Flow of Medicaid Funds to Your School District
advertisement

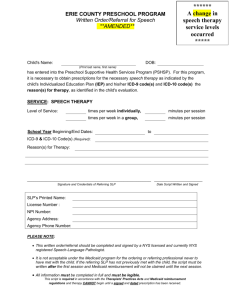
Medicaid in Education Settings – What Every SLP Needs to Know Janet Deppe, CCC-SLP Director, State Advocacy jdeppe@asha.org Overview; Topics we’ll cover History of Medicaid Funding Flow ChartsFederal/State/Local Medicaid Programs Federal Requirements Early and Periodic Screening and Diagnosis and Treatment Services (EPSDT) Overview Topics (cont) Administrative Claiming Medicaid and IDEA State Medicaid Plans Documentation and OIG Audits Preventing billing errors Accessing Medicaid $$ Overview Topics (cont) Medicaid Funding Success Stories Resources History of Medicaid Federal-state matching entitlement program for low income families 57 million Americans, 28 million children and 8.6 individuals with disabilites served (Herz 2005) $287 billion in Medicaid benefits (2004) $168 billion (federal) and $119 billion (state) History of Medicaid (cont) Program originated in Title XIX of the Social Security Act of 1965 Early Periodic Screening Detection and Intervention (EPSDT) added in 1967 1988 Catastrophic Medicaid Act allowed for billing in schools Funding of Medicaid Programs Medicaid funding is mandatory – IDEA funding is discretionary Administered according to State Medicaid Plan Two programs: medical assistance (ma), administration (admin) 50-83% matching rate for ma, 50% (admin) Flow of Medicaid Funds to Your School District Congress appropriates funds annually based on the federal fiscal year beginning on October 1st. Funds go to the U.S. Department of Health and Human Services Dollars are received at U.S. Dept. of Health and Human Services and are administered by the Centers for Medicare and Medicaid (CMS) Funds are put in the state’s account at the Federal level and the state draws down the funds as needed. • Funds are allocated to each state to match state expenditures for the cost of medical assistance (i.e., Medicaid is a federal-state matching system.) • Medicaid’s federal matching rates, or Federal Medical Assistance percentages (FMAPs), are determined by a formula tied to state per capita income. According to the Kaiser Commission on Medicaid and the Uninsured, on average the federal matching rate is 57% of the costs of Medicaid benefits (Medicaid Resource Book, July 2002) Dollars Received At State Level • State may or may not require LEAs or school districts to bill for Medicaid services. • If schools do participate, a system for billing is established: • States are not required to return all money generated by the schools back to the schools. It depends on state laws and regulations. (For example, a state may retain a percentage for administrative costs; a private vendor may retain a percentage.) Flow of Medicaid Funds to Your School Dollars Received At the Local Level • Medicaid revenue, if received by the school district (see above) is placed into the school budget and allocated as per state and/or local policy. Some states have specific requirements for how a local district must use funds. • Examples of how local school districts use Medicaid revenue: special education; general fund; health services; equipment/supplies; professional development; hiring staff; return funds to program that generated the revenue; purchase of technology for staff; creation of new special education programs. • Some states place restrictions on how local school districts may use Medicaid revenue. Examples: may only be used for educational purposes and shall not be made available to local communities for purposes other than education; may not be used to supplant funds currently being spent on health and social services; must be used within the special education program; may not be transferred to the district’s general fund. Teachers and Related Services Providers Funding reaches teachers and related service providers based on how local school district allocates the Medicaid revenue (see above) Students Students benefit based on how district allocates Medicaid revenue . Federal Medicaid Requirements Individual must be enrolled in Medicaid Service must be covered in state plan Schools: child referred by physician SLP/A must have CCC or equivalent SLP/A must maintain appropriate documentation including dates of service, name of recipient, person providing service, duration, medical justification and group vs. individual treatment EPSDT Requires states to provide screening for vision, dental, and hearing services Provide assessment of communication skills or language development focusing on expression, comprehension, and articulation EPSDT ( cont) Based on results states must provide services necessary to treat or ameliorate deficits, illnesses or conditions Administrative Claiming Besides payment for services (medical assistance), school districts can receive Medicaid reimbursement for: Identification and enrollment of eligible students Direct support to the provision of health care services Individual members have little access to administrative claiming funds Medicaid and IDEA funding Is this double dipping? No, Federal IDEA funds partially cover therapy services Medicaid must be primary to IDEA funds for health-related services Medicaid vs. IDEA funding – See: http://www.asha.org/practice/reimburseme nt/medicaid/IDEAMedicaid.htm State Medicaid Plans States are required to outline plan Centers for Medicare and Medicaid (CMS) reviews plan for conformity to Federal regulations Must offer services that are medically necessary State Medicaid Plan Each state has the authority to establish: Eligiblity standards Determine type, amount and frequency of services Set rates and administer the program State Medicaid Plan What does your state plan include: Collateral services Transportation costs In addition to direct health related services Medicaid fee schedule state-by-state KS Provider Home Page https://www.kmap-stateks.us/Public/provider.asp Kansas Medical Assistance Program https://www.kmap-state-ks.us/ Documentation and the Office of Inspector General (OIG) audits 20 state Medicaid school-based programs were audited between 2001-2010. See findings at: http://www.asha.org/practice/reimbursement /medicaid/oig_reports.htm Areas of concern to SLP/A Provider qualifications Documentation Each of the audits recommended refund of federal payments Recent Audit Results (2010) AZ and NJ audit results were released in early 2010 Arizona billed the federal government $32,212 for school-based Medicaid services (1/04-6/06) Based on OIG findings, it was recommended that $21.3 million be refunded due to the following reasons; Services not provided or overbilled Recent Audit Results (2010) Based on OIG findings, it was recommended that AZ refund $21.3 million. The following reasons were cited: Services not provided or overbilled Documentation requirements not met SLP provider requirements not met Lack of Prescription/referral Student eligibility requirements not met Recent Audit Results (2010) NJ findings were similar: The OIG sampled claims from 7/03 through 10/06. Of the 100 school-based claims 49 compiled with federal and state requriements and 51 did not. 19 claims had more than one deficiency. The OIG recommended that NJ refund $8,079,312 to the federal government Recent Audit Results (2010) Deficiencies were found in 4 areas: Claims had services not provided Claims lacked a referral or prescription Claims did not meet federal provider qualifications Claims were made for services not documented in the child’s plan Commonly Cited Billing Errors Lack of appropriate referral Lack of Qualified Providers Can be a physician or a qualified practitioner of the healing arts including SLPs Use of BA level practitioners without supervision Lack of or incomplete documentation Prevention of Billing Errors Ensure that a referral from an approved provider is obtained (An IEP alone is not an acceptable substitute for a referral) Ensure that child meets Medicaid eligibility Demonstrate that a qualified provider (maintain license or CCC) is used or document that the provider is under the supervision of a qualified SLP Prevention of Billing Errors (con’t) Ensure that time study forms represent actual activities performed Provide adequate documentation including: Name of recipient, medical justification, dates of service, person providing service (include credentials, ie., CCC), duration, and group vs. individual therapy Where does the Medicaid money go? Several states deposit in general fund Others to Special Education budget $$$ to districts does not guarantee access by SLP program Some to SLP budget To Advocate for $$ to SLP or Special Education budget you need to know: % to the district from the state % to Spec Ed % ( if any) to the SLP program Accessing Medicaid funding Assess your needs (what will the monies be used for) Know the decision makers Be proactive: Know what you want and how to get it Gain support of administrators and the unions Accessing Medicaid Funds (cont) Advocate for funds for materials and supplies, or back to providers as a bonus or for additional time worked Know % of students who are Medicaid eligible (on income and/or disability) Know how much money district SLPs generate for the district Medicaid funding success stories All SLP Medicaid funds go to SLP budget Pittsburgh Public Schools Salary increase based on additional work completing Medicaid documentation; Minneapolis Public Schools View successes at: http://www.asha.org/about/legislationadvocacy/schoolfundadv/default Resources: Center for Medicare and Medicaid directory of state plans: www.cms.hhs.gov/medicaid/consumer. asp ASHA’s Medicaid reimbursement resources: http://www.asha.org/members/issues/r eimbursement/reimbur-default Resources ASHA Summary of OIG reports: http://www.asha.org/practice/reimbursement /medicaid/SchoolBasedServicesSLP.htm Medicaid funding success stories: http://www.asha.org/about/legislationadvocacy/state/advocacy-schools.htm School Finance Committee Medicaid Resources: http://www.asha.org/advocacy/schoolfundad v/default.htm Questions ????