically. Incubate overnight.
a] Consider organisms that grow aerobically and anaerobically as aerobes (facultative) b] Consider organisms that grow only on the anaerobic BAP as obligate anaerobes.
4] This laboratory does not have anaerobic organism identification capability. See Results Reporting section below.
• yeast or mold are isolated.
Isolation of suspected contaminants
1] Environmental contamination is suspected when : a] Growth occurs outside the streak lines b]An organism is isolated that is only considered a true pathogen under special circumstances e.g.
mold c] Growth occurs on the plates but not in the broth
2]Skin contamination is suspected when an organism normally present on the skin is isolated e.g.
coagulase-negative staphylococci, diptheroids
Correlate culture findings with the direct specimen Gram’s stain and CSF antigen results.
1) CSF a) Orally notify the ordering provider or ward of direct smear findings. Document the date, time, and to whom you reported the results b) Issue a written preliminary report with the Gram’s stain results
2) Other body fluids - issue a written preliminary report with the Gram’s stain results
B.
Negative cultures
– report “No growth after 4 days.
Positive cultures
1) Preliminary report a) Issue when significant growth occurs b) Provide as much detail as possible
1] Quantity and gram-morphology. Example:
Moderate lactose-fermenting gram-negative rods
2] Give organism name if known based upon rapid tests such as Staphaurex, oxidase, spot indole
Example 1: Many Staphylococcus aureus. Susceptibilities to follow.
Example 2: Moderate Pseudomonas aeruginosa.
Susceptibilities to follow.
2) Final repor
Report complete organism name (genus and species) – do not abbreviate
Report all appropriate susceptibility results
(when applicable) c) Anaerobic bacteria
1]Report anaerobic nature and Gram’s stain morphology
2]Example: Few anaerobic gram-positive cocci
• Great care must be taken when examining smears since some organisms may be few in number.
• Smear preparations that are too thick may be difficult to interpret.
LIMITATIONS:
A.False-positive cultures can occur due to contamination of the sample with skin flora.
B.False-negative cultures can occur due to low numbers of organisms in the specimen, prior antimicrobial treatment, or the fastidious nature of the etiologic agent.
CSF infection: Acute pyogenic (bacterial) meningitis
► Streptococcus pneumoniae
► Neisseria meningitidis
► Haemophilus influenzae
► Group B Streptococcus
► Escherichia coli
► Listeria monocytogenes
► …
peritoneal infection: Spontaneous bacterial peritonitis (SBP)
•
SBP is the development of peritonitis (infection in the abdomina cavity) despite the absence of an obvious source for the infection.
•
It occurs almost exclusively in people with portal hypertension (increased pressure over the portal vein), usually as a result of cirrhosis of the liver
•
It can also occur in patients with nephrotic syndrome.
•
The diagnosis of SBP requires paracentesis
(aspiration of fluid with a needle) from the abdominal cavity.
•
If the fluid contains bacteria or large numbers of neutrophil granulocytes (>250 cells/µL), infection is confirmed.
The most commonly occurring organisms are enteric gram-negative rods such as Escherichia coli and Klebsiella spp., which cause more than half of all infections. Gram-positive organisms cause about 25% of infections.
Although some series show Streptococcus pneumoniae as the most common streptococcal organism others find the viridans group as the predominant gram-positive pathogen.
Enterococcus spp. have been documented in
6% to 10% of cases.
S. aureus is noted infrequently, representing only about only 2% to 4% of all SBP infections.
the most frequently isolated organisms included E. coli, streptococci , and Klebsiella spp.; these accounted for more than 80% of all cases of SBP
Plural infections
•
The bacteria isolated from infected pleural effusion vary significantly between community- and hospitalacquired infections.
•
Streptococcus milleri group
• staphylococci
•
Streptococcus pneumonia
• anaerobes
•
Less common organisms responsible for communityacquired infection include other streptococci , enterobacteria , Haemophilus influenzae ,
Pseudomonas spp., tuberculosis, and Nocardia.
•
In an earlier study it was reported that nosocomial pleural infections were most commonly caused by methicillin-resistant
Staphylococcus aureus , other staphylococci , and enterobacteria such as Klebsiella pneumoniae