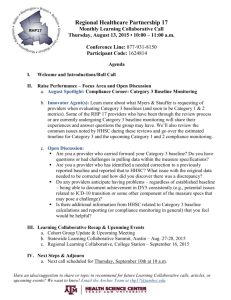
Optimizing Laboratory Testing Learning Session 2 February 12
advertisement

1 Pursuing High Value Healthcare Optimizing Laboratory Testing Learning Session 3 April 2, 2015 Central Vermont Hospital Conference Center Few Reminders 2 Please silence your cell phones, pagers, etc Restroom location Collaborative Materials Agenda Worksheets Morning Agenda 3 Welcome and Collaborative Timeline Team Reports Break Research Findings- Optimizing Laboratory Testing PDSA- Putting Ideas into Action Lunch Afternoon Agenda 4 Data Update NORC Data Upload Report Reviews Data Comparisons Team Working Session -Design at least one PDSA to implement -Determine Process Measures and create a data collection plan -Discuss potential barriers Team Report Out from Working Session Next Steps Welcome 5 ALLEN REPP Kick-Off Week 1 Collaborative Timeline Sept 11, 2PM Pre-work 5-6 weeks Learning Session 1 Oct. 22 8:30 to 3:30 Continuous Coaching/Faculty Support Conference Call / Webinar Nov 6, 2PM Conference Call / Webinar Jan. 8, 2PM Conference Call / Webinar Dec 4, 2PM Learning Session 4 Jun. 4 DHMC 8:30 to 3:30 6 Learning Session 2 Feb. 12 UVM 8:30 to 3:30 Conference Call / Webinar May 7, 2PM Conference Call / Webinar Mar 5, 2PM Learning Session 3 Apr. 2 CVH 8:30 to 3:30 Our Vision 7 Continuous Quality Improvement State-wide learning, sharing & support system Patient Centered Improvement Efforts Foundation: Common Tools & Techniques Quality Improvement Tools Model for Improvement Common Lab Improvements & Site Specific Improvements Our First Collaborative: Global Aim 8 We aim to reduce harm to patients and conserve system resources by optimizing the use of laboratory tests for patients cared for in our region’s hospitals. We will use a collaborative approach considering the best medical evidence and quality improvement science. It begins with an evaluation of current test ordering profiles and patterns followed by an organized plan to optimize testing and ends with a plan to sustain these practices. By doing this we expect to reduce cost and improve satisfaction and quality of care for patients and the health system. It is important to work on this now because as health care professionals we can play an important role in health care reform by designing more patient-centered, efficient and high value inpatient care. Optimizing Laboratory Testing Collaborative Team Reports Learning Session 3 April 2, 2015 Optimizing Laboratory Testing Collaborative Our Team Report Team: UVMHN CVMC Learning Session 3 April 2, 2015 Our Team Team Members – List Names and Institutional Roles: Don Weinberg, MD Kristin Calcagni, Lab Judy Perdue, Lab Justin Stinnett-Donnelly, MD Kevin Knapp, IT Tommie Murray, QM Team Meeting Frequency and members who attend: Monthly meetings Our Data Status of Baseline Data Query: Run Please see next Slide Specific Institutional Aim(s) and other data reviewed to support your aims: (Please use the AIM template language on the QI Monitoring Worksheet) Decrease the number of laboratory draws / day Patients will not getting woken up at 6am with a needle Reduce the possibility of anemia Reducing patient pain and discomfort 2013-01 2013-02 2013-03 2013-04 2013-05 2013-06 2013-07 2013-08 2013-09 2013-10 2013-11 2013-12 2014-01 2014-02 2014-03 2014-04 2014-05 2014-06 2014-07 2014-08 2014-09 2014-10 2014-11 2014-12 2015-01 2015-02 # Labs / 1000 Pt Days 1400.0 1200.0 1000.0 800.0 1000 800 600.0 600 400.0 400 200.0 200 0.0 0 Patient Days Baseline Data 1/2013 – 2/2015 (# tests/1000 pt days) 1600 1400 Patient Days Average All Labs 1200 ALB ALK BILT BUN CA CaIo CL CRE1 HCT HGB K MCV MG 600 2013-01 2013-02 2013-03 2013-04 2013-05 2013-06 2013-07 2013-08 2013-09 2013-10 2013-11 2013-12 2014-01 2014-02 2014-03 2014-04 2014-05 2014-06 2014-07 2014-08 2014-09 2014-10 2014-11 2014-12 2015-01 2015-02 2015-03 # Tests / 1000 Pt Days 1200 1000 800 1000 -5 stDev 800 400 600 400 0.3 stDev 200 200 0 0 # Patient Days CVMC March Data 1600 1400 -2.2 stDev 1200 Patient Days WBC WBC Avg BUN BUN Avg MG MG Avg +2SD -2SD Our Ideas/Theories for Change Change Ideas/Theories to meet Specific Institutional Aim: Modification of standardized admission orders to eliminate recurrent orders for CBC, BMP and CMP Continue ability for MDs to add recurrent labs when clinically indicated Action Plan and Timeline for each Change Idea: March 2, 2015 Our Next Steps Data review monthly Calculation of total numbers of each test / patient / day Optimizing Laboratory Testing Collaborative Our Team Report Brattleboro Memorial Hospital Learning Session 3 April 2, 2015 Our Team Team Members – List Names and Institutional Roles: Aida Avdic – Hospitalist A. Shams Helminski – Hospitalist Michele Rowland, Charmaine Winton – Quality Frank Field , Doreen Lincoln, John Farina – IT Carolyn Allen - Laboratory Team Meeting Frequency and members who attend: Monthly meetings Email exchange Our Data Status of Baseline Data Query: Extracts completed – data uploaded to NORC this week Specific Institutional Aim(s) and other data reviewed to support your aims: (Please use the AIM template language on the QI Monitoring Worksheet) Minimizing routine morning laboratories (CBC and BMP) for patients admitted within 24 hours (evening and night admissions) Optimizing CBC ordering for stable patients (every 48-72 hours) Our Ideas/Theories for Change Change Ideas/Theories to meet Specific Institutional Aim: Hospitalist meeting (monthly update and reminders) Limitations of the electronic health record (no easy way to build in reminders or ‘hard stops’) Effect of shift change / service change Action Plan and Timeline for each Change Idea: Test period March and April Reminders on Hospitalist work stations Our Next Steps Data analysis and comparison of pre / post intervention Awaiting data for March Feedback to Hospitalists Other tests to address? Optimizing Laboratory Testing Collaborative Our Team Report The University of Vermont Medical Center Learning Session 3 April 2, 2015 Our Team Team Members : Allen Repp MD, Chief, Primary Care Internal Medicine Mark Fung MD, Medical Director Lab and Pathology Mark Pasanen MD, Program Director, Internal Medicine Hospitalist Program and Internal Medicine Residency Program Jill Warrington MD, Pathology Lauren Pearson MD, Pathology Resident Maria Burnett MD, Medicine Resident • Meeting Frequency: • • Standing weekly meeting Meeting approximately 1x/month since our last collaborative session. Work accomplished in sub-groups Trace Barrett MD, Medicine Resident Steven Jarzembowski MD, Medicine Resident LeAnna Burgess MD, Medicine Resident Melissa Holman RHIA, CHDA, Senior Measurement Analyst, Jeffords Institute for Quality Allison Kaigle Holm PhD, Senior Research Specialist, Jeffords Institute for Quality Heidi Guevin RN, Quality Improvement Consultant, Jeffords Institute for Quality Our Data Status of Baseline Data Query: Preliminary data retrieved for 2013 Required baseline data accessed from UVMMC shared drive • Specific Institutional Aim(s) and other data reviewed to support your aims: Decrease unnecessary venipunctures and blood loss Retrieved and reviewed All Service Medicine Admissions with standing daily lab orders • Family Practice, Medicine, PCIM Our Ideas/Theories for Change Change Ideas/Theories to meet Specific Institutional Aim: Education for healthcare providers Modify admission order sets with daily labs Modify “a la carte” orders with daily option Patient lab needs discussed on rounds with rounding tool/checklist Lab orders to identify last three results Lab orders to identify costs of labs Hard stop to indicate/identify need for daily lab order Eliminate lab testing on day of discharge Incentives for not ordering labs Action Plan and Timeline for each Change Idea: MD Education- presentations at education forums: 2/2, 2/4, 3/3 Modify Gen Med/Family Med Admission order sets: PRISM re-engaged, meet 4-6-15 Modify Admission order sets from other services Modify “a la carte” lab orders: TBD Resident (medicine/pathology) Survey surrounding ordering practices-draft 4-2-15 Chart Audit Tool- draft 4-6-15 Optimizing Laboratory Testing Collaborative Our Team Report Porter Hospital Learning Session 3 April 2, 2015 Our Team Team Members – List Names and Institutional Roles: Amber Bailey, Information Technology Marianne Collins, Quality Director David Rand, Hospitalist Julie Vest, Lab Director Rebecca Woods, Information Technology Director Team Meeting Frequency and members who attend: We will meet as a team to review our data in the next week or two Our Data Status of Baseline Data Query: Data submitted. Looking forward to the results Specific Institutional Aim(s) and other data reviewed to support your aims: Create a QI culture Decrease blood draws, patient discomfort, anemia Our Ideas/Theories for Change Change Ideas/Theories to meet Specific Institutional Aim: -Decrease frequency of reflex platelet checks when on lovenox -Cease phlebotomy practice of from drawing extra “hold” tubes ….More to come once data is reviewed Action Plan and Timeline for each Change Idea: -Not yet defined Our Next Steps Review data Invite all stakeholders in the next two weeks to meet Optimizing Laboratory Testing Collaborative Our Team Report NVRH Lab Collaborative Learning Session 3 April 2, 2015 Our Team • Team Members – List Names and Institutional Roles: • Michael Rousse, MD, MPH Hospitalist Director • Bonnie Torres, MLS (ASCP) Director of Laboratory Services • Andrea Dinneen, MBA, MPH CIO, VP Information Services • Jim Coulson Infection Control Officer • Ryan Cloutier Application Support Analyst Team Meeting Frequency and members who attends: Currently developing team strategy Our Data Status of Baseline Data Query: All Baseline Data has been collected and uploaded to NORC. Specific Institutional Aim(s) and other data reviewed to support your aims: Reduce the number of unnecessary labs Target CBC/CBCD, BMP/CMP, Albumin, and Troponins (w and w/o reflex testing) Study Number of Tests, Number of Tests per Avg Daily Census, Number of Tests per Patient per day. Compare the total Number of Phlebotomies, Avg Daily Census, Avg LOS, and Annual Discharges for 18 yo+. Our Ideas/Theories for Change Change Ideas/Theories to meet Specific Institutional Aim: Develop a safe method to reduce unnecessary labs as identified by our data Possible Solutions Modify Workflows Modify Order Sets Incorporate Order Level Decision Support Etc. Action Plan and Timeline for each Change Idea: TBD after receiving initial results from data analysis Our Next Steps Work with the Collaborative’s Data Analysts Begin collecting monthly data Finalize Team Strategy Begin developing strategies to decrease the unnecessary labs Am J Clin Pathol 143:393-397 March 2015 issue Presentation By Mark Fung, MD PHD Univ of Vermont Medical Center Study Design 2 month intervention in general medicine units at 400 bed hospital Educational flyers in offices Periodic email reminders of using daily lab tests only if results changed patient care 2 month pre-intervention data (982 patients) 2 month post-intervention data (988 patients) Measured # of daily blood tests/patient/day Included CBC, BMP, CMP, PT/INR, PTT Messaging Interactive educational sessions with providers and nurses Discussions at division meetings and noon conferences Educational flyers in provider and nurse work areas Weekly e-mail communication to all providers and nurses 3 Consistent Points Covered Providers should: Question the utility of very blood test and order only if result will affect patient care Think about the impact that costs of blood tests have on health care expenditures Consider “adding on” test to blood samples already collected whenever possible Results Am J Clin Pathol 143:393-397 Pros and Cons to their approach Pros Low cost intervention – talks, flyers, emails, awareness Did not compromise provider work flow or efficiency Con Unknown how much of the improvements will persist long term http://onlinelibrary.wiley.com/doi/10.1002/jhm.2354/abstract (in press) Study Design – QI intervention 53 providers across 4 inpatient facilities Focused on common labs ordered by a large community hospitalist group Academic detailing, audit, feedback, and transparent reporting of performance Pre-analysis was 10 month baseline (n=7824) 7 month intervention period (n=5759) Messaging Introductory email recommending 2 changes: Immediate stop to practice of open-ended ordering of common labs as daily Assessing the need for common labs in the next 24 hours, and ordering based on that need, but no further into the future Messaging (continued) Providers were informed that number of common labs ordered daily would be monitored prospectively Monthly reports given to individual providers Top 5 hospitalists with highest frequently ordered labs sent a personal e-mail notification of their “top five” status Messaging (continued) Monthly report included: Reminder of the recommendations and reasoning in the original e-mail List of all members and their frequency of lab ordering as daily (open ended) per month Recommendation to discontinue daily ordering of common labs At least one example of a patient with 5 days of daily labs with no mention in the progress notes Limitations of this study Patient characteristics were statistically different between pre-analysis and intervention period (but small) Choosing Wisely Report was made public during same time of start of intervention period Baseline and Intervention time periods were not seasonally matched. Quality Improvement Process Global Aim 3 Measure(s) Change Ideas Step 8- Test Your Changes Step 7 –Determine Process Measures Success Measure 2 SDSA 1 3 2 1 PDSA Step 6- Brainstorm Change Ideas Specific Aim Global Aim Theme Step 5 –Determine Cause and Effects Step 4- Create Specific Aim Step 3- Create Global Aim We are here! Step 2- Get Baseline Data Assessment Step 1- Form Team 52 Modified from Quality By Design, A Clinical Microsystems Approach Nelson, Batalden and Godfrey© Trustees of Dartmouth College Model for Improvement 53 1. What are we trying to accomplish? 2. How will we know that a change is an improvement? 3. What changes can we make that will result in an improvement? Avoid this turning into a viscous cycle. Small short term tests of change. TAKE ACTION! Setting Aims Establishing Measures Selecting Changes Testing Changes Important Things to Know about the Model for Improvement • Can be used for most types of changes • Focus on small tests of change • New tests are based on what you learn • Approach should not create chaos • Only spread to others when you are ready Why Test? • Increase your belief (and others!) that the change will result in improvement • Document how much improvement can be expected from the change • Understand the effects – upstream & downstream • Minimize resistance to change Tips for Testing Changes • • • • • • Team approach (interdisciplinary) Understand where you are today – baseline Do not try to get buy-in, consensus, etc. Strive for Ownership not buy-in! Test with engaged volunteers Scale down size of test • # of patients, location, # of providers • Run tests in a small period of time • Test over a wide range of conditions • Different days, ages, genders, locations Small RAPID Tests of Change Act • Adopt, adapt or abandon based on what was learned • Build knowledge into next PDSA cycle Study Plan • State objectives • Make predictions • Who will do what by when Do • Complete analysis •Carry out the test • Compare data to prediction •Document problems, • Summaries what surprises, observations was learned Reminder: Balanced Cycles Too Much Planning Act Do Too Much Studying Act Act Plan PLAN Study Too Much Doing Plan Study DO STUDY Do Too Much Acting ACT Plan Too Much Studying Study Do Reminder: Push Yourself & Your Team If you think you can test it in… 1 Day……..few hours 2 Weeks….few days 1 Month….1 week 1 Year……wrong model! Form Team-Rutland Regional Hospital Step 1- Form Team Team Members Name Role Team Members Name Joe Walker Role Project Admin and Lab Lead Dr. Rick Hildebrant MD Lead Wendy Bixby Admin Support Sherry Ravlin IT Data Mgr Deborah Roy IT Project Mgr Daniel Michel IT Report Writer Rob Mcginness IT Interface Elizabeth Mahar-Kyhill Nursing Lead Dr. Susan Blish MD Alternate Angela Murphy Performance Improvement/QM Assessment Step 2- Baseline Data- Inpatients > 18 yrs. of age calendar yr. 2013 Baseline Data Hemo Lytes # of Tests #Tests/Avg. Daily Census # Tests/Patient Day Total Inpatient Lab Tests # Annual Inpatient Phlebs AVG Daily Census AVG Length of Stay (LOS) Annual # of discharges 18yr+ EMR Based Order Protocols? BUN Creat PTT TBD Institutional Aim Step 3- Create Institutional Aim We aim: To improve the quality and value of the care we provide to our patients by ensuring we order the appropriate laboratory tests during their stay. In/at: Rutland Regional Medical Center The process begins with: Analyzing how our laboratory ordering and collection data compares to the rest of the collaborative. The process ends with: A workflow to minimize unnecessary laboratory testing. By working on the process, we expect: To reduce unnecessary testing and phlebotomy and to improve patient satisfaction with their care. It is important to work on this now because: We have an opportunity to improve the quality and value of the care we provide to our patients. Specific Aim Step 4 –Create Specific Aim We will: Decrease 30% of the contracted hospitalists will reduce the percentage of day 2 CBC’s ordered on patients with a normal admission CBC for COPD. From: our current value to be provided by the collaborative To: less than X% of the current value By: June 1, 2005 Fishbone/Cause and Effect Diagram Step 5- Determine Cause and Effect Equipment People Resident vs attending Daily Labs Tab in EHR Central Line Draws Why do we have so many repeat HCT’s on HCT Stable patients? Can’t see previous Lab Ordering Process Rounding Process Patient/Family Request Order Sets EHR Way we have always done it Process Environment Report Monitoring Report Monitoring Change Ideas Step 6- Brainstorm Change Ideas List Possible Change Ideas: Plan Step 7- Determine Process Measures/Plan What will be Measured Who will Measure? How will it be measured? When Plan Step 7- Determine Process Measures/Plan What will be Measured Who will Measure? How will it be measured? When DO Step 8- Test Your Change Cycle 1 Date: February 16, 2015 What Who How When Study What was learned? What will be changed? ACT Cycle 2 What What was learned? What will be changed? Date: February 23, 2015 Who How When Lunch!! DATA UPDATE Data Definitions Patient Patient Days: (“date/time discharge – date/time admit”)/24 Patient Stays Hospital Days: 0 (admission), 1, 2, 3, 4, 5, …. Data Initial Measures: Admissions Number of Patient Days: sum((“date/time discharge – date/time admit”)/24) Number of Unique Patient Stays Number of Unique Patients Length of Stay: average, standard deviation, median, 25th & 75 percentiles 15 Most Frequent DRGs Data Initial Measures: Labs Number of Unique Date/Time Collections Total Number of Date/Time Collections 15 Most Frequent Lab Test Codes Data Initial Measures: Refining (HELP!) What DRGs do we want to exclude? 775 vaginal delivery w/o complications 765 cesarean section with complications 766 cesarean section w/o complications others? What Lab Test Codes should we focus on? collaborative vs. institution specific distinguishing lab panels vs. individual tests – is there a need? do we know what these test codes mean? are these all blood tests? Data Pending Measures Distribution of Hospital Days Day 0 (day of admission) Day 1 (starts 12am after day of admission) Day 2 And so on…. Number of Unique Date/Time Collections by Hospital Day Day 0 Day 1 Day discharge Day discharge -1, etc Data Pending Measures Sequential Date/Time Collections Do patients get the same labs every day? Normal lab results How can we define if a value is within a standard normal range? If you have two normal values in a row, what is the probability the third draw will be abnormal? Stable lab results If values are not within a normal range, how we can tell if there is change over time? Delta checks Focus on the abnormal values Data Collaborative Comparison Measure The number of unique date/time collections per patient day # Unique date/time collections in a given month Total Number of Patients Days in a given month Data Collaborative Comparison Measure The number of unique date/time collections per patient day UVM MC: 25,223/8,667.08 = 2.91 (Oct 2014) CVMC: 931/1,568.21=0.59 (Oct 2014) RRMC: 2,305/2,687.31= 0.86 (Oct 2014) PMC: 101,422/25,755.15=3.94 (All Baseline) NVRH: 13,804/14,232.37=0.97 (All Baseline) BMH: 557/471=1.18 (Dec 2014) Bennington: pending DHMC: pending Working Session 83 ALL TEAMS & ORGANIZATIONS Supported Team Working Session 84 Review Tracking Tool & Action Plan Review Institutional/Specific Aims Create at least one PDSA to implement Determine Process Measures and data collection plan Consider possible barriers Team Report Outs 85 PDSA Plan Process Measures Data Collection plan Barriers What might limit your ability to change? What support will you need? 86 We wanted to make it easy for teams across institutions to easily share documents with each other Protected, but not difficult to access Admin approval needed before documents can be seen Created a section on the website where team members can upload, and download files Each institution has its own username and password Used across the institution Will provide username and passwords to team leaders 87 How do you use the Shared Team Document function? Start at VMSFoundation.org Click on the Optimizing Laboratory Testing Collaborative image (home for all Collaborative information) Click on Shared Team Documents Option to Upload or Download files, make choice and enter username and password 88 Uploading a file: File Title - Give it a name File Description - Summary paragraph Click Browse and then select the file on your computer Click upload Categorize document 1. 2. 3. 4. 5. 6. Institution: Select your institution Document Category: Data, Interventions, Measurement, Other, References Click preview and/or save It will not appear in the database immediately. An admin will have to approve. Five of us, so should happen quickly. 89 Downloading a file: Click Download Documents 1. Documents are sorted by Document Category and Project 2. Click parameters to sort 3. Click on desired file name and then apply to download. Next Steps Keep meeting with your team! Determine frequency time and location of future meetings- Schedule them! Collect and/or Validate Baseline data Finalize your site specific improvement aims Finalize your change ideas Finalize your plans to measure your success Plan your PDSA cycles Check out our website Work in progress VMSfoundation.org: click on High Value Care for Vermonters box We will be contacting you to set up a time for one of us to join a team meeting at your location.