Time in Therapeutic Range PST vs UC vs ACC
advertisement

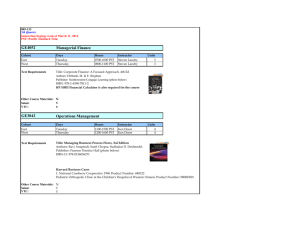
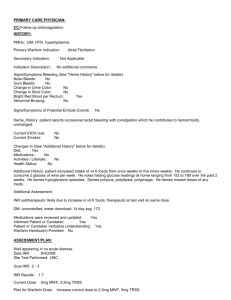
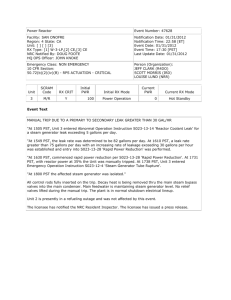
Improving the Outcomes of Oral Anticoagulation: Home Monitoring of Warfarin Therapy Jack Ansell, M.D. Lenox Hill Hospital, NY September 22, 2009 Disclosures Consultant: Roche Diagnostics, ITC, HemoSense The Dilemma of Anticoagulation Management • Warfarin has a narrow therapeutic window of effectiveness and safety. • Many factors influence a patient’s stability within that window. • Frequent monitoring is required to maintain patients in the therapeutic window. • Monitoring is labor intensive and complex. • • Consequences Increased adverse events with poor management Physicians avoid warfarin use because of its complexity. ORAL ANTICOAGULATION IS ALL ABOUT MANAGEMENT The Desired Outcome: Benefits must be greater than Risks Hospital Transition to Outpatient Outpatient Hemorrhage Risks1,2 INR Reduction in risk of stroke or venous thromboembolism (VTE) Benefits2,3 1. Ansell J et al. Chest. 2004;126:204S-233S. 2. Hirsh J et al. J Am Coll Cardiol. 2003;41:1633-1652. 3. Rothberg MB et al. Ann Intern Med. 2005;143:241-250. Transition from Hospital to Ambulatory Care Settings 4 How well does a University Hospital do in managing warfarin therapy? “Inpatient Warfarin Medication Utilization Evaluation” Treatment decisions involving inappropriate assessment of response • 349 records reviewed and assessed by established criteria • 647/2030 (31.8%) warfarin treatment decisions were deemed inappropriate Total = 647 decisions 8% Initial dose too high (52 decisions) Initial dose too low (9 decisions) 1% 10% Different dose from home therapy (63 decisions) 1% 1% Continued home dose but should have been changed (6 decisions) 10% Continued home dose but should have been held (4 decisions) Held dose when therapy should have been restarted (66 decisions) 69% PK/PD not taken into account (447 decisions) 5 Is the correct starting dose used? “Inpatient Warfarin Medication Utilization Evaluation” 35.3% (123/349) patients were initiated on warfarin in-house for the first time New starts (n=123) 51% Dose ok Dose too high 7% 42% Dose too low 6 What is the impact on outcomes? “Inpatient Warfarin Medication Utilization Evaluation” New starts for VTE indication (n=47) Initial Dose Inappropriate (n=23) Bleeding events Bleeding risk distribution Vitamin K use 4 documented bleeds 3 transfusions ≥ 2 u 5 > 2 g/dL decr. Hgb 15 high risk 6 moderate 2 low 4 pts Initial Dose Appropriate (n=24) 2 documented bleeds 4 transfusions ≥ 2 u 5 > 2 g/dL decr. Hgb 11 high risk 8 moderate 5 low 1 pt 7 Models of Chronic Anticoagulation Management Routine Medical Care (Usual Care) AC managed by physician or office staff w/o any systematic program for education, follow-up, communication, and dose management. May use POC device or laboratory INR Anticoagulation Clinic (ACC) AC managed by dedicated personnel (MD, RN or pharmacist) with systematic policies in place to manage and dose patients. May use POC device or laboratory INR Patient Self-Testing (PST) Patient uses POC monitor to measure INR at home. Dose managed by UC or ACC Patient Self-Management (PSM) Patient uses POC monitor to measure INR at home and manages own AC dose Challenges With Conventional Laboratory Testing • Patient issues – Time for traveling to office or laboratory – Ability to travel – Need for venous access • Labor-intensive and higher costs – Scheduling visits – Proper handling and delivery of sample – Documentation at several time points • Potential for communication delays – Laboratory to contact provider with results – Provider to contact patient with dosage adjustments Jacobson AK. In: Ansell JE, Oertel LB, Wittkowsky AK, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis, Mo: Facts and Comparisons; 2003;45:1-6. Technology Advances: Offers a new paradigm for monitoring since 1987 • Use of capillary whole blood1,2 – Allows fingerstick sampling2 – Appropriate for self-testing1 • Consistency of INR results1 • Portability1 – Can be done anywhere • Simplicity1 – Patient can easily perform test 1. Leaning KE, Ansell JE. J Thromb Thrombolysis. 1996;3:377-383. 2. Ansell JE. In: Ansell JE, Oertel LB, Wittkowsky AK, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis, Mo: Facts and Comparisons; 2003;44:1-6. What are the outcomes with Home Monitoring? Thromboembolism with PST or PSM vs Control Heneghan et al. Lancet 2006;367:404 Thromboembolism with PST or PSM PSM Usual Care PST AMS Heneghan et al. Lancet 2006;367:404 Major Hemorrhage with PST and PSM vs Control Heneghan et al. Lancet 2006;367:404 Author Year Intervention # Patients TTR (% or time in range) Major Hemorrhage Thromboembolism PST vs UC Beyth 2000 PST/ams* vs UC 163 vs 162 56 vs 32 p<0.001 5.6% vs 12% p=0.049 8.6 % vs 13% p = 0.2 23 vs 24 93 vs 75 p=0.003 0 0 0 vs 1 event 0 PST vs AMS White 1989 Kaatz 2001 Gadisseur 2003 THINRS 2009 PST/ams* vs AMS PST/ams* vs AMS PST/ams* vs AMS 63 vs 65 p=NS 52 vs 60 PST /ams vs AMS 63.9 vs 61.3 p=0.14 ~68% vs 63% p = NS PSM vs UC Horstkotte 1998 Sawicki 1999 Fitzmaurice 2002 Kortke 2001 Sidhu 2001 Sunderji 2004 Voller 2005 PSM vs UC 75 vs 75 92.4 vs 58.8 PSM vs UC 83 vs 82 57 vs 33.8 p=0.006 1 event vs 1 event 1 event vs 2 events PSM vs UC 23 vs 26 74 vs 77 p=NS 0 vs 1 event 0 PSM vs UC 305 vs 295 78.3 vs 60.5 p=<0.001 1.7 % vs 2.6% p=NS 1.2% vs 2.1% p=NS PSM vs UC 34 vs 48 76.5 vs 63.8 p<0.0001 1 event vs 0 1 event vs 0 PSM vs UC 69 vs 70 71.8 vs 63.2 PSM vs UC 101 vs 101 67.8 vs 58.5 p=0.0061 2 events vs 0 0 vs 1 event PSM vs AMS 49 vs 53 84.5 vs 73.8 1 event vs 0 1 event vs 0 PSM vs AMS 47 vs 52 66.3 vs 63.9 p=0.14 1 event vs 1 event 0 PSM vs AMS 40 vs 39 71.1 vs 70.4 PSM vs AMS 368 vs 369 58.6 vs 55.6 p=NS 4 events vs 7 events 4 events vs 20 events PSM vs AMS Watzke 2000 Gadisseur 2003 Khan 2004 MenendezJandula 2005 Improving AC Outcomes at the Time of Discharge 128 patients randomized to home POC monitoring (n= 60) or UC (n=68) after discharge. POC testing on d 2,4,6,8 vs UC on d 8 Discharge Home UC Monitoring Monitoring Sub-therapeutic 49% 47% Therapeutic 42% 45% Supra-therap 9% 8% Day 8 Home Monitoring 29% 67% 4% UC Monitoring 33% 41% 26% p value <0.01 Adverse events up to day 90 Major Bleeding Total Bleeding Embolic Event Readmit due to AC Complication Death Home Monitoring 2 15 9 3 7 (n=59) Usual Care Monitoring 10 36 10 8 8 (n=68) 0.05 0.009 NS 0.32 NS Jackson et al. J Intern Med 2004:256:137 Who is able to perform Home Monitoring? Considerations for Patient Selection Willing to: Learn and perform testing procedure Keep accurate written records Communicate results in timely fashion Able to: Participate in a training program to acquire skills/competencies to perform self-testing Generate an INR Understand implications of test result Maintain records Reliable to: Perform procedure with acceptable technique to obtain accurate results The THINRS Trial: Design • Purpose: Compare HQACM with PST to HQACM alone on major health outcomes • Patient population: Atrial fibrillation or mechanical heart valve • Participating Centers 28 VA Med Ctrs with ACC of > 100 patients • Two parts: Part 1: Training and home testing for 2-4 weeks Part 2: Competency assessment and, if capable, randomization to HQACM every 4 weeks or PST every week Matchar. Amer J Med 2002;113:42-51 The THINRS Trial: Design A key attribute “everyone” was those who were randomized to management of this trial is that trained for PST and deemed capable, then either PST or ACC Matchar. Amer J Med 2002;113:42-51 The THINRS Trial: Intervention & Outcomes Interventions: • HQACM (monthly INR) Designated, trained staff person Local standard management algorithm • PST (Weekly INR) Interactive value response reporting system with web-based local monitoring Outcomes: • Primary time to first major event (stroke, major bleed, death) • Secondary time in range, satisfaction, quality of life Matchar. Amer J Med 2002;113:42-51 The THINRS Trial: Participants 3,644 Trained 78 did not pass training 3,566 home with meter for 2-4 weeks 508 dropped out 3,058 competency assessment 136 did not pass assessment or dropout 2,922 randomized 2,922 / 3,644 = 80% Passed Competency Matchar. Amer J Med 2002;113:42-51 Summary from THINRS: Outcomes • 80% of screened subjects demonstrated PST competency and were randomized – approx. 4 out of 5 pass • Patients were less likely to pass PST, if – Older, h/o CVA, poor cognition, low literacy, poor manual dexterity Matchar. Amer J Med 2002;113:42-51 Summary from THINRS: Outcomes: Stroke, Bleed, Death PST HQDM 4,235 pt yrs 4,495 pt yrs Event Type HQACM Rate per pt-yr PST Rate per pt-yr Total Rate per pt-yr Stroke 32 0.76% 31 0.69% 63 0.72% Major Bleed 189 4.46% 173 3.85% 362 4.15% Death 157 3.71% 152 3.38% 309 3.54% Total 378 8.93% 356 7.92% 734 8.41% Summary from THINRS • 80% of screened subjects demonstrated PST competency and were randomized – approx. 4 out of 5 pass • Patients were less likely to pass PST, if – Older, h/o CVA, poor cognition, low literacy, poor manual dexterity • Outcomes (TTR & AEs) were improved to a small degree with PST How Does Home Monitoring Achieve Good Outcomes ? • Access to testing Frequency (convenience), timeliness Greater Time-in-Range • Consistency of testing Instrument & thromboplastin Consistent Results • Awareness of test results Knowledge, empowerment, compliance Greater Time-in-Range Managing Home Monitoring? Trusting the INR Result FS LT INR = .258 + .89 * FS RT INR; R^2 = .956 5.0 INR by left hand fingerstick 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 1.0 1.5 2.0 2.5 3.0 3.5 4.0 INR by right hand fingerstick 4.5 5.0 Trusting the INR Result Thromboplastin — Reagent Combinations and observed variation in INR Ortho 1.00 BFA DADE 1.03 BFA Behring 1.08 BFA Pacific Hem 1.20 BFA IL Test 1.43 BFA 5.5 DADE 1.96 BFA 5 Ortho 1.00 ACL 4.5 4 DADE 1.03 ACL Behring 1.08 ACL Pacific Hem 1.20 ACL IL Test 1.43 ACL 3.5 DADE 1.96 ACL 3 Ortho 1.00 MLA 2.5 2 DADE 1.03 MLA Behring 1.08 MLA Pacific Hem 1.20 MLA IL Test 1.43 MLA 1.5 DADE 1.96 MLA Courtesy A. Jacobson Optimal Frequency of INR Monitoring* Test Interval vs % In Range 100 90 % in Range 80 70 60 50 40 30 More Frequent testing increases % in range 20 10 0 0 7 14 21 28 35 42 49 Days Between Tests Summary 18 published studies: PST Coalition Report, July 2000 Barriers to PST/PSM • Lack of physician awareness or acceptance1,2 • Fear it will lead to unintended self-management3 • Implementation of PST/PSM3 • Reimbursement3 1. Jacobson AK. In: Ansell JE, Oertel LB, Wittkowsky AK, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis, Mo: Facts and Comparisons; 2003;45:1-6. 2. Roche Diagnostics. CoaguChek System: Why Use? Available at: http://www.coaguchek-usa.com/ information_for_professionals/why_use/content.html. Accessed May 12, 2006. 3. Wittkowsky AK et al. Pharmacotherapy. 2005;25:265-269. Barriers to INR Patient Self-Testing (PST): National Survey of Anticoagulation Practitioners1 Cost of Device Main Barrier 90 80 78.7 70 60.4 60 Survey 50 Respondents 40 (%) 30 35.7 20 10 0 Cost of device Cost of reagent cartridges Fear of PST leading to PSM Provider Barriers to PST 1. Wittkowsky AK et al. Pharmacotherapy. 2005;25:265-269. Willingness to Pay for PST is low • Few patients are willing to pay for self-testing, despite the benefits of weekly testing. • Those willing to pay for PST stated an average of $18 per month as the acceptable out-of-pocket expense for home testing with a POC device. Amount Willing to Pay Out-ofPocket Per Month Percent Respondents n=71 $0 35% $5 - $30 51% $35 - $100 14% Proprietary information CMS did the right thing by approving reimbursement, but they did it the wrong way As of March 19, 2008 CMS expanded coverage to patients with VTE and chronic AF Medicare National Coverage Policy for Home PT/INR Testing (as of July 2008) Medicare will cover the use of home INR monitoring for chronic, oral anticoagulation management for patients with mechanical heart valves (non-porcine), chronic atrial fibrillation, or venous thromboembolism . The monitor and the home testing must be prescribed by a treating physician and all of the following must be met: • Patient anticoagulated for at least 3 months • Patient must undergo face-to-face educations program and demonstrate correct use of device • Patient continues to correctly use device • Self-testing no more frequently than once per week More information at: http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM6313.pdf Oral Anticoagulation Patient Self-Testing: Consensus Guidelines for Practical Implementation. Managed Care 2008;17(#10, Suppl 9):1-9 What is an IDTF ? CMS defined a new entity independent of a hospital or physician’s office in which diagnostic tests are performed by licensed or certified non-physician personnel under appropriate physician supervision. This entity is called an Independent Diagnostic Testing Facility (IDTF). The IDTF may be a fixed location, a mobile entity, or an individual non-physician practitioner and in all cases must comply with the applicable laws of any state in which it operates. IDTF’s… How They Work Manages Doctor INR Prof fee $9/mon Train fee $191 Rx INR Patient INR CMS IDTF Inst order Inst sent Device Manufacturer Tech fee $140/mon Serv + Inst Communication with patient doing home monitoring Oral Anticoagulation Patient Self-Testing: Consensus Guidelines for Practical Implementation. Managed Care 2008;17(#10, Suppl 9):1-9 PST dosed by internet expert system vs AMS Criteria AMS Supervised PST P - value 10.7 (+ 5.2) 41.7 (+ 6.6) <0.001 19.6 days 4.6 days <0.001 Time in range 58.6% 74% <0.001 Extreme INRs 6% 1.7 % <0.001 INRs < 1.5 45.9 % 33.3 % <0.001 INRs > 5.0 (%) 54.1 % 66.7 % 0.006 # INRs /pt (mean) Freq of testing (mean) RCT (cross-over) of 162 patients, followed for 6 months; mean age 59 yr (16-91), 80% male with diverse indications. Daily time to manage 80 patients 10-45 min (mean 23.2 min) Ryan et al. J Thromb Haemost 2009;7:1284 Conclusions . . . • • • • • • • • Anticoagulants (oral and parenteral) top the list for adverse events. Management of warfarin therapy is often poor, even in the best of circumstances. The transition from inpatient to outpatient anticoagulation is a critical transition that requires labor intensive systems and processes for successful implementation. POC INR technology can play an important role in facilitating such care. Anticoagulation management models include Routine or Usual Care, Anticoagulation Clinics, and PST/PSM (home monitoring) Point-of-care (POC) provides an alternative to laboratory testing that is easy, portable, and accurate and allows for testing either by physician or patient POC home monitoring can be done either with physician management or patient self-management Home monitoring requires systems in place to implement and manage results. IDTFs can perform much of the implementation and follow up tracking of results