lecture_5_gastrointestinal_alteration_1
advertisement
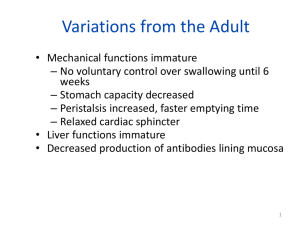
Alteration in Gastrointestinal Function Lecture 5 Part One 1 Functions of GI Tract 1. The child ingest and absorb food and fluid to sustain to life and promote growth. 2. Elimination of waste product is another role of GI tract. 2 Gastrointestinal Tract of a Child Esophagus and Stomach • The esophagus is continuous tube that allows food to pass to the stomach. • The stomach is located in LUQ , the role of the stomach is to store and to secrete enzyme and digestive juice that aid in digestion. 4 Pancreas • Functions 1. Digestive enzymes – digest proteins • Trypsin, Chymotrypsin – digest starch • Amylase 2. Buffers – neutralizes acid from stomach Liver • Function – Produces bile a. bile stored in gallbladder until needed breaks up fats – act like detergents to breakup fats Bile contains colors from old red blood cells collected in liver = iron in RBC rusts & makes feces brown Small intestine • Functions – Chemical digestion • major organ of digestion & absorption – Absorption through lining • Over 6 meters in adult • Small intestine has huge surface area = 300m2 • Structure – 3 sections • duodenum = most digestion • jejunum = absorption • ileum = absorption Large intestines (colon) Functions • Re-absorb water • > 90% of water reabsorbed • Vitamins K and B are reabsorbed with the water. Pediatric Differences 1. GI system is immature at birth. 2. Sucking and swallowing are automatic reflexes initially, gradually coming under voluntary control as the nerves and muscles develop by 6 weeks of age. 3. The newborn's stomach capacity is only 10 to 20 ml 4. It expands rapidly to 200 ml by one month of age and reaches adult capacity of 2000-3000 ml by late adolescence. 5. Gastric emptying time: – 2 to 3 hours in the newborn – 3 to 6 hours by one to two months of age. Pediatric Differences 6. Lower esophageal sphincter has a poor development of mucous membrane and muscular layer, its tone is decreased or relaxed. 7. Pyloric sphincter is developed well. • The fundus of stomach is under the left dome of diaphragm. 8. Gastroesophageal reflux and regurgitation is frequent in infants. 10 Pediatric Differences 9. Gastric acid secretionis deficient in several digestive enzymes that are usually not sufficient until 4-6 months of age. • Stomach pH is 5, comparing to 2 in adults. • ↓ pancreatic enzyme activity: – ↓ amylase, responsible for the initial digestion of carbohydrates, is insufficient resulting in an intolerance of starches. – If cereals are given before 4-6 months, the infant may develop gas and diarrhea. – lactase breaks down or hydrolyzes lactose. ↓ lactase level results in incomplete absorption of lactose, which can cause gas, abdominal distention, and diarrhea. – ↓ lipase, responsible for digestion and absorption of fats. Fat in breast milk is absorbed more readily than in formula because human milk contains lipase. 11 Pediatric Differences • The infant's first stool is meconium – sticky and greenish black. – composed of intrauterine debris, such as bile pigments, epithelial cells, fatty acids, mucus, blood, and amniotic fluid. – Passage of meconium should occur within the first 24 hours. • Transitional stools: – appear by the third day after the initiation of feedings. – greenish brown to yellowish brown in color, less sticky than meconium, and may contain some milk curds. • Typical milk stool: – is passed by the fourth day. – In breast-fed infants the stools are yellow to golden in color and pasty in consistency, with odor, similar to that of sour milk. – In infants fed cow's milk formula, the stools are pale yellow to light brown, are firmer in consistency, and have a more offensive odor. • Breast-fed infants usually have more stools than do bottle-fed infants. The stool pattern can vary widely; six stools a day may be normal for one infant, whereas a stool every other day may be normal for another. Pediatric Differences • The liver is also immature after the first few weeks of the life the liver is able to conjugate bilirubin and excrete bile. • The process of gluconeogenesis and plasma protien and ketone formation remain immature during the first year of life. 14 Diagnostic Test Abdominal computed tomography (CT scan) Abdominal magnetic resonance imaging (MRI) Abdomenal ultrasound Barium tests Liver functions tests (LFTs) Stool culture Gastrointestinal endoscopy A series of cross-sectional x-ray images that show abdominal organs Magnetic and radio waves create images of abdominal organs and tissues in all thre planes of the body Process of beaming sound waves into the abdomen to producec images of orans such as the gallbladder X-ray examinations using a liquid barium mixture to locate disorders of the gastrointestinal tract Measurements of liver enzymes and other stubstances in the blood Feces are placed in a growth medium (culture) to test for microoraganisms, such as bacteria Visual examination of the gastrointestinal tract with an endoscope 15 Cleft lip and Palate • • • • 1:2000 births – cleft palate 1: 700 birth cleft lip 20-30% will have other congenital defects A cleft lip happens if the tissue that makes up the lip does not join completely before birth. This causes an opening in the upper lip. • The opening can be a small slit or a large opening that goes through the lip into the nose. It can be on one or both sides of the lip or, rarely, in the middle of the lip. • Aspiration, family coping, altered nutrition, infection, ineffective breathing pattern, tissue integrity, (Parent) knowledge deficit • Cleft lip / palate can be unilateral and bilateral Cleft lip and Palate • Children with a cleft lip or a cleft palate often have problems with feeding and talking. They also might have ear infections, hearing loss, and problems with their teeth. • Often, surgery can close the lip and palate. Cleft lip surgery is usually done before age 12 months, and cleft palate surgery is done before 18 months. 19 Cleft lip and palate surgery • Cleft lip repair. The edges of the cleft between the lip and nose are cut (A and B). The bottom of the nostril is formed with suture (C). The upper part of the lip tissue is closed (D), and the stitches are extended down to close the opening entirely (E). Teaching plan for caregivers related to feeding an infant born with bilateral CL/CP. • • • • Anatomy and functioning of the palate Successful feeding techniques Breastfeeding can be accomplished If breastfeeding is unsuccessful, a breast pump may be used • Enlarging the nipple hole with a cross cut allows the infant to receive the formula in the back of the throat, bypassing the sucking problem • Stimulate sucking the lower lip by rubbing it with the nipple Teaching plan for caregivers related to feeding an infant born with bilateral CL/CP. • Place nipple in mouth and infant will swallow • Allow the infant to rest • Facial expressions will change before choking and gagging by elevation of eyebrows and wrinkling of forehead. • Remove nipple slowly and gently from mouth • Allow frequent rests • Allow infant to consume 3–4 ounces • Special nipples are available if needed • An asepto syringe can be used if infant is unable to ingest adequate amounts with nipple 24 • http://www.youtube.com/watch?v=vyP1A9odEs 25 Nursing care plan • Nursing Diagnosis: Risk for Aspiration (Breast Milk, Formula, or Mucus) related to anatomic defect • Goal : Prevention or minimization of risk factors in the patient at risk of aspiration • Nursing intervention: • Assess respiratory status and monitor vital signs at least every 2 hours. • Position on side after feedings. • Feed slowly and use adaptive equipment as needed. • Burp frequently (after every 15–30 mL of fluid). • Position upright for feedings. • Keep suction equipment and bulb syringe at bedside. 26 Nursing care plan Nursing Diagnosis: Ineffective Family Coping related to situational crisis of birth of a child with a defect. Goal: Facilitating family participation in the emotional and physical care of the child. Nursing intervention: • Help parents to hold the infant and facilitate feeding process. • Point out positive attributes of infant (hair, eyes, alertness, etc). • Explain surgical procedure and expected outcome. • Show pictures of other children’s cleft lip repair. • Assess parents knowledge of the defect, their degree of anxiety and level of discomfort. • Explore the reactions of extended family members. 27 Nursing care plan • Nursing Diagnosis: Altered Nutrition: Less Than Body Requirements related to the infant’s inability to ingest nutrients • • • • • • • • • • • Goal : Provision of a balanced dietary intake of foods and fluids. Nursing intervention: Assess fluid and calorie intake daily. Assess weight daily (same scale, same time, with infant completely undressed). Observe for any respiratory impairment. Provide 100–150 cal/kg/day and 100–130 mL/kg/day of feedings and fluid. increasing total fluids. Facilitate breastfeeding. Hold the infant in a semisitting position. Give the mother information on breastfeeding the infant with a cleft lip and/or palate 28 Nursing intervention: cont…. • Hold infant in an upright or semisitting position for feeding. • Place nipple against the inside cheek toward the back of the tongue. May need to use a premature nipple (slightly longer and softer than regular nipple with a larger opening) or a Brecht feeder (an oval bottle with a long, soft nipple). • Feed small amounts slowly. • Burp frequently, after 15–30 mL of formula has been given. • Initiate nasogastric feedings if the infant is unable to ingest sufficientcalories by mouth. 29 Tracheoesophageal Fistula and Esophageal Atresia • Tracheoesophageal fistula is an abnormal connection in one or more places between the esophagus and the trachea. • Tracheoesophageal fistula is also known as TE fistula or simply TEF • TE fistula is a birth defect, which occurs in 1 in 4,000 births. 30 Esophageal atresia • The esophagus does not form properly while the fetus is developing before birth, resulting in two segments; one part that connects to the throat, and the other part that connects to the stomach. However, the two segments do not connect to each other. 31 Esophageal Atresia & Tracheoesophageal Fistula Symptoms of TE fistula or esophageal atresia • • • • Frothy, white bubbles in the mouth Coughing or choking when feeding Vomiting Blue color of the skin (cyanosis), especially when the baby is feeding • Difficulty breathing • Very round, full abdomen 33 Treatment • Attempt NG placement, X-ray, echo, ultrasound – diagnostic tests • Surgical emergency – Surgery in several stages (TPN then G-tube) Very good prognosis 34 Nursing intervention • • • • Suctioning to remove secretion Position to keep patent airway Observe for signs of respiratory distress Keep the infant NPO, IV therapy 35 Pyloric Stenosis • Narrowing of pyloric sphincter (stomach to small intestine) – obstruction – 2-8 weeks old, gradual onset and severity of vomiting – projectile, jaundice possible, wt loss, dehydration, gastric peristaltic waves, alkalosis – Diagnose with an upper GI series – Make child NPO, monitor and replace needed fluid & electrolytes IV, NG to suction, surgery – Begin small, freq. feedings 4-6 hours following surgery Nursing management • • • • • Meet fluid and electrolyte need. Minimize wt loss. Promote rest and comfort. Prevention of infection. Provide supportive care. 38 Gastroesophageal reflux disorders GERD • 1:300 infants • Poor wt. gain (failure to thrive), respiratory problems, behavior problems, pain • Diagnose with clinical history, Upper GI series and endoscopy, pH probe, milk allergy testing • Tx depends on severity – Mild will tx like GER and resolve by 12-18 months – Severe may require medications and/or surgery (Nissen fundoplication) http://emedicine.medscape.com/article/1892517-overview#showall Gastroesophageal Reflux • Normally caused by an incompetent/poorly developed lower esophageal (cardiac) sphincter – very common ~50% of all infants • Peak at 1-4 months • Infants – reduce vol of feeding, thickening formula feeding (rice cereal – doesn’t work with BM), keep infant upright after feeding, smoke exposure elimination • Small , freq meals, limit contributing foods (acidic, caffeine, carbonated, peppermint, fatty), no food just before bed • Medications may be required intermittently or continuously The American Academy of Pediatrics recommends • Placing the infant with gastroesophageal reflux in the prone position. Eliminating these factors and placing the infant with reflux in the prone position is the safest position. http://www.naspghan.org/user-assets/Documents/pdf/PositionPapers/GERD.pdf