AMH in pre-pubertal girls Crisosto et al, JCEM, 2007
advertisement

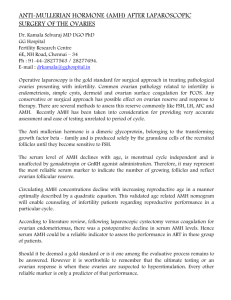
Moustafa Eissa MD FRCOG Cyberjaya University College of Medical Sciences, Malaysia In this subject facts are disperse and hypotheses and speculations are the majority Anti Mullerian Hormone (AMH) is a dimeric glycoprotein. It is secreted from granulosa cells of antral and preantral follicles. (Pepinsky et al 1988). Its expression in females starts as early as 32 weeks of gestational age (Rajpert-DeMeyts et al 1999) It is secreted from granulosa cells of antral and preantral follicles before selection for dominance. It's secretion declines in preovulatory follicles (Durlinger et al 2002). This is a widely accepted fact. However, in a study done by our group comparing AMH level in follicular fluid (FF) and serum in a study group of dysfunctional ovulation cysts and a control group of mature graffian follicles, we found high levels of AMH and it was not declining (Table 1). There was a strong correlation between follicular and serum AMH in the study group and inverse significant correlation between AMH (FF) and serum FSH (Figure 1). (Eissa et al 2013) Table (1): Hormonal profile in Control and Cyst formation groups. *FF: follicular fluid (means follicular fluid in group 1 and cyst fluid in group 2). Group 1 Control (n= 10) Mean ± SD Group 2 Study (Cyst) (n= 25) Mean ± SD Serum FSH(ng\ml) 4.65±1.5 5.41±1.9 0.2 (NS) Serum AMH(ng\ml) 5.9±2.02 14.6±3.3 0.0001(S) FF* AMH (ng\ml) 29.5±25.7 440.7±182.9 0.0001(S) FF* Testosterones(ng\ml) 5.8±4.2 5.2±3.7 0.6(NS) FF* Estradiol(ng\ml) 21.2±0.6 20.4±6.8 0.7(NS) Hormone P value Figure (1) correlation between serum and follicular fluid concentration of AMH in cyst group r= - 0.65 p= 0.0001 Serum FSH (ng/ml) 8.00 6.00 4.00 2.00 0.00 300.00 600.00 900.00 Intrafollicular AMH (ng/ml) 1200.00 1500.00 Polycystic Ovarian Syndrome (PCOS) is one of the most common endocrinopathies affecting 5-10% of women of reproductive age. (Amer 2006) PCOS is a multifactorial complex characterized by chronic anovulation, polycystic ovarian appearance, biochemical and clinical manifestations of hyperandrogenism. Figure (2 and 3). (Rotterdam Consensus 2004). Figure 2 Figure 3 The cause of anovulation in PCOS patients Stein & Leventhal (1935): the sclerocystic thickened capsule is the primary cause of anovulation Amer (2006): chronic anovulation is the result of abnormal folliculogenesis and steroidogenesis. Homburg et al (2009): the basic lesion is excessive secretion of androgens. Hyperinsulinaemia and high LH exacerbate the problem. La Marca et al (2009): The failure to find a causative gene, although its familial nature, suggested a developmental theory based on Barker theory. The excessive exposure to androgens in utero of rhesus monkeys programs the offending genes. This theory is not proved in human yet. (Abbott et al 2002). So it is now known that the main pathology of PCOS lies in the ovaries itself and the excessive production of androgens by the ovaries is the main endocrinological disturbance. However, insulin resistance and hyperinsulinaemia and increased LH secretion play a role in the pathogenesis of PCOS. Figure (4) (Homburg and Crawford 2014) Figure 4 Laparoscopic PCOS drilling Figure 5 Figure 6 Laparoscopic ovarian drilling Figure 7 Numerous theories of the aetiology of the associated anovulation have been speculated as hyperandrogenaemia, hyperinsulinaemia and dysfunctional feedback mechanism However, there is no clear evidence that excessive insulin or androgen has a direct inhibitory effect on ovulation. While there is a good correlation between severity of hyperandrogenemia and anovulation, there is no clear evidence that excessive androgen inhibit ovulation. (Homburg and Crawford 2014). Also, there is no convincing evidence that insulin has an inhibitory effect on ovulation. The dysfunctional feedback mechanisms are widely thought to be secondary to the primary pathophysiological change in the ovary itself (Franks et al 2006). AMH and anovulation in PCOS patients In PCOS patients, ovaries have large number of pre-antral and small antral follicles compared to normal ovary, the concentration of AMH is markedly increased compared to the control. (Pigny et al 2006). Since in vivo and in vitro studies showed that growth of the primordial follicles to growing follicles occurs in absence of AMH (Durlinger 2001), so this is may be the main role of AMH to prevent the growth of primordial follicles and prevent exhaustion of primordial follicle pool. Hence ovarian aging may be delayed in women with PCOS since high AMH levels may inhibit the selection and growth of primordial follicles (Mulders et al 2004). This may be the initial step of understanding the causative relationship of AMH to anovulation in PCOS patients. On the other hand and in normal ovary, the growing follicles (>10mm) are deprived of AMH, so they become more responsive to circulating FSH and follicle selection occurs. (Pellatt et al 2007). In studies of McGee and Hsueh (2000) and Durlinger et al (1999), it was found that AMH decreases the sensitivity of growing follicles to the secreted FSH. These studies are not proved in humans and further studies are needed. Kevenaar et al (2007) suggested a role of AMH in FSH induced steriodogenesis in human. This may explain the high oestradiol and the normal or relatively subnormal level of FSH in PCOS patients. The main pathophysiological disturbance of failure of ovulation in PCOS patients leads to accumulation of pre-antral and antral follicles and increased secretion of AMH. So, this in a vicious circle, leads to further anovulation. (Wang et al 2007). Level of AMH, although, high in PCOS patients, it depends on the severity of the condition. The density of pre-antral follicles is six times in amenorrheic PCOS patients compared with the normal ovary (Webber et al, 2003). It’s concentration in amenorrheic PCOS is high compared to oligomenorrheic and regularly menstruating patients (La Marca et al 2009) Also, it is higher in insulin resistant PCOS patients than insulin sensitive patients. These findings may strengthen the role of AMH in causing anovulation in PCOS patients. (Fleming et al 2006). Role of AMH in diagnosis and monitoring treatment of PCOS patients AMH measurement is useful in diagnosis and monitoring treatment in PCOS patients with high sensitivity and specificity. . In absence of ultrasound diagnosis, measurement of AMH might be used accurately in diagnosis of PCOS. (Pigny et al 2006) PCOS women with high circulating AMH (≥ 3.4 ng/mL) seem to be resistant to CC and may require a higher starting dose (Mahran et al 2013). PCOS women with markedly raised circulating AMH seem to be resistant to HMG ovulation induction and may require a higher starting dose. The good response seems to be inversely proportional to AMH level (Figure 6). (Amer et al 2013). Figure (8) Good response rates in 34 cycles of HMG ovarian stimulation in PCOS women with different serum AMH levels .Amer et al 2013 Conclusion Further studies are needed to know if this high AMH in PCOS patients is a result of the accumulation of small antral follicles because of the failure of ovulation or it is a cause of disruption of folliculogenesis. If this proved in humans an AMH antagonist may be the key treatment. The use of AMH measurement in evaluation of PCOS patients need a large and well designed trial. More studies are needed to evaluate the role of measuring AMH in adolescent girls to identify those at high risk for developing PCOS. Also, further studies are needed to identify those who may respond to treatment as weight loss, clomiphene citrate and insulin desensitizers. Thank you