Laparoscopic Gastric Bypass - 3 Each / Case
advertisement

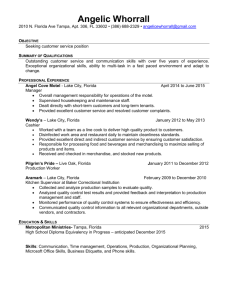
Avoiding Medical Malpractice Michele M. Cerullo, JD Assistant Attorney University of South Florida Office of the General Counsel An easy case: from www.amazon.com Laparoscopic Gastric Bypass - DYNJS0303 - Laparoscopic Gastric Bypass - 3 Each / Case by IS Distributed http://www.amazon.com/Laparoscopic-Gastric-Bypass-DYNJS0303-Each/dp/B000WCW4FK/ref=cm_cr_pr_product_top • • 92 of 92 people found the following review helpful ▫ 1.0 out of 5 stars Terrible instructions! February 2, 2010 ▫ By Ian C. Guch ▫ The instructions that come with this product are just terrible. Even though I did everything according to the book, I had about seven pieces left over. I'm sure they're useful for something, but I can't figure out what. 11 of 12 people found the following review helpful ▫ 1.0 out of 5 stars Completely Disappointing, September 26, 2011 ▫ By Silicon Valley Bob "bob41116" (San Jose, CA USA) - See all my reviews ▫ I've taken on other do-it-yourself projects, so I was disappointed with the instructions that accompanied this product. There's a lot of medical jibber-jabber--morbidity this, contraindications that--until I finally threw up my hands and sent the whole thing back. If they ever come up with a set of IKEA-like instructions, I'd be willing to give it another try. The Statistics • 2011 Harvard study – Most doctors in America will be sued at some point during their career More Statistics • The good news: A relatively small number of claims result in payments to patients or their families ▫ About 93% of all medical malpractice cases are resolved before trial (only 7% go in front of a jury) ▫ NEJM study: Of medical malpractice cases that make it to court trials, plaintiffs prevailed in 21% of verdicts, while settlementbased resolutions favored the plaintiff in 61% of cases ▫ NEJM study: Average compensation in medical malpractice claims to be about $485,000, with average jury awards after a verdict in court checking in at almost twice the average out-of-court settlement ($799,000 for jury awards and $462,000 for settlements). ▫ JAMA: The average compensation for medical malpractice that occurred in the inpatient setting was around $363,000, while the average award for healthcare mistakes in the outpatient setting was about $290,000. Inpatient Surgeries (2009 CDC) • Total number of procedures performed: 48.0 million • Number of selected procedures performed: • Arteriography and angiocardiography using contrast material: 1.9 million • Cardiac catheterizations: 1.1 million • Endoscopy of small intestine with or without biopsy: 1.1 million • Endoscopy of large intestine with or without biopsy: 525,000 • Computerized axial tomography (CAT scans): 497,000 • Diagnostic ultrasound: 902,000 • Balloon angioplasty of coronary artery or coronary atherectomy: 605,000 • Hysterectomy: 494,000 • Cesarean section:1.3 million • Reduction of fracture: 621,000 • Insertion of coronary artery stent: 528,000 • Coronary artery bypass graft: 415,000 • Total knee replacement: 676,000 • Total hip replacement: 327,000 The reality…. • The “Hassel Factor” ▫ Medical malpractice suits can take anywhere from 1 to 7 years to resolve ▫ Once the suit is filed, it takes an average of 27.5 months to reach resolution of a medical malpractice case through a negotiated settlement or through a jury verdict. Dissecting a case • The Parties: ▫ Plaintiff – “the complainer” also known as a claimant or complainant and the person or institution that initiates the lawsuit. ▫ Defendant – “I didn’t do it!” or a person or institution against whom an action is brought in a court of law; the person being sued or accused. ▫ Fact Witness – “I saw it all” or a person with knowledge about what happened in a particular case, who testifies in the case about what happened or what the facts are. ▫ Expert Witness – “I know it all” or a person who is a specialist in a subject, often technical, and qualified to present his/her expert opinion without having been a witness to any occurrence relating to the lawsuit or criminal case. ▫ The fact/expert witness? The Investigation • Reasonable investigation by the attorney filing the action to determine that there are grounds for a good faith belief that there has been negligence in the care or treatment of the claimant. • The complaint or initial pleading shall contain a certificate of counsel that such reasonable investigation gave rise to a good faith belief that grounds exist for an action against each named defendant. • Good faith may be shown to exist if the claimant or his or her counsel has received a written opinion, which shall not be subject to discovery by an opposing party, of an expert that there appears to be evidence of medical negligence. • If the court determines that such certificate of counsel was not made in good faith and that no justiciable issue was presented against a health care provider that fully cooperated in providing informal discovery, the court shall award attorney’s fees and taxable costs against claimant’s counsel, and shall submit the matter to The Florida Bar for disciplinary review of the attorney. ▫ Florida Statutes, 766.104 Presuit Notice and Exchange of Discovery • After completing the presuit investigation and prior to filing a complaint for medical negligence, a claimant shall notify each prospective defendant by certified mail, return receipt requested, of intent to initiate litigation for medical negligence. • Notice to each prospective defendant must include, if available, a list of all known health care providers seen by the claimant for the injuries complained of subsequent to the alleged act of negligence, all known health care providers during the 2-year period prior to the alleged act of negligence who treated or evaluated the claimant, copies of all of the medical records relied upon by the expert in signing the affidavit, and the executed authorization to release PHI. • The parties exchange information such as unsworn statements, document, physical and mental examinations. ▫ Florida Statutes, 766.106 Notice of Claim or Summons • A Notice of Claim or Summons is a legal notice indicating the beginning of a lawsuit. • If you receive a Notice of Claim/Suit, a Summons, or are named personally as a defendant in a lawsuit, contact the Self Insurance Program (SIP)/ Risk Management or the Office of the General Counsel immediately (813-974-8008). 11 UNITED STATES DISTRICT COURT MIDDLE DISTRICT OF FLORIDA SUMMONS IN A CIVIL ACTION Sue A. Lot, Plaintiff, CASE NUMBER: v. THE UNIVERSITY OF SOUTH FLORIDA BOARD OF TRUSTEES, Drs. Mistake and Trouble Defendants. (Name and Address of Defendant) THE UNIVERSITY OF SOUTH FLORIDA c/o (name) , Assistant General Counsel University of South Florida 4202 E. Fowler Avenue, ADM 250 Tampa, FL YOU ARE HEREBY SUMMONED and required to file with the Clerk of this Court and serve upon PLAINTIFF'S ATTORNEY (name and address) Anita Lexus Jag & Mercedes, P.A. 1234 E. 7th Ave., Suite 1000 P.O. Box 5551212 Tampa, FL 33675-7777 (813) 123-4567 an answer to the complaint which is herewith served upon you, within 20 days after service of this summons upon you, exclusive of the day of service. If you fail to do so, judgment by default will be taken against you for the relief demanded in the complaint. SHERYL L LOESCH AUG 2 9 2009 DATE CLERK BY DEPUTY CLERK The Complaint • Criminal Complaint - charges the person named or an unknown person with a particular offense. It states the facts that constitute the offense and must be supported by probable cause. • Civil Complaint - initiates a civil lawsuit by setting forth for the court a claim for relief from damages caused, or wrongful conduct engaged in, by the defendant. The complaint outlines all of the plaintiff's theories of relief, or causes of action (e.g., negligence, battery, assault), and the facts supporting each cause of action. Subpoena • • • • Subpoena for Deposition: testimony under oath Duces Tecum: bring records with you Without deposition: provide the records If patient records are request, be aware of HIPAA and contact the OGC • Call the attorney issuing the subpoena to coordinate a time, date and location for the deposition • Contact the OGC about an issues or questions that arise IN THE CIRCUIT COURT OF THE THIRTEENTH JUDICIAL CIRCUIT OF THE STATE OF FLORIDA IN AND FOR HILLSBOROUGH COUNTY CRIMINAL JUSTICE DIVISION State of Florida VS DEFENDANT DR. ALPHA SURGEON TAMPA GENERAL HOSPITAL 1 DAVIS BLVD TAMPA, FL 33606 CASE NO: 00-0000 SUBPOENA DIVISION: D Patient:_______________________ Date of Birth:___________________ By service of this subpoena, you are hereby commanded to appear for the purpose of giving truthful testimony in behalf of the STATE OF FLORIDA in a Jury Trial, wherein the STATE OF FLORIDA is plaintiff and the above named is defendant. You are called to appear for a period of time beginning at 8:00am., the week of the 16th day of July, 2011, before JUDGE ______________, in courtroom #23, Third Floor, of the HILLSBOROUGH COUNTY COURTHOUSE ANNEX, NORTH TOWER, 801 East Twiggs Street, Tampa, Florida. Pursuant to Section 914.03, Florida Statutes, this subpoena shall remain in full force and effect until disposition of the cause or until you are excused by the Court. *****IMPORTANT***** UPON RECEIPT OF THIS SUBPOENA AND PRIOR TO THE COURT DATE ABOVE, CONTACT THE WITNESS AID CENTER AT (813) 272-5050, TO CONFIRM THE DATE AND RECEIVE NOTIFICATION OF ANY CHANGES, CONTINUANCES, OR SPECIAL INSTRUCTIONS. IN ACCORDANCE WITH THE AMERICANS WITH DISABILITIES ACT, PERSONS NEEDING A SPECIAL ACCOMMODATION TO PARTICIPATE IN THIS JURY TRIAL SHOULD CONTACT 272-5050, NOT LATER THAN SEVEN (7) DAYS PRIOR TO THE PROCEEDING OR VIA FLORIDA RELAY SERVICE FOR THE HEARING IMPAIRED AT 1-800-995-8770 (TDD-TTY). DATED, this 29th day of June, 2011. MARK A. OBER STATE ATTORNEY 13TH JUDICIAL CIRCUIT RETURN INFORMATION INDIVIDUAL SERVICE ON NAMED PERSON SUBSTITUTE SERVICE BY SERVING: ASSISTANT STATE ATTORNEY NON-SERVICE FOR THE FOLLOWING REASON: FLA BAR* REASON: SCOTT HARMON/vlm 2001-106037-0021 DATE: FOR THE COURT DEPUTY SHERIFF-PROCESS SERVER STATE OF FLORIDA DIVISION OF ADMINISTRATIVE HEARINGS OFFICE OF THE JUDGE OF COMPENSATION CLAIMS ST. PETERSBURG EMPLOYEE: EMPLOYER/CARRIER: CLAIM NUMBER: xxxxx-xxxxx-xx DATE OF ACCIDENT: 02/13/09 SUBPOENA DUCES TECUM FOR DEPOSITION THE STATE OF FLORIDA: TO: Will Sueyou, M.D. USF / Department of Neurology College of Medicine Health & Sciences Bldg. 12901 Bruce B. Downs Blvd., Room #2128 Tampa, FL 33612 YOU ARE HEREBY COMMANDED to appear before a person authorized by law to take depositions at: USF / Department of Neurology, College of Medicine, Health & Sciences Bldg., 12901 Bruce B. Downs Blvd., Room #2128, Tampa, FL 33612 on August 16,2011, at 2:00 p.m., for the taking of your deposition in this action, and to have with you at that time and place the following: Copies of the entire medical file, including, but not limited to, any and all medical records, reports, x-rays, narratives, bills, et cetera, in your custody and control concerning any and all care, treatment and examination rendered to , SS#: , D.O.B: If you fail to appear, you may be in contempt of Court. You are subpoenaed to appear by the following attorneys and unless otherwise excused from this subpoena by these attorneys or the Court, you shall respond to this subpoena as directed. Herein fail not. A true copy. Sheriff Given under my hand and seal, at Clearwater, Florida, this I 4 day of June, 2010. Mr. Attorney, Esquire For the Court SAM SNIDE, ESQUIRE Snide, Snide & Snide, PCA. P.O. Box 5555 Clearwater, FL 33766 Fla. Bar #0000000 Attorney for Employer/Carrier Attendance • Subpoena for Trial: You must attend unless excused. You may face a motion for contempt of court if you choose to ignore the subpoena. • Contact the Witness Center or issuer to schedule a date and time for your appearance at trial. • Provide a contact number, including an after hours phone or pager number to minimize your inconvenience. • Federal courthouse: must have id and no electronic devices. • State courthouse: electronic devices are permitted. Contact With Attorneys • If you receive a telephone call from an attorney who does not work for USF or if you are unsure whether the attorney works for USF, you do NOT have to speak with the attorney. Refer the caller to the USF Office of the General Counsel at (813)974-2131. • You are not permitted under HIPAA to discuss you patients with outside attorneys or law enforcement unless certain documentation has been provided. Served With Letters or Court Papers • Court papers (subpoenas, summons, etc.) should be served at the Office of the General Counsel and will be forwarded to you from the OGC either by fax or email to your USF Health email account. Always refer process servers to 4202 E. Fowler Avenue, CGS 301 to serve court papers. • HOWEVER, if you are personally served with any court papers or letters from a non-USF attorney, fax the papers on the day you receive them to (813)974-5236 (USF Policy 0-103). You may also contact the Office of the General Counsel at (813)974-2131 and ask to speak with an attorney. • Please check voice mail, mail and (USF Health) email regularly. If you are out for more than a few days-make sure someone checks your mail and you turn on your “out of office assistant” on in your email. Med Mal - Deviation from the standard • The National Standard of Care: requires a doctor to use the degree of skill and care of a reasonably competent practitioner in his field under same or similar circumstances • The Locality Rule: requires a doctor to have the reasonable caliber of skill and knowledge that is generally possessed by surgeons and physicians in the locality where he or she practices • The Respectable Minority Rule: where the doctor did not follow the same course of therapy that other doctors would have followed, he can show that his course is accepted by a respectable minority of practitioners The standard - Florida • Prevailing professional standard of care - level of care, skill, and treatment which, in light of all relevant surrounding circumstances, is recognized as acceptable and appropriate by reasonably prudent similar health care providers • ED standard – reckless disregard The formula • Duty (physician-patient relationship) + • Breach of duty (failure to meet the required standard of care) + • Causation (breached caused patient’s injury) + • Damages = • LIABILITY Top 10 Medical Malpractice Claims * according to one author • • • • • • • • • • Medication Errors Diagnosis Failures Negligent Supervision Delayed Treatment Failure to Obtain Patient Consent Lack of proper credentialing or technical skill Unexpected death Infections Pain, suffering and emotional distress Lack of Teamwork and Communication Prevention. The easy steps… • The Physician/Patient Relationship • August 2010 Florida Medical Business ▫ Front cover “Listen Up! People Sue Less When You Hear More.” • Malcolm Gladwell, Blink: ▫ “The overwhelming number of people who suffer an injury due to the negligence of a doctor never file a malpractice suit at all. Patients don’t file lawsuits because they’ve been harmed by shoddy medical care. Patients file lawsuits because they’ve been harmed by shoddy medical care and something else happens to them.” ▫ “What comes up again and again in malpractice cases is that patients say they were rushed or ignored or treated poorly.” 1997 Study (Wendy Levinson, MD) • Levinson recorded hundreds of conversations between a group of physicians and their patients. Half of the doctors had never been sued, and the other half had been sued at least twice. • Levinson found that just on the basis of those recorded conversations alone, she could find clear differences between the two groups: ▫ ▫ ▫ ▫ The doctors who had never been sued spent more than three minutes longer with each patient than those who had been sued did (18.3 minutes versus 15 minutes). They were more likely to make “orienting” comments, such as “First I’ll examine you, and then we will talk the problem over” or “I will leave time for your questions.” They were more likely to engage in active listening, saying things such as “Go on, tell me more about that.” They were far more likely to laugh and be funny during the visit. • Levinson reported no difference in the amount or quality of information doctors gave their patients; the never-sued doctors didn’t provide more details about medication or the patient’s condition. • The difference was entirely in how they talked to their patients. “Listen! (And be liked)… ▫ “People are reluctant to sue people they like, and people like people that listen to them.” How to listen better: Reflective feedback- ask questions, make statement or offer cues that show you understand, agree or don’t understand Silence – focus on what is being said Listen with your eyes Positioning Allow the extremely emotional person to speak The easy steps…. • Teamwork and team communication • The team includes: patients, nurses, referring and consulting physicians, laboratories and more • Keep the communication lines open with the team • Watch for disruptive behavior and report it What is disruptive behavior? “It is the health care equivalent of road rage.” Dr. Peter B. Angood, Chief Patient Safety Officer at the Join Commission Who does it? What it looks like? • Leading offenders: High Specialty Fields • Medical conditions (beware of the Americans with Disabilities Act) • Harassment, including sexual harassment • Discrimination • Retaliation • Defamation • Violations of HIPAA and patient privacy • Unprofessionalism • JUST PLAIN OLD BAD BEHAVIOR Disruptive Doctors and Medical Care • Survey of health care workers at 102 nonprofit hospitals from 2004-2007 ▫ 67% of respondents believed there is a link between disruptive behavior and medical mistakes ▫ 18% KNEW of a mistake that occurred because of disruptive behavior • 40% of hospital staff have been so intimidated by a physician they did not share concerns about orders for medication that appeared to be incorrect – 7% contributed to a medical error Laurie Tarkan, Arrogant, Abusive and Disruptive — and a Doctor, New York Times, December 1, 2008 January 1, 2009 Joint Commission Standard • Activities considered under the new standard are verbal outbursts, condescending attitudes, refusing to take part in assigned duties and making physical threats, based on the Joint Commission’s belief that these behaviors have a negative effect on communication, collaboration and teamwork vital to a good patient care environment. • Zero tolerance policy, involvement and support from physician leaders, and reducing fears of retribution if a physician reports a colleague for this type of behavior Other pitfalls… • • • • • • • • • Documenting Medical Records History Follow-up Patient education Informed consent Informed refusal Labs Documenting prescriptions Leaving foreign objects in a patient? Surgery on the wrong body part? Weak Medical Record • If it is not in the record, it did not happen • Adequate explanation in the record of what the doctor did or did not do. Must include the physician’s rationale for critical decisions, facts must be correct, and the record should not contain unresolved contradictions. The medical record should be appropriately altered should something need to be changed. • DO NOT alter the medical record after you receive a notice of intent, subpoena or other legal document. Medical records must be… • contemporaneous, accurate, truthful, and appropriate • HOW? ▫ ▫ ▫ ▫ ▫ ▫ Be honest and careful how entries are changed Be objective Be specific Be legible Be competent Watch for patient cues History and Follow-up care • Medical history must be elicited and documented • Incomplete histories delay diagnosis; medication errors can occur • Medical issues identified one on visit are not followed up on subsequent visits ▫ If action is deferred document why ▫ Always re-visit medical issues ▫ Document any courses of action or resolutions to the medical issue Patient Education • Adequate education of the procedure, treatment, or referral • Oral education with documentation (adequate?) • Formal consent process and informed refusal process • Written documentation ▫ Providing the written consent in advance ▫ Providing written educational documents Patient Consent (a growing problem) • What does consent look like? • Written ▫ Patient explained about the right and obligation to make informed decisions concerning patient’s care ▫ Description of the treatment/procedure ▫ Risks and side effects of the treatment/procedure ▫ Benefits of the treatment/procedure ▫ Alternatives to the treatment/procedure ▫ Risks and benefits to not undergoing or receiving the treatment/procedure ▫ Patient responsibilities ▫ Photographs and recordings Informed refusal • Written • Patients have the right to decline any treatment, procedures or referrals. • Physicians are obliged to explain the possible consequences of refusal. Labs and Prescriptions • Diagnostic lab and imaging tests are not received in a timely manner or acted upon. • Must have an effective system for keeping track of and reviewing labs and medications. Mistakes Happen • Report to USF’s Self-Insurance Program ▫ 974-8008 • Address it with the patient Case study • March 6,2001, 1:40 pm: 22 year old Maeurer was admitted by Khoury to the ER for a severe asthma attack and seen by Levine • 3:00 pm: Maeurer was incubated and was in a severe state of respiratory acidosis; carbon dioxide level of 90 and blood PH of 7.03 • Transferred to ICU and examined by Conetta and Iakovou; pupils were reactive to light and she could see; put on respirator and in an induced coma • Between March 6-18 anemia developed • March 18: X-ray shows a collapsed lung • Tubes inserted to inflate Maeurer’s lungs three times causing episodes of oxygen desaturation • April 10: Maeurer transferred to a different hospital where MRI and CT scans indicated blindness and brain infarcts Does it matter? • 13 hours after X-ray was taken, the collapsed lung was treated because Conetta stated he was not notified of the condition • Conetta took an x-ray and knew Maeurer was blind but never notified the attending • The resident claimed during a deposition that they believed Maeurer may have been given too much Norocuron and the residents contacted the manufacturer about signs of an OD Does it matter? • BUT at trial the residents testified they did not communicate with the manufacturer or think Maeurer was given too much Norocuron • Between March 7 and March 18, there is not a single entry that the patients pupils were checked? Would it have mattered? Facts not in evidence • A drug that was administered to the patient was recently part of a study? • The study was published (1 day before? 1 week before? 1 month before? 1 year before?) the patient was treated? The result • Suit for delayed intubation; delayed treatment of the collapsed lung and anemia AND LACK OF physician supervision and communication • Information gap between attendings and residents • Losses for: total blindness; pain and suffering; economic loss; loss of future wages The breakdown • A settlement of $750,000 was negotiated with Khoury • A settlement of $1,950,000 was negotiated with Levine and the hospital • Liability apportionment ▫ ▫ ▫ ▫ 35% Conetta 30% for Hospital 20% Iakovou 15% Levine Apologies - The American Medical Association Code of Medical Ethics • When a patient suffers significant medical complications that may have resulted from the physician's mistake or judgment, the physician is ethically required to disclose to the patient all the facts necessary to ensure understanding of what has occurred. • A physician's concern about legal liability that might result from full disclosure should not affect his or her decision to deal candidly with a patient. Apology Law – Florida Hospital Duty to Inform Patients • An appropriately trained person designated by each hospital • Inform the patient, in person about adverse incidents that result in serious harm to the patient • Notification of outcomes of care that result in harm to the patient do not constitute an acknowledgment or admission of liability, or can introduced as evidence. Apology Law - Florida 90.4026 Statements expressing sympathy; admissibility; definitions.— (1) As used in this section: • (a) “Accident” means an occurrence resulting in injury or death to one or more persons which is not the result of willful action by a party. • (b) “Benevolent gestures” means actions that convey a sense of compassion or commiseration emanating from human impulses. • (c) “Family” means the spouse, parent, grandparent, stepmother, stepfather, child, grandchild, brother, sister, half-brother, half-sister, adopted child of parent, or spouse’s parent of an injured party. (2) The portion of statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering, or death of a person involved in an accident and made to that person or to the family of that person shall be inadmissible as evidence in a civil action. A statement of fault, however, which is part of, or in addition to, any of the above shall be admissible pursuant to this section. How to apologize • Get ready – know the facts and be prepared to answer questions • Find a suitable location, quiet and free from distractions • Listen and empathize • Explain the facts • Apologize –say your sorry • Explain your role • Discuss next steps Other ramifications • Certification • Licensure Most Importantly….. • Contact the General Counsel’s office with any questions or concerns. • (813) 974-2131 • http://generalcounsel.usf.edu/