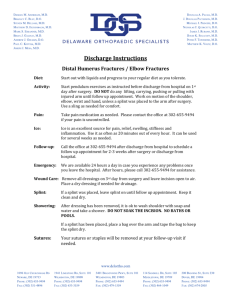
NSC - Splinting
advertisement

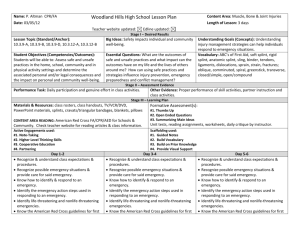
Extremity Injuries and Splinting Dr. Esmailian mehrdad Assistant Professor of Emergency Medicine M_esmailian@med.mui.ac.ir 4-1 Skeletal System 42 Functions of the Musculoskeletal System Gives the body shape Protects internal organs Provides for movement Consists of more than 600 muscles 43 Splinting Movement may worsen musculoskeletal injury and cause more pain Splint injured arm or leg if risk of area being moved (unless help expected quickly) Always splint an extremity before transporting victim 44 Splinting Helps prevent further injury Reduces pain Minimizes bleeding and swelling 45 Mechanism of Injury Force may be applied in several ways: 46 Significant force is generally required to cause fractures or dislocations This force may be applied to the limb in any of the following ways: 1) Direct blows 2) Indirect forces 3) Twisting forces 4) High-energy injury 47 1) A direct blow fractures the bone at the point of impact 2) Indirect force may cause a fracture or dislocation at a distant point 3) Twisting injuries are a common cause of musculoskeletal injury, especially to the knee 48 4) High-energy injuries produce severe damage to the skeleton, surrounding soft tissues, and vital internal organs a. Automobile crashes b. Falls from heights c. Gunshot wounds 49 Trauma is not necessary to fracture a bone a. Slight force can easily injure a weakened bone b. In geriatric patients with osteoporosis, minor falls, simple twisting, or even a muscle contraction may cause a fracture 410 Injuries from Falls Frequently after a fall, the force of the injury is transmitted up the legs to the spine, sometimes resulting in a fracture of the lumbar spine 411 Types of Musculoskeletal Injuries Fracture Broken bone Dislocation Disruption of a joint Sprain Joint injury with tearing of ligaments Strain Stretching or tearing of a muscle 412 Splinting Splints can be improvised when needed and tied with bandages, belts, neckties, strips of cloth Always check breathing and care for lifethreatening conditions first Consider mechanism of injury and possibility of spinal injury 413 Fractures • Closed fracture A fracture that does not break the skin • Open fracture External wound associated with fracture • Nondisplaced fracture Simple crack of the bone • Displaced fracture • Fracture in which there is actual deformity 414 Signs and Symptoms of a Fracture Deformity Tenderness Guarding Swelling Bruising 415 Crepitus False motion Exposed fragments Pain Locked joint 416 Signs and Symptoms of a Dislocation Marked deformity Swelling Pain Tenderness on palpation Virtually complete loss of joint function Numbness or impaired circulation to the limb and digit 417 Signs and Symptoms of a Sprain Point tenderness can be elicited over injured ligaments. Swelling and ecchymosis appear at the point of injury to the ligaments. Pain Instability of the joint is indicated by increased motion. 418 Severity of Injury Critical injuries can be identified musculoskeletal injury grading system 419 using Minor Injuries Minor sprains Fractures or dislocations of digits 420 Moderate Injuries Open fractures of the digits Nondisplaced long bone fractures Nondisplaced pelvic fractures Major sprains of a major joint 421 Serious Injuries Displaced long bone fractures Multiple hand and foot fractures Open long bone fractures Displaced pelvic fractures Dislocations of major joints Multiple digit amputations Laceration of major nerves or blood vessels 422 Severe Life-Threatening Injuries (Survival Is Probable) Multiple closed fractures Limb amputations Fractures of both long bones on the leg (bilateral femur fractures) 423 Critical Injuries (Survival Is Uncertain) Multiple open fracture of the limbs Suspected pelvic fractures with hemodynamic instability 424 Rapid Physical Exam for Significant Trauma If you find no external signs of injury, ask patient to move each limb carefully, stopping immediately if this causes pain Skip this step if the patient reports neck or back pain. Slight movement could cause permanent damage to spinal cord 425 Focused Physical Exam for Nonsignificant Trauma Evaluate circulation, motor function, sensation If two or more extremities are injured, transport Severe injuries more likely if two or more bones have been broken Recheck neurovascular function before and after splinting Impaired circulation can lead to death of the limb 426 Assessing Neurovascular Status If anything causes pain, do not continue that portion of exam Pulse Palpate the radial, posterior tibial, and dorsalis pedis pulses 427 Capillary refill Note and record skin color Press the tip of the fingernail to make the skin blanch. If normal color does not return within 2 seconds, you can assume that circulation is impaired 428 Sensation Check feeling on the flesh near the tip of the index finger In the foot, check the feeling on the flesh of the big toe and on the lateral side of the foot 429 Motor function Evaluate muscular activity when the injury is near the patient’s hand or foot Ask the patient to open and close his or her fist Ask the patient to wiggle his or her toes 430 Emergency Medical Care Completely cover open wounds Apply the appropriate splint If swelling is present, apply ice or cold packs Prepare the patient for transport Always inform hospital personnel about wounds that have been dressed and splinted 431 Splinting Flexible or rigid device used to protect extremity Injuries should be splinted prior to moving patient, unless the patient is critical Splinting helps prevent further injury Improvise splinting materials when needed 432 General Principles of Splinting Remove clothing from the area Note and record the patient’s neurovascular status Cover all wounds with a dry, sterile dressing Do not secure splint on open wound Do not move the patient before splinting Splint only if it doesn’t cause more pain 433 Immobilize the joints above and below the injured joint Pad all rigid splints Elevate splinted extremity if possible Apply cold packs if swelling is present Maintain manual immobilization 434 Use constant, gentle, manual traction if needed If you find resistance to limb alignment, splint the limb as is Check circulation Swelling, bluish color, tingling, numbness, cold skin are signs and symptoms of reduced circulation If reduced circulation, remove splint 435 Immobilize all suspected spinal injuries in a neutral in-line position If the patient has signs of shock, align limb in normal anatomic position and transport When in doubt, splint 436 Types of Splints Rigid splints Soft splints Anatomic splints 437 Rigid Splint Board Plastic or metal Rolled newspaper or magazine Thick cardboard 438 439 440 Applying a Rigid Splint Provide gentle support and in-traction of the limb Another EMT-B places the rigid splint alongside or under the limb Place padding between the limb and splint as needed 441 Secure the splint to the limb with bindings Assess and record distal neurovascular function 442 Soft Splint Pillow Folded blanket or towel Triangular bandage folded into sling 443 Anatomic Splint Bandage injured leg or finger to uninjured one 444 In-line Traction Splinting Act of exerting a pulling force on a bony structure in the direction of its normal alignment Realigns fracture of the shaft of a long bone Use the least amount of force necessary If resistance is met or pain increases, splint in deformed position 445 Securing Splints Use bandages, strips of cloth (cravats), Velcro® straps around splint and extremity Use knots that can be untied Do not secure with tape 446 Hazards of Improper Splinting Compression of nerves, tissues, and blood vessels Delay in transport of a patient with a lifethreatening condition Reduction of distal circulation Aggravation of the injury Injury to tissue, nerves, blood vessels, or muscle 447 Upper Extremity Injuries Clavicle and Scapula Shoulder Upper arm Elbow Lower arm Wrist Hand 448 Clavicle and Scapula Injuries Clavicle is one of the most fractured bones in the body Scapula is well protected Joint between clavicle and scapula is the acromioclavicular (A/C) joint Splint with a sling and swathe 449 Pad hollow between body and arm Apply sling and binder to support arm and immobilize against chest if this causes pain use larger soft splint 450 A/C Separation With A/C separation, the distal end of the clavicle usually sticks out 451 Dislocation of the Shoulder Most commonly dislocated large joint Usually dislocates anteriorly Is difficult to immobilize A patient with a dislocated shoulder will guard the shoulder, trying to protect it by holding the arm in a fixed position away from the chest wall 452 Splint the joint with a pillow or towel between the arm and the chest wall Apply a sling and a swathe 453 Guidelines for Slings Use sling to prevent movement of arm and shoulder and to elevate extremity Splint injury first, when appropriate If you splint injury in position found and this position makes use of sling difficult – do not use sling 454 Guidelines for Slings Do not move arm into position for sling if it causes pain A cold pack can be used inside sling Do not cover fingers inside sling 455 Fractures of the Humerus Occurs either proximally, in the midshaft, or distally at the elbow Consider applying traction to realign a severely angulated humerus, according to local protocols Splint with sling and swathe, supplemented with a padded board splint 456 Apply rigid splint along outside of arm Tie above injury and at elbow Support wrist with sling Apply wide binder to support arm and immobilize it against chest If it causes pain to raise wrist for sling, use a long rigid splint 457 Elbow Injuries Fractures and dislocations often occur around the elbow Injuries to nerves and blood vessels common Assess neurovascular function carefully Realignment may be needed to improve circulation 458 If elbow bent, apply rigid splint from upper arm to wrist If more support needed, use sling at wrist and binder around chest 459 Elbow Injuries If elbow straight, apply rigid splint from upper arm to hand If more support needed, use binders around chest and upper arm and lower arm and waist 460 Fractures of the Forearm Usually involves both radius and ulna Use a padded board, air, vacuum, or pillow splint A fracture of the distal radius produces a characteristic silver fork deformity 461 Secure point of bandage at elbow 462 Position triangular bandage 463 Bring lower end of bandage to opposite side of neck 464 Tie the ends 465 Tie binder bandage over sling and around chest 466 Injuries to the Wrist and Hand Follow BSI precautions Cover all wounds Form hand into the position of function Place a roller bandage in palm of hand Apply padded board splint Secure entire length of splint Apply a sling and swathe 467 Apply rigid splint on palm side of arm from forearm past fingertips Tie above and below wrist Leave fingers uncovered Support forearm and wrist with sling and apply binder around upper arm and chest 468 Support arm. Check circulation 469 Position arm on rigid splint 470 Secure splint 471 Check circulation 472 Put arm in sling. Tie binder over sling and around chest 473 Finger Injuries Fractures and dislocations Often splint not required Use rigid splint or anatomic splint 474 Lower Extremity Injuries Pelvic and Hip Upper leg Knee Lower leg Ankle Foot 475 Fractures of the Pelvis/Hip May involve life-threatening internal bleeding Assess pelvis for tenderness Stable patients can be secured to a long backboard or scoop stretcher to immobilize isolated fractures of the pelvis 476 Assessment of Pelvic/Hip Fractures If there is injury to the bladder or urethra, the patient may have lower abdominal tenderness They may have blood in the urine (hematuria) or at the urethral opening 477 Stabilizing Pelvic/Hip Fractures A stable patient with a pelvic fracture may be placed on a long board If the patient is unstable, consider using a PAGS with the patient stabilized on the long board (consult your local protocols) 478 Do not move victim Immobilize leg and hip in position found Pad between legs and bandage together (unless this causes more pain) Treat victim for shock but do not elevate legs 479 Dislocation of the Hip Hip dislocation requires significant mechanism of injury Posterior dislocations lie with hip joint flexed and thigh rotated inward Anterior dislocations lie with leg extended straight out, and rotated, pointing away from midline Splint in position of deformity and transport 480 Femoral Fractures Presents with very characteristic deformity Fractures from trauma injuries best managed with traction splint or PASG and a backboard Isolated fracture in geriatric patients can be managed with long backboard or a scoop stretcher 481 A proximal femur fracture will be rotated Splint the injured leg to the uninjured leg and secure the patient to a scoop stretcher or backboard 482 Rigid splint may be unnecessary Provide additional support with folded blankets or coats Can use an anatomic splint Check circulation and sensation in foot and toes 483 Put rigid splint on each side of leg Pad body areas and voids Inside splint should extend from groin past foot Outside splint should extend from armpit past foot 484 Splinting a Femur Fracture Tie splints with cravats or bandages Check circulation periodically 485 Injuries of Knee Ligaments Knee is very vulnerable to injury Patient will complain of pain in the joint and be unable to use the extremity normally Splint from hip joint to foot Monitor distal neurovascular function 486 Dislocation of the Knee Produces significant deformity More urgent injury is to the popliteal artery, which is often lacerated or compressed Always check distal circulation 487 Fractures About the Knee If there is adequate distal pulse and no significant deformity, splint limb with knee straight If there is adequate distal pulse and significant deformity, splint joint in position of deformity If pulse is absent below level of injury, contact medical control immediately 488 Dislocation of the Patella Usually dislocates to lateral side Produces significant deformity Splint in position found Support with pillows 489 If possible, put rigid splint on both sides of leg Pad body areas and voids Check circulation and sensation in foot and toes first and periodically after splinting 490 Splinting the Knee If knee is straight apply two splints along both sides of knee If knee is bent, splint in position found Tie splints with cravats or bandages 491 Injuries to Lower Leg Usually, both bones fracture at the same time. Open fracture of tibia common Stabilize with a padded rigid long leg splint or an air splint that extends from the foot to upper thigh Because the tibia is so close to the skin, open fractures are quite common 492 Rigid splint applied the same as for knee injury Three-sided cardboard splint can be used 493 Check circulation. Gently slide four to five strips of bandages under both legs 494 Pad between legs 495 Gently slide uninjured leg next to injured leg 496 Tie bandages. Check circulation 497 Ankle Injuries Most commonly injured joint Dress all open wounds Assess distal neurovascular function Correct any gross deformity by applying gentle longitudinal traction to the heel Before releasing traction, apply a splint 498 Ankle Injuries Position foot in middle of soft pillow Fold pillow around ankle Tie pillow around foot and lower leg 499 Foot Injuries Usually occur after a patient falls or jumps. Immobilize ankle joint and foot Leave toes exposed to assess neurovascular function 4100 Elevate foot Also consider possibility of spinal injury from a fall A pillow splint can provide excellent stabilization of the foot 4101 4102