Day Care Infections - Virginia Head Start Association, Inc.
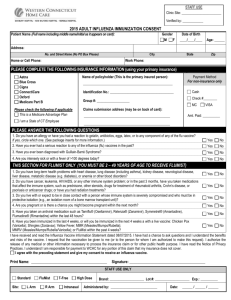
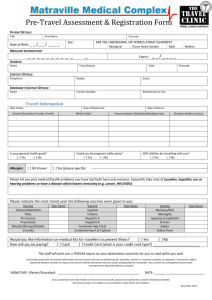
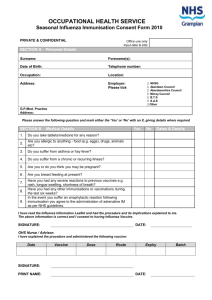
advertisement

DAY CARE INFECTIONS 13 million children under 5 years of age use child care services. National Center for Health Statistics, 2010 90 percent of families with preschool children use child care services. National Commission on Children, 2010 TYPES OF DAY CARE SETTINGS Small family child-care home • 6 children • licensing not required Large family child-care home • 7-12 children • variable licensing requirements Centers • 13 children • Licensed Facilities for ill children Facilities for children with special needs APHA/AAP Out-of-Home Child Care Guidelines, 1992. HIGH RISK PERSONNEL Susceptible to childhood infections (measles, mumps, chickenpox, etc.) Immunocompromised • asplenia • cancer • transplantation • HIV Pregnant women Grossman Ed 8, Infection Control in the Child Care Center, Demos Medical Publisher, 2012 HIGH RISK CHILDREN Risk Factors: Infancy Immunocompromised Chronic lung disease Cardiac disease Physical handicaps Chronic skin disease Grossman, Ed 8, Infection Control in the Child Care Center, Demos Medical Publisher, 2012. HIGH RISK CHILDREN FOR SPREADING INFECTION Children living in impoverished conditions • multiple care givers • transient “family” or shelter • poor sanitary conditions • untreated infections in the home Children from developing nations Children with immune deficiencies Children with chronic infections DAY CARE FACTORS THAT INCREASE TRANSMISSION OF PATHOGENS Large numbers of children in close contact Infants and toddlers have • no independent personal hygiene • are incontinent • put everything in their mouths Children are susceptible to most infectious agents Infected children may be contagious before symptomatic • Parvovirus B19 • Varicella Infected children may be asymptomatic • Giardia • Hepatitis A RESPIRATORY TRANSMISSION Bacteria Bordetella pertussis Haemophilus influenzae type B Mycobacterium tuberculosis Neisseria meningitidis Streptococcus pneumoniae Viruses Adenovirus Influenza Measles Parainfluenza Parvovirus B19 Respiratory syncytial virus Rhinovirus Rubella Varicella FECAL-ORAL TRANSMISSION Bacteria Campylobacter Clostridium difficile E. coli 0157:H7 Salmonella Shigella Viruses Parasites Astrovirus Cryptosporidium Calicivirus Enterobius vermicularis Enteric adenovirus Giardia lamblia Enteroviruses Hepatitis A Rotavirus TRANSMISSION BY SKIN OR MUCOUS MEMBRANE CONTACT Bacteria Viruses Parasites and Fungi Group A streptococci Herpes simplex Pediculosis Staphylococcus aureus Varicella zoster Scabies Molluscum contagiosum Tinea capitis Tinea corporis TRANSMISSION BY INOCULATION OR SPLATTERING OF BLOOD Cytomegalovirus Hepatitis B Hepatitis C Human immunodeficiency virus ILLNESSES AND ABSENTEESIM IN DAY CARE CHILDREN (2 YEAR SURVEILLANCE PERIOD) Illness Episodes Days Absent Age (years) CC Homes CC Centers CC Homes CC Centers 1 1-2 17 16 5 16 15 10 7 11 3-4 9 6 5 9 5 7 4 4 5 Cordell RL, Pediatrics 100:850, 1997. ANTIBIOTIC USE IN DAY CARE CHILDREN (2 MONTH SURVEILLANCE PERIOD) CC Centers CC Homes Home % who received antibiotics 36% 7% 8% Mean duration of antibiotics 21 5 5 Pickering, Infect Dis Child 11:61, 1998. ENVIRONMENTAL COLIFORM CONTAMINATION (2946 SAMPLES) Number Contaminated (%) Inanimate objects 307 (15) Toy balls 73 (46) Hands 131 (17) Van et al, JAMA, 1991. HEPATITIS A HEPATITIS A Child care attendees or employees account for 14% of all cases of Hepatitis A in the United States. ETIOLOGIC AGENT Small non-enveloped RNA virus EPIDEMIOLOGY Source • infected human High risk child care centers • large numbers of children • longer hours • diapered children Mode of spread • fecal-oral CLINICAL MANIFESTATIONS Most children are asymptomatic 80% of adults are symptomatic Rash Fatigue Jaundice Anorexia Dark urine Light stools Vomiting INCUBATION PERIOD 15 to 50 days INFECTIOUS PERIOD Among symptomatic persons, infectivity has waned by the time the individual seeks medical care. DIAGNOSIS Hepatitis A serology THERAPY Supportive PREVENTION Standard precautions Vaccine Immune serum globulin CHILD CARE EXCLUSION Infected children can return 10 days after onset of symptoms During an outbreak, return to day care will be governed by the public health department RECOMMENDATIONS FOR OTHER CHILDREN Hepatitis A vaccine Immune serum globulin, if exposed Children should be taught how to minimize risks of transmission by handwashing RECOMMENDATIONS FOR PERSONNEL Hepatitis A vaccine Significant risks of infection in the day care setting PARENTAL ADVICE Pre-attendance Hepatitis A vaccine VARICELLA BEFORE 1995 INTRODUCTION OF THE VARICELLA VACCINE IN THE UNITED STATES 4 million cases per year 11,000 hospitalizations per year 100 varicella associated deaths Meyer PA et al, J Infect Dis, 2000 AFTER INTRODUCTION OF VARICELLA VACCINE IN THE UNITED STATES 1995-2000 New Cases: California Texas Pennsylvania 71% 84% 79% ETIOLOGIC AGENT DNA virus EPIDEMIOLOGY Source infected human: -respiratory tract -infected lesions Mode of spread airborne direct contact CLINICAL MANIFESTATIONS Pruritic vesicular rash Fever Systemic symptoms INCUBATION PERIOD 10 to 21 days INFECTIOUS PERIOD Until lesions are crusted DIAGNOSIS Clinical Viral culture Serology THERAPY Acyclovir for high risk individuals PREVENTION Vaccine Airborne and Contact precautions VZIG in high risk exposed children Post-exposure vaccination of susceptible children and adults CHILD CARE EXCLUSION Infected children can return when lesions are crusted (approximately 5 to 7 days) RECOMMENDATIONS FOR OTHER CHILDREN VZIG for high risk exposed children Varicella vaccine RECOMMENDATIONS FOR PERSONNEL Varicella vaccine for susceptible adults THEORETIC CONCERNS Increased Varicella in Older Children and Adults who have: Never received the vaccine Have waning immunity Have less booster exposures to VZV later varicella disease herpes zoster INFLUENZA ETIOLOGIC AGENT Enveloped RNA virus EPIDEMIOLOGY Source • infected human Mode of spread • large droplet aerosol • small droplet aerosol • direct and indirect contact with infected secretions INFLUENZAE ATTRIBUTABLE MORBIDITY IN NORMAL CHILDREN LESS THAN 1YEAR OF AGE Increased Hospitalization Increased Outpatient Visits Increased Antibiotic Use Neuzil KM et al, NEJM, 2000 Izurieta HS et al, NEJM, 2000 High risk children Chronic lung disease Congenital heart disease Immunocompromised Sickle cell disease Diabetes Chronic renal failure Metabolic disease Under 2 years of age CLINICAL MANIFESTATIONS Fever Headache Myalgias/Arthralgias Chills Pharyngitis Rhinorrhea Cough/Croup/Bronchitis INCUBATION PERIOD 1 to 3 days INFECTIOUS PERIOD Influenza A - 6 days prior to 7 days after symptoms Influenza B - 6 days prior to 14 days after symptoms DIAGNOSIS Viral Culture Rapid tests (immunofluorescent or enzyme immunoassay) THERAPY Influenza A Influenza B -Amantadine -Rimantadine -Zamamivir (inhaled) -Oseltamivir -Zamamivir (inhaled) -Oseltamivir PREVENTION Annual influenza vaccine • high risk children - recommended* • healthy children 6 to 23 months encouraged* Prophylactic antiviral therapy for high risk children *Recommendations of the ACIP, MMWR, 2002 CHILD CARE EXCLUSION Until child is able to participate in child care center activities RECOMMENDATIONS FOR OTHER CHILDREN Avoid aspirin during influenza season Annual influenza vaccine RECOMMENDATIONS FOR PERSONNEL Annual influenza vaccine MOLLUSCUM CONTAGIOSUM ETIOLOGIC AGENT DNA virus EPIDEMIOLOGY Source • infected human Mode of spread • direct skin to skin contact • contaminated formites CLINICAL MANIFESTATIONS Small painless skin lesions notable for a central dimple Lesions are usually on face, trunk and limbs Lesions spontaneously disappear within 6-12 months INCUBATION PERIOD 2-24 weeks INFECTIOUS PERIOD As long as child has visible lesions DIAGNOSIS Clinical Biopsy THERAPY Usually unnecessary Cryotherapy Curettage Laser Cimetidine Topical therapies Acyclovir for high risk individuals PREVENTION No vaccine available Handwashing Cover lesions with clothing CHILD CARE EXCLUSION None recommended PREVENTIVE STRATEGIES ENTRANCE REQUIREMENTS FOR CHILDREN Medical history Immunizations • Diphtheria-Pertussis-Tetanus • Hemophilus influenza B • Hepatitis A • Hepatitis B • Influenza • Mumps • Polio • Rubella • Rubeola • Varicella • Pneumococcus ENTRANCE REQUIREMENTS FOR STAFF Medical history Immunizations • Diphtheria-Tetanus • Hepatitis A • Hepatitis B • Influenza • Mumps • Polio • Rubella • Rubeola • Varicella • (Pertussis) EXCLUSION FROM CHILD CARE INFECTION Chickenpox Conjunctivitis Bacterial Viral Diarrhea EXCLUSION UNTIL: Lesions are dry and crusted 24 hours after the initiation of therapy Exudate disappears Diarrhea can be contained Infection has been treated (eg. Shigella) Hepatitis (A,B,C) Asymptomatic Herpetic Gingivostomatitis Lesions are dry and crusted Impetigo 48 hours after effective therapy Measles (Rubeola) 5 days from the appearance of the rash Pediculosis/Scabies Infestation has been treated Pertussis 5-7 days after initiation of antibiotics Rotavirus Asymptomatic Salmonella Diarrhea can be contained Streptococcal Infection Upper Respiratory Illness 24 hours after initiation of antibiotics Lack of fever