Ms Helen Welch - Welsh Pain Society
advertisement

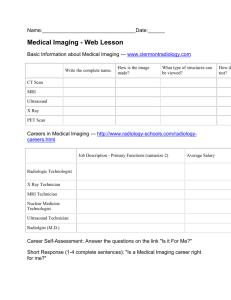
MSKTriage – Multidisciplinary working in action Purpose of triage The prioritization of care based on • illness • Injury • Severity • Prognosis • Resources available • Managing patient / healthcare professional expectation Types of triage in MSK • NHS Telephone triage • A&E • Multidisciplinary triage services • Paper based questionnaire triage : Startback • Computerized on line triage Benefits of triage model •Waiting list management •Stratified care approach targeting resources to demand •Fits with WAG models of “right place, right person, right time” •Reinforcing public health messages •Multidisciplinary working Does it work? •Daker-White et al. designed a randomized clinical trial (RCT) in a British orthopaedic clinic, comparing APP care to orthopaedic surgeons in training and found that APPs were as effective as junior doctors to treat patients with musculoskeletal disorders while ordering less diagnostic tests and reducing direct medical costs. Patient satisfaction was also higher for the APP care. •Other studies have looked at diagnostic validity and diagnostic concordance between APPs and surgeons for patients seen in an outpatient orthopaedic clinic and have found that for diagnosis and for determining whether patients would benefit from conservative care or surgical review, agreement may range from good to excellent (range κ = 0.69 to 1.00) (Aiken et al, 2008, Mackay et al, 2009) • Treatment recommendations agreement is fair to very good (range κ = 0.52 to 0.70) (Aiken and McColl, 2009) Cwm Taff ESP CMATS physio experience Out of 2909 cases seen since Dec 2013 • 386 referred to secondary care for surgical opinion (13.26%) • 34 referred to rheumatology • 119 referred to pain clinic • 937 referred to physiotherapy • Out of known outcomes of patients referred to secondary care for surgical opinion over 76% where converted to actual surgery Patient satisfaction on Extended Scope Physiotherapy (ESP) Musculoskeletal triage. H Welch (Cym Taff NHS Trust), G Paul-Taylor, R John Physiotherapy Department , Cwm Taf Health Board, Prince Charles hospital, Merthyr Tydfil, Wales Aims/introduction Results/graphs/illustration To evaluate: •the patient experience of patients referred to the ESP •patients’ expectations and satisfaction of the service To identify: •the demographic data of the patients Mean age range 40-59 yrs (range 20 -70yrs). 50% >1 year duration of symptoms. 94% rated the service provided as good - excellent. 88% of patient’s reported that they were happy to be assessed by the ESP. Graph of patients rating of overall experience?: Materials and methods A prospective audit of 50 new patients to the ESP service over a 3 month period between Dec 2008 and Feb 2009. Patients completed an anonymous self administered satisfaction survey following their initial appointment. Data was analysed with descriptive statistics. 100% References 88% 90% 80% 70% 60% 50% 40% 30% 20% 6% 10% 6% 0% 0% 0% 0% Excellent Conclusions The ESP service in Cwm Taff Health board achieves a high level of patient satisfaction. Good Average Poor Very Poor Not Documented 96% agreed they were able to discuss their treatment openly with only 10% preferring to see a Doctor. Dawson, Ghazi. The experience of physiotherapy extended scope practitioners in orthopaedic outpatient clinics. Physiotherapy. Vol. 90. 4. 210216. Poster No. GP149 Triage / Assesment The key to finding a remedy to a problem is the accurate recognition of the problem. Why is it important?? Failure to correctly identify an appropriate diagnosis can lead to:•Negative outcomes (Trowbridge 2008) •Delays in appropriate treatment (Whiting et al, 2008) •Unnecessary healthcare costs (Dohrenend and Skillings) What do we use to triage and determine care Three diagnostic questions when addressing a patient •The first question of diagnosis : are the patients symptoms reflective of a viseral or serious or potentially life threatening disorder •The second question of diagnosis : from where is the patients pain arising •The third question of diagnosis: What has gone wrong with this person as a whole that would cause the pain experience to develop and persist Murphy and Hurwitz (2007) Problems with diagnostic triage Can you algorise all conditions? Mostly done on LBP due to economic cost of condition. STarT Back The Keele STarT Back Screening Tool (SBST) is a brief validated tool (Hill et al 2008), designed to screen primary care patients with low back pain for prognostic indicators that are relevant to initial decision making. The STarT Back trial which was recently published in The Lancet (see references) was designed to compare the clinical and cost effectiveness of a stratified management approach; allocating patients to different treatment pathways based on their prognosis i.e. low, medium, or high risk of poor outcome. The tool helps primary care clinicians (GPs, physiotherapists etc) to group patients into 3 categories of risk of poor outcome (persistent disabling symptoms) - low, medium, and high-risk. By being able to categorise patients into these 3 groups, clinicians are then able to target interventions to each sub-group of patients to help improve outcome. Some problems with interpretation of High risk High risk does not mean hands off. High risk means more complex patients and a higher level of knowledge and skills needed to treat with a combined psychologically informed hands on approach (Hill, 2013) Practical use for STarTBack GPs (for those patients at low risk of poor outcome) or referral to primary care physiotherapists who can apply physiotherapy approaches to addressing pain and disability (for those at medium risk) and additional cognitive-behavioural approaches to help address psychological and social obstacles to recovery (for those at high risk) . IMPaCT Back study See STarTback web page for more details Problem? – can we rely on objective tests Limited quality research done on diagnostician utility of physical tests • The majority of clinical special tests of the lumbar and cervical spine have demonstrated poor diagnostic value • Should we think of them as driving decision making and determining prognosis rather than making a diagnosis of a superficial condition • Should we be thinking of them as screening tests rather than diagnostic tests? What makes a clinical test a “Best Test” •Reliable •Clinical utility •Validated finding high diagnostic accuracy Diagnostic accuracy Sensitivity Likelihood ratio’s Percentage of people who test positive for a specific disease among a group of people who have the disease A value of > or equal to 1 rules in a diagnosis Specificity Percentage of people who test negative for a specific disease among a group of people who do not have the disease A value closer to 0 rules out Simple rule Just remember High sensitivity and low likelihood ratio to rule out High specificity and high likelihood ratio to rule in Luckily The more serious and sinister the pathology the more sensitive and specific the tests get to providing an accurate diagnosis. Problem? Pathologies will present differently according to stage and chronicity of disorder Problem? Patients presentation and radiological findings often do not correlate. MR imaging examinations of the lumbar spine frequently reveal numerous findings, including disk desiccation, height loss, or bulging, with questionable relevance to patient symptoms. These findings are common in asymptomatic adults, with prevalence in this group as high as 90% (boden et al,1990, Jarvik at al, 2001, Jenson et al, 1994) Moreover, multiple studies have failed to demonstrate clinical benefit with the use of early MR imaging for LBP compared with radiographs alone or no imaging at all; furthermore, the imaging results may negatively affect patients’ sense of well-being (Jarvik,2003, Modic et al, 2005, Ash et al, 2008) Can we do anything to reduce anxiety with abnormal MRI findings •In patients •Healthcare professionals Lumbar MR Imaging and Reporting Epidemiology: Do Epidemiologic Data in Reports Affect Clinical Management? Brendan J. McCullough, MD, PhD, , Germaine R. Johnson, MD, , Brook I. Martin, PhD, MPH, and , Jeffrey G. Jarvik, MD, MPH In this study, patients with LBP or radiculopathy were less likely to receive a prescription for narcotics by primary care providers after lumbar spine MR imaging if the imaging report included a simple statement describing the prevalence of common findings in asymptomatic individuals. Similar trends were observed for repeat cross-sectional imaging and physical therapy referrals, although the differences were not statistically significant. Taken together, these findings suggest primary care providers were more reserved in their treatment of patients whose MR imaging report included the statement. Summary of potential problem :Errors in diagnosis • Confirmation bias • Poor diagnostic thinking process • Over reliance on objective assessment • Non descript conditions that have little or no unique manifestations • Weakness is the clinical tools • Bias of reporting of clinical tools in literature and clinical practice So what are essential the components of a triage assessment • Well performed history • Physical examination • Addition tests - bloods / radiological investigations – if needed Is there anything else that can help us to determine pathway of care Can we use a mechanism based classification of pain • Can account for variations in clinical presentation • use a cluster of symptoms and signs characteristic to each category • Good consenus of opinion on characteristics of pain mechanisms (Smart et al, 2009) research Smart, Blake , Staines and doody (2009) Clinical indicators of nociceptive, peripheral neurogenic and central mechanism of MSK pain : a Delphi survey of expert clinicians 3 round Delphi of 103 experts. Nociceptive Ranked in order of agreement • Clear, proportionate mechanical / anatomical nature to agg and easing factors • Pain associated with and in proportion to trauma or pathological process or movement / postural dysfunction • Pain localised to area of injury / dysfunction • Responsive to simple NSAIDs or analgesia • Usually intermittent and sharp with movement / mechanical provocation. • May be constant dull ache / throb at rest • Associated with other fractures of inflammation • Recent onset Nociceptive clinical examination • Clear, consistent and proportionate mechanical / anatomical pattern of pain reproduction on movement / mechanical testing of target tissue • Localised pain on palpation • Absence of unexpected findings • Antalgic Peripheral neurogenic • Pain described as burning, shooting, sharp, aching or electric shock • History of nerve injury • Pain in associated with other neurological symptoms • More responsive to anti epileptic and anti depressants than to NSAID • Pain of high severity / irritability • Mechanical pattern to agg and easing - load or compression neural tissues • Pain in association with other dysesthesia • Reports so spontaneous pain Peripheral neurogenic : clinical indicators • Pain / symptoms associated with tests that load or compress neural tissue • Pain on palpation of neural tissues • Positive neurological findings • Positive findings of hyperalgesia • Ant align posturing of affected body part. Central pain • Disproportionate , non mechanical, unpredictable pattern of pain provocation in response to multiple non specific agg/easing factors • Pain persisting beyond expected tissue healing time • Pain disproportionate to nature / extent of injury • Widespread non anatomical distribution of pain • History of failed interventions • Strong association with maladaptive psychosocial factors • More responsive to anti epileptic and anti depressants than to NSAID • Constant unremitting pain • Night pain / disturbed sleep • Pain in association with other dysesthesia • Pain of high severity and irritability Central pain : clinical indicators • Disproportionate inconsistent non mechanical non anatomical pattern of pain provocation in response to testing • Positive findings of hyperalgesia, allodynea and hyperpathia • Diffuse non anatomical area of pain • Positive identification of various psychosocial factors 1 :Reasoning of pain as related to aspects of the physical examination of patients • What am I going to choose in my physical examination to reproduce it Tests of nerve trunk mechanosensitvitiy Peripheral neurogenic Tests of neurological deficit LANNS 2: Reasoning of pain related to reasoning surrounding physio therapeutic or medical interventions Advice & Self management Therapy & Rehabilitation • How am I going to treat this Chronic pain services surgery Gp management Reasoning of pain related to concurrent thinking concerning a patient's prognosis or outcome • How long it may take to settle Reasoning of pain related to patient communication • How do I communicate with the patient the management plan and explanation of their symptoms remember diagnosis is not an event but a process Rule out sinister problems Identify the appropriate location Identify other contributors to the condition Then matching to resources • Reorganization of services • Improved links from secondary to primary care • Public health message • Training for development for triage posts • Psychosocial resources – pain management programes / pain clinic