Complication of Hemodialysis
advertisement

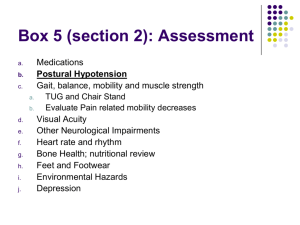
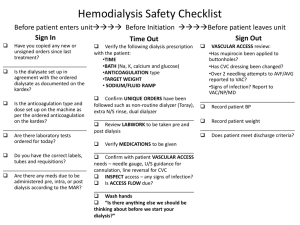
Acute Complication of Hemodialysis Dr.Alaa Mohammed Fouad Mousli Surgical Demonstrator Objective In this presentation we will review briefly the causes, diagnosis and treatment of the common acute complications that we face during hemodyalysis. Acute complication HHCCBNF Hypotension — 25 to 55 % Cramps — 5 to 20 % Nausea and vomiting — 5 to 15 % Headache — 5% Chest pain — 2 to 5 % Back pain — 2 to 5 % Itching — 5 % Fever and chills — Less than 1 % Hypotension Usual manifestation of hemodynamic instability during ultrafiltration dialysis (in which fluid removal is the primary goal) Why is it important? Whatever the underlying cause, patients with hemodialysis-associated hypotension appear to have increased mortality. Clinical Patterns There are TWO clinical patterns of dialysis-associated hypotension: Episodic hypotension, which typically occurs during the latter stages of dialysis; this is associated with vomiting, muscle cramps, and other vagal symptoms (such as yawning). Clinical Patterns – Con’t Chronic persistent hypotension in long-term patients with predialysis systolic blood pressures of less than 100 mmHg. Etiology Rapid reduction in plasma osmolality, which causes extracellular water to move into the cells . Rapid fluid removal in an attempt to attain "dry weight" Inaccurate determination of true "dry weight". Autonomic neuropathy (the role of baroreceptors and a subsequent increase in efferent sympathetic activity). Diminished cardiac reserve. Use of acetate rather than bicarbonate as a dialysate buffer. (Acetate accumulation in the blood has vasodilator activity). Intake of antihypertensive medications that can impair cardiovascular stability. Use of a lower sodium concentration in the dialysate Arrhythmias or pericardial effusion with tamponade, which are volume-unresponsive causes of hypotension. Reactions to the dialyzer membrane, which may cause wheezing and dyspnea as well as hypotension. Increased synthesis of endogenous vasodilators, such as nitric oxide. Sudden release of adenosine during organ ischemia High magnesium concentrations in the dialysate. Failure to increase plasma vasopressin levels. Keep it in Mind Plasma osmolality. True dry wight. Autonomic Neuropathy. Acetate & Nitric Oxide. Na & Mg. Cardiac Diseases. Be patient in your management DIAGNOSIS AND TREATMENT Although occasionally asymptomatic, patients with hypotension may suffer from : ◦ ◦ ◦ ◦ light-headedness. muscle cramps. Nausea & vomiting. dyspnea. The acute management of low blood pressure associated with hemodialysis includes the following: Ultrafiltration should either be stopped or the rate decreased. The patient should be placed in the Trendelenburg position. The blood flow rate should be reduced. Intravascular volume may be replaced with mannitol or saline. Currently the use of an intravenous bolus of saline is the first-line therapy for hypotension. PREVENTION Accurate setting of the "dry weight" Steady, constant ultrafiltration Increased dialysate sodium concentration and sodium modeling Bicarbonate dialysate buffer Temperature control Prevention – Con’t Improvement in cardiovascular performance in cardiac patients. Midodrine (the selective alpha-1 adrenergic agonist) in patients with autonomic neuropathy and perhaps others with severe hemodialysis hypotension not responsive to the above measures. Carnitine . Avoidance of food. Adenosine receptor antagonist. Vasopressin infusion. Muscle Cramps A cramp is a prolonged involuntary muscle contraction common complication of hemodialysis treatments and mostly involves the muscle of the lower extremities in old non diabetic anxious patient resulting in early termination of a hemodialysis session. Usually occur near the end of hemodialysis treatments. Low PTH Values and high serum Creatin phosphokinase is frequent finding Etiology Plasma volume contraction. Tissue hypoxia Hyponatremia. Hypomagnesemia. Carnitine deficiency. Treatment. Treatment is directed at two goals: ◦ Reducing the frequency of cramps. ◦ Relieving symptoms when they occur. Interventions to reduce the frequency of cramps ◦ Prevention of dialysis-associated hypotension. ◦ The use of high concentrations of sodium in the dialysate. ◦ Carnitine supplementation ◦ Administration of quinine that decrease the excitability of the motor end-plate to nerve stimulation and increase muscle refractory period, thereby preventing prolonged involuntary muscle contraction. All these may reduce the frequency of dialysisassociated cramps. Minimize inter-dialytic weight gains ◦ will avoid plasma volume contraction and hypo-osmolality that occurs with high rates of ultrafiltration required to achieve the patient's dry weight during a brief dialysis session. Others These include short acting benzodiazepines (eg, oxazepam), nifidepine, phynetoin, creatine monohydrate, carbamezapine, amitryptalyin, and gabapentin. Headach, Nausea & Vomiting The longer treatment times together with large degree of urea removal and/or ultra filtration significantly enhance the incidence of headache, nausea, and vomiting during dialysis. Longer dialysis time alone doesn’t cause these side effects. These symptoms may be apart of dialysis disequilibrium Syndrome (DDS) will be discussed later. Patients who have headaches on dialysis in the absence of hypotension and suspected dialysis disequilibrium should be questioned about : ◦ Caffien use, which can sometimes precipitate headache ◦ Metabolic disturbances (eg, hypoglycemia, hypernatremia, hyponatremia), ◦ Uremia ◦ Subdural hematoma ◦ Medication-induced headaches. Dialysis disequilibrium Syndrome DDS central nervous system disorder described in dialysis patients characterized by neurological symptoms of varying severity that are thought to be due primarily to cerebral edema. Usually occure in new patient started on hemodialysis especially with hign BUN. Other risk factor , sever metabolic acidosis , extremes of age , presence of other CNS diseases like seizure disorders. Pathogenesis The symptoms of DDS are caused by water movement into the brain, leading to cerebral edema. Two theories have been proposed to explain why this occurs: ◦ a reverse osmotic shift induced by urea removal . ◦ fall in intracellular pH. Clinical Manifestation The classic DDS develops during or immediately after hemodialysis. Early findings include ◦ ◦ ◦ ◦ ◦ ◦ ◦ Headache Nausea Disorientation Restlessness Blurred vision Asterixis More severely affected patients progress to confusion, seizures, coma, and even death. Differential Diagnosis Uremia Subdural hematoma CVA Meningitis Metabolic disturbances Drug induced encephalopathy Treatment In general, symptoms of DDS are self-limited and usually resolve within several hours. The management of mild nonspecific disequilibrium symptoms, such as nausea, vomiting, restlessness, and/or headache, is symptomatic; however, in the acutely uremic patient with such symptoms who is undergoing dialysis, the blood flow rate should be slowed and consideration should be given to stopping the dialysis session. Dialysis is stopped in the patient with seizures, coma, and/or obtundation. Patency of the airway should be ensured. Severe DDS with seizures can be reversed more rapidly by raising the plasma osmolality with either 5 mL of 23 percent saline or 12.5 g of hypertonic mannitol. CHEST PAIN Chest pain that occurs during dialysis could be: associated with hypotension DDS Angina Hemolysis Air or pulmonary embolism (rare). The decision to continue or stop the dialysis treatment because of chest pain is based upon clinical findings, such as hemodynamic stability, and the results of the history and physical examination. Angina should always be considered as those patients at an increased risk of coronary disease. The appropriate history, physical examination, and, if clinically indicated, electrocardiogram and cardiac enzyme evaluation should therefore be performed.If dialysis is continued, the administration of oxygen and aspirin, reduction of the desired ultrafiltration and/or blood pump speed, and administration of nitrates or morphine should be considered on an individual basis. Angina during dialysis may be prevented with the administration of nitrates and/or beta blockers prior to the treatment. However, the efficacy of these agents is diminished since they commonly result in hypotension, thereby reducing the ability to effectively remove extracellular fluid. Hemolysis May present as chest pain and tightness, or back pain and If it is not recognized early, severe hyperkalemia may happen and lead to death. Findings highly suggestive of hemolysis include: A port wine appearance of the blood in the venous line Complaints of chest pain, shortness of breath, and/or back pain A falling hematocrit A pink color of the plasma in centrifuged specimens. The etiology of hemolysis in hemodialysis patients is usually related to problems with the dialysis solution These include: Overheating Hypotonicity due to an insufficient concentrate-to-water ratio Red blood cell trauma like in kinking of the blood lines. Con’t hemolysis The initial treatment is to: stop dialysis immediately Clamp the blood lines (do not return the blood to avoid hyperkalemia) prepare to treat hyperkalemia and the potentially severe anemia investigate the cause hospitalization for observation since life-threatening hyperkalemia may develop after dialysis has been terminated. Air embolism Rare but fatal cause of chest pain and dyspnea during dialysis. (Foam in the venous blood line should rise the suspicion that air is entering the dialysis system). Disconnection of connecting caps and/or blood lines can also lead to air embolism in patients being dialyzed with central venous catheters. Symptoms of the air embolism depend upon the patient's position at the time of the event. In the seated patient, air tends to migrate into the cerebral venous system without entering the heart leading to loss of consciousness and seizure while in those who are recumbent, air tends to enter the heart and then the lungs leading to dyspnea, cough, and perhaps chest tightness. Con’t- Air embolism Treatment of suspected air embolism includes: Clamping the venous line and stopping the blood pump Positioning of the patient on the left side in a supine position with the chest and head tilted downward. Cardiorespiratory support The administration of 100 percent oxygen by either mask or endotracheal tube The most important aspect of air embolism is prevention by the adequate function of monitoring devices on dialysis machines THANK YOU