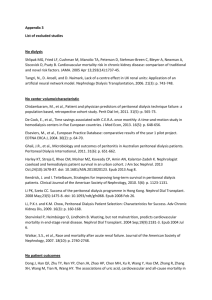
Prezentacja programu PowerPoint

NADCIŚNIENIE I NIEDOCIŚNIENIE TĘTNICZE U
CHORYCH DIALIZOWANYCH
– DIAGNOSTYKA I LECZENIE
R Y S Z A R D G E L L E R T
K L I N I K A N E F R O L O G I I I C H O R Ó B W E W N Ę T R Z N Y C H , C M K P
TOP
NEPHROLOGICAL
TRENDS
Poznań, 10-11.10.2014
Conflict of interest
NONE
• HYPERTENSION
• Chronic
• HYPOTENSION
• Chronic
• Intradialytic
• BP intradialytic increase
BP IN CKD 5D
HYPERTENSION IN CKD 5D: PREVALENCE
• The prevalence of hypertension was 86% (among 369 chronic HD patients, defined by either a 44-hour interdialytic ambulatory BP of ≥135/85 mmHg or the prescription of any antihypertensive agent).
• Antihypertensive drugs prescribed in 89% of patients, but adequate controll only in 38%.
• Inferior vena cava (IVC) diameter in expiration was associated with increased risk of poorly controlled hypertension both in cross-sectional analysis and after withdrawal of antihypertensive drug
• Poor control was independently associated with greater antihypertensive drug use.
Agarwal R: Epidemiology of interdialytic ambulatory hypertension and the role of volume excess. Am J Nephrol 34: 381–390, 2011
ADJUSTED FIVE-YEAR SURVIVAL PROBABILITIES AMONG INCIDENT
ESRD PATIENTS, 2006 (FROM DAY ONE; TABLE 5.B)
• diabetes: 0.34;
• HYPERTENSION: 0.40;
• glomerulonephritis: 0.51;
• other: 0.38
USRDS, 2013
ARTERIAL PRESSURE
Coordination
Pump
VOLUME
Resistance
Arterial compliance (C=dV/dP)
KDIGO CLINICAL PRACTICE GUIDELINE
FOR THE MANAGEMENT OF BLOOD PRESSURE IN
CHRONIC KIDNEY DISEASE (KI, DEC., 2012)
• 343 Chapter 1: Introduction
• 347 Chapter 2: Lifestyle and pharmacological treatments for lowering blood pressure in CKD ND patients
• 357 Chapter 3: Blood pressure management in CKD ND patients without diabetes mellitus
• 363 Chapter 4: Blood pressure management in CKD ND patients with diabetes mellitus
• 370 Chapter 5: Blood pressure management in kidney transplant recipients (CKD
T )
• 372 Chapter 6: Blood pressure management in children with CKD ND
• 377 Chapter 7: Blood pressure management in elderly persons with CKD ND
• 382 Chapter 8: Future directions and controversies
SUMMARY OF KDIGO GUIDELINE. WHAT DO WE REALLY KNOW ABOUT MANAGEMENT
OF BLOOD PRESSURE IN PATIENTS WITH CHRONIC KIDNEY DISEASE?
DAVID C. WHEELER, GAVIN J. BECKER; KI 2013
Before the development of the BP Guideline, KDIGO organized a consensus conference on the topic of BP management in CKD 5 patients receiving dialysis, held in New York in March 2009. The conference report concluded that there was uncertainty about how to measure BP in hemodialysis patients, a poor understanding of the association between BP and risk of adverse outcomes, and a complex interplay of factors influencing both systolic and diastolic pressure. As a result, the KDIGO executive decided that it was premature to make recommendations regarding BP management in CKD Stage 5D patients .
BLOOD PRESSURE TREATMENT -
“CONVENTIONAL“ WISDOM IN ESRD PATIENTS
Salt ???
Changes over time ??? Heart failure
Volume - dependent
Salt/water
Blood pressure regulation
Vasoconstriction - dependent
RAS, sympathetic activity, lack of
NO, medullipin etc.
Arterial compliance calcification
What is the “real” RR ???
HD HD HD
Acute changes ???
HD HD
HD
HOME BLOOD PRESSURE MONITORING IS OF GREATER
PROGNOSTIC VALUE THAN HEMODIALYSIS UNITS RECORDINGS
Alborzi et al. CJASN 2007;2:1228-1234
HYPERTENSION IN CKD 5D – DIAGNOSTIC APPROACH
• THERE HAVE BEEN NO RANDOMIZED PROSPECTIVE TRIALS EVALUATING THE
TARGET BLOOD PRESSURE IN DIALYSIS PATIENTS
• Recommend (???):
<140/90 mm Hg preHD, <130/80 postHD, (BP higher by 10 mmHg as comapred to interdialytic readings)
<135/85 mmHg daytime, <120/80 mmHg nighttime (self- monitoring, ambulatory automated BP monitoring)
• Volemia/hydration status – clinical evaluation + bioimpedance (multifrequency)
• Ca-P, PTH
• Std Kt/V (weekly)
• Patient’s compliance
• Other (if secondary hypertension suspected, RAA, )
BLOOD PRESSURE AND LONG-TERM MORTALITY IN UNITED STATES
HEMODIALYSIS PATIENTS: USRDS WAVES 3 AND 4 STUDY
ROBERT N FOLEY, ET AL.: KIDNEY INTERNATIONAL (2002) 62, 1784–1790
BLOOD PRESSURE AND LONG-TERM MORTALITY IN UNITED STATES
HEMODIALYSIS PATIENTS: USRDS WAVES 3 AND 4 STUDY
ROBERT N FOLEY, ET AL.: KIDNEY INTERNATIONAL (2002) 62, 1784–1790
BLOOD PRESSURE AND LONG-TERM MORTALITY IN UNITED STATES
HEMODIALYSIS PATIENTS: USRDS WAVES 3 AND 4 STUDY
ROBERT N FOLEY, ET AL.: KIDNEY INTERNATIONAL (2002) 62, 1784–1790
Association between BP and 15-month CV death in 40 933 maintenance HD patients
(95% confidence interval bars are depicted)
The lowest mortality was associated with predialysis systolic pressure of 160 to 189 mm Hg
Kalantar-Zadeh et al. Hypertension 2005;45:811-817
Unadjusted, case-mix and dialysis dose–adjusted
Unadjusted survival by baseline predialysis systolic BP
16,959 incident HD p-ts
Stidley et al. J Am Soc Nephrol 2006;17:513-520
Hazard ratios (HR) for all-cause (AC) mortality by baseline predialysis SBP
Stidley et al. J Am Soc Nephrol 2006;17:513-520
Hazard ratios (HR) for all-cause (AC) mortality by baseline predialysis DBP
Stidley et al. J Am Soc Nephrol 2006;17:513-520
Hazard ratios (HR) for all-cause (AC) mortality by baseline postdialysis SBP
Stidley et al. J Am Soc Nephrol 2006;17:513-520
Hazard ratios (HR) for all-cause (AC) mortality by baseline pulse pressure
Stidley et al. J Am Soc Nephrol 2006;17:513-520
RELATIONSHIP BETWEEN BLOOD PRESSURE AND MORTALITY IN
DIALYSIS PATIENTS.
Luther JM Kidn Int 2008;73:667-668
HYPERTENSION + STRICT VOLUME CONTROL
AND MORTALITY
Relationship between final systolic blood pressure (SBP) and mortality in number per 100 patient-years
Mehmet Ozkahya , Pharmacological and non-pharmacological treatment of hypertension in dialysis patients, Kidney Int Suppl; Dec 2013; 3(4): 380–382.
HYPERTENSION IN CKD 5D - PATHOPHYSIOLOGY
• Hypervolemia - coupled with excessive dietary sodium ( weight increases by 100–
120ml for each gram of NaCl consumed between dialysis sessions ) and fluid intake.
• Renin angiotensin (aldosterone) system overactivity - due to regional renal ischemia and scarring
• Uremia - causes a neural reflex which stimulates cardiovascular centers in brainstem
• Increased sympathetic activity - due to increased levels of Ang II increases vascular resistance
• Erythropoietin – increases BP by 10 mm Hg
• Hyperparathyroidism – Calcification and stiffness of arterial tree
• Increased pulse pressure - due to increase in vascular resistance and volume overload.
• Secretion of ouabain like inhibitors of Na-K ATPases - leads to elevation of intracellular calcium and increases the vascular resistance.
• ADMA (asymmetric dimethyl arginine) - not properly understood.
• Endothelin-1 - potent vasoconstrictor; accumulates second to the decreased renal clearance
• NO (inadeqately low)
SUBGROUP ANALYSES FOR THE EFFECTS OF TREATMENT
ON CARDIOVASCULAR EVENTS treatment with bp lowering agents should routinely be considered for patients undergoing dialysis to prevent cardiovascular events and mortality
Lancet
Published Online February 26, 2009
RISK OF ALL-CAUSE AND CARDIOVASCULAR MORTALITY FOR BLOOD
PRESSURE LOWERING TREATMENT VS CONTROL REGIMENS
Lancet
Published Online February 26, 2009
HYPERTENSION IN HD5D - MANAGEMENT
centered on:
• volume / hydration status control - interdialytic weight gains should be discouraged (low sodium intake + increased dialysis treatments)
• Lifestyle modification – less salt (consumption of 9 g of salt mandatory intake of 1L of water) and alcohol consupmtion, more physical exercise
• Dialysis – longer, more frequent, more ultrafiltration in „resistant” hypertension
• Management of comorbidities
• Antihypertensive agents (ACEi, BB, CCB, minoxidil)
• OTHER – reanal artery denervation (?)
THE EFFECT OF DRY WEIGHT REDUCTION ON INTERDIALYTIC
AMBULATORY SYSTOLIC AND DIASTOLIC BP IN HYPERTENSIVE
HEMODIALYSIS PTS.
among hypertensive patients on hemodialysis the additional ultrafiltration group (n=100) had the dry weight probed without increasing time or duration of dialysis, whereas the control group (n=50) only had physician visits
Agarwal et al. Hypertension 2009; 53: 500-507
CAPTOPRIL TEST FOR HYPERVOLEMIA
• The importance of the captopril test to detect hypervolemia in hypertensive dialysis patients must be mentioned.
• If blood pressure remains >140/90mmHg, but if there is doubt whether euvolemia was reached because CTI is close to normal (<0.50), the captopril test can be used to evaluate the ‘renin-dependency' of the blood pressure.
• The test is performed on a non-dialysis day. Blood pressure is taken at 10-min intervals with an automatic machine in a quiet room for 1h before and at least
90min after oral administration a tablet of 25mg captopril.
• The test is considered positive when blood pressure drops to normal levels or if diastolic blood pressure drops by >10mmHg. If the test is positive, then a renin– angiotensin system blocker such as enalapril should be started. However, if the test is negative, measures to reduce the dry weight must to be performed
PHARMACOLOGIC PROPERTIES OF Β-BLOCKERS IN CHRONIC
DIALYSIS PATIENTS
Acebutolol
Atenolol
Carvedilol
Metoprolol
Propranolol
T1/2(h) normal
3.5
6-9
T1/2(h
)
ESRD
3.5
<120
4-7
3-4
4-7
3-4
Initial dose in HD
Maintenance dose in HD
Removal during HD
200 q24h
25 q48h
5 q24h
50 b.i.d.
200-300 q24h
25-50 q48h
5 q24h
50-100 b.i.d.
yes
Yes no high
2-4 2-4 40 b.i.d.
40-80 b.i.d.
yes
Henrich W. Principles and Practice of Dialysis; za Haller H.
Treatment of Hypertension in Patients on Hemodialysis
PHARMACOKINETIC PROPERTIES OF ACE INHIBITORS IN ESRD
Captopril
Enalapril
Fosinopril
Lisinopril
T1/2(h) normal
2-3
11
12
13
Ramipril 11
T1/2(h)
ESRD
20-30
Initial dose in
HD
Maintenanc e dose in
HD
12.5 q24h 25-50 q24h prolonged 2.5 q24h or q48h
2.5-10 q24h or q48h prolonged 10 q24h 10-20 q24h
54 2.5 q24h or q48h
2.5-10 q24h or q48h prolonged 2.5-5q24h 2.5-10 q24h
Removal during HD
Yes
Yes
Yes
Yes yes
Henrich W. Principles and Practice of Dialysis; za Haller H.
Treatment of Hypertension in Patients on Hemodialysis
PHARMACOKINETIC PROPERTIES OF ARB’S IN ESRD
Candesartan
Irbesartan
Losartan
Telmisartan
Valsartan
T1/2(h) normal
9
T1/2(h
)
ESRD
?
Initial dose in HD
4 q24h
Maintenance dose in HD
8-32 q24h
11-15 11-15 75-150 q24h 150-300 q24h
2
24
4
?
50 q24h
40 q24h
50-100 q24h
20-80 q24h
Removal during HD
No
No
No
No
6 ?
80 q24h 80-160 q24h No
Henrich W. Principles and Practice of Dialysis; za Haller H.
Treatment of Hypertension in Patients on Hemodialysis
TREATMENT OF RESISTANT HYPERTENSION CAN BE NEARLY HALVED
WITH THE AID OF MORE THOROUGH DIAGNOSTIC EVALUATION
Weber F., Anlauf M: Dtsch Arztebl Int. 2014 Jun
20;111(25):425-31
INTRADIALYTIC HYPOTENSION (IDH)
IDH - a serious complication of hemodialysis (HD), associated with increased risk of:
• vascular access thrombosis,
• inadequate dialysis dose ( the fluid administration and early HD termination can leave patients volume-expanded and at risk for associated cardiovascular morbidity)
• mortality
IDH prevalence range from 15% to 50% of ambulatory HD session, depending on the criteria used to define it there is no consensus definition of IDH .
The KDOQI guidelines define IDH as a decrease in either systolic BP ( SBP )≥20 mmHg or mean arterial pressure≥10 mmHg as well as associated symptoms
KDIGO CLINICAL PRACTICE GUIDELINE FOR ACUTE KIDNEY
INJURY (KI, MAR., 2012)
IDH - PATHOPHYSIOLOGY
IDH results from hypovolemia (aggressive reduction of circulating blood volume exceeding plasma refilling) during ultrafiltration and:
• inadequate cardiovascular compensatory mechanisms
• impaired autonomic response to hypovolemia
• vasoactive substances (adenosine, nitric oxide, etc. ) synthesized or release during dialysis
• adrenal insufficiency
• inadeqaute mass transfer of sodium and calcium
• osmolality drop
• antihypertensive drugs’ elimination
• hyperthermia
• acetate in dialysis/substitution fluid
KDIGO CLINICAL PRACTICE GUIDELINE FOR ACUTE KIDNEY
INJURY (KI, MAR., 2012)
• AVOID HYPOTENSION
• TO PREVENT AKI and
• TO PREVENT AKI COMPLICATIONS
• TREAT HYPOTENSION WITH FLUID AND VASOPRESSORS AS INDICATED IN „Early
Goal-Directed Therapy”
KDIGO CLINICAL PRACTICE GUIDELINE FOR ACUTE KIDNEY
INJURY (KI, MAR., 2012)
• 3.9.2: We suggest not using NAC (N-acetylcysteine) to prevent AKI in critically ill patients with hypotension. (2D )
• Available therapies to manage hypotension include fluids, vasopressors and protocols which integrate these therapies with hemodynamic goals. A resuscitation strategy devised for patients with hypotension from septic shock that is based upon achieving specific physiologic end-points within 6 hours of hospital admission has been termed Early Goal-Directed Therapy (EGDT) . This approach has been endorsed by the ‘‘Surviving Sepsis Campaign’’ and has gained considerable acceptance despite only one, single-center, RCT evaluating its effectiveness. This protocolized strategy, consisting of fluids, vasoactive medication, and blood transfusions targeting physiological parameters, is recommended by many experts for the prevention of organ injury in septic-shock patients.
• Bradykinin release syndrome (has been observed at the start of CRRT with uncoated AN-69 membranes.) is characterized by acute hypotension and pulmonary vascular congestion.
KDIGO CLINICAL PRACTICE GUIDELINE FOR ACUTE KIDNEY
INJURY (KI, MAR., 2012)
• Intradialytic hypotension is a major problem during RRT in AKI patients, limiting its efficacy and causing morbidity. Surprisingly, there are only a few studies assessing this highly relevant clinical problem.
In CVVH (Barenbrock et al. ) the incidence of hypotension and other cardiovascular events was lower with bicarbonate
• 5.7.1: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI. (2C )
• 5.7.2: We recommend using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and circulatory shock.
(1B )
• 5.7.3: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and liver failure and/or lactic acidemia. (2B )
KDIGO CLINICAL PRACTICE GUIDELINE
FOR THE MANAGEMENT OF BLOOD PRESSURE IN
CHRONIC KIDNEY DISEASE (KI, DEC., 2012)
GENERAL STRATEGIES
• 2.1: Individualize BP targets and agents according to age, co-existent cardiovascular disease and other co-morbidities, risk of progression of CKD, presence or absence of retinopathy (in CKD patients with diabetes) and tolerance of treatment. (Not Graded)
• 2.2: Inquire about postural dizziness and check for postural hypotension regularly when treating CKD patients with BP-lowering drugs. (Not Graded)
In the HEMO cohort, patients with more frequent episodes of IDH had incrementally greater mortality in both unadjusted and adjusted analyses.
Flythe J E et al. JASN doi:10.1681/ASN.2014020222
©2014 by American Society of Nephrology
Frequency of IDH was similar across HEMO and LDO cohorts.
Flythe J E et al. JASN doi:10.1681/ASN.2014020222
©2014 by American Society of Nephrology
Flythe J E et al. JASN doi:10.1681/ASN.2014020222
ASSOCIATION OF INTRADIALYTIC HYPOTENSION AND CONVECTIVE VOLUME
IN HEMODIAFILTRATION: RESULTS FROM A RETROSPECTIVE COHORT STUDY
FRANKLIN G MORA-BRAVO, ET AL; BMC NEPHROL. 2012; 13: 106.
HDF,
CKD
Group 1: 0 to 0.2 liters. Group 2: 0.3 to 7.53 liters, Group 3: 7.54 to 14.8 liters;
Group 4: 14.9 to 16.96 liters; Group 5: 16.97 to 18.9 liters; Group 6: 19.1 to 21 liters
ACETATE-FREE BIOFILTRATION REDUCES INTRADIALYTIC HYPOTENSION:
A EUROPEAN MULTICENTER RANDOMIZED CONTROLLED TRIAL
TESSITORE N., ET AL.: BLOOD PURIF 2012;34:354–363
BD – bicarbonate dialysis
AFB – acetate free biofiltration
PRESERVATION OF BLOOD PRESSURE STABILITY WITH HYPERTONIC
MANNITOL DURING HEMODIALYSIS INITIATION
FINNIAN R. MC CAUSLAND ET AL.: AM J NEPHROL. 2012 ; 36(2): 168–174
The association of mannitol (gray bar) versus no mannitol administration (reference; white bar) with a drop of >20mmHg from pre-dialysis systolic blood pressure (SBP) or minimum intra-dialytic SBP <90mmHg. Estimates from Model 1 were adjusted for age, sex, diabetes, access
(catheter vs non-catheter), pre-dialysis SBP and congestive heart failure. Model 2 was additionally adjusted for pre-dialysis serum sodium, predialysis weight, acuity of kidney injury (chronic vs acute) and categories of ultrafiltration (0, 0-1, 1-2 and >2 liters), session length (≤120, 121-
180, >180 mins), blood flow (<300, 300-399, 400 mL/min) and dialysate flow (≤500, 501-600, 601-800 mL/min).
VASOPRESSIN RELEASE IS ENHANCED BY THE HEMOCONTROL
BIOFEEDBACK SYSTEM AND COULD CONTRIBUTE TO BETTER
HAEMODYNAMIC STABILITY DURING HAEMODIALYSIS
ESMÉE M. ETTEMA, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2012) 27 (8): 3263-3270.
Table 3.
Plasma AVP levels during SHD (standard Hd) and HHD (Hemocontrol)
[median and interquartile range (IQR)]
AVP level (pg/mL) SHD AVP level (pg/mL) HHD P-value for difference between SHD & HHD
0 Min 0.94 (IQR 0.62–2.10)
30 Min 1.20 (IQR 0.65–1.50)
60 Min 0.92 (IQR 0.47–1.50)
120 Min 0.85 (IQR 0.33–2.30)
180 Min 1.00 (IQR 0.59–3.00)
240 Min 1.20 (IQR 0.8–1.70)
1.00 (IQR 0.84–1.60)
1.90
a (IQR 1.2–2.90)
1.30 (IQR 0.85–2.20)
1.30 (IQR 0.90–2.00)
1.20 (IQR 0.65–3.2)
1.10 (IQR 0.65–3.2)
0.900
0.001
0.041
0.776
0.532
0.394
a Denotes P < 0.01 compared with pre-dialysis value
ADRENOCORTICAL FUNCTION IN HYPOTENSIVE PATIENTS
WITH END STAGE RENAL DISEASE
ALEJANDRO L. ARREGGER ETA AL.: STEROIDS, 84, 2014
Adrenal function normal primary adrenal insufficiency secondary adrenal insufficiency selective hypoaldosteronism secondary hyperaldosteronism
%
30
8
12
18
32
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 3.1.2a Individualized, automatic BV control should be considered as a second-line option in patients with refractory IDH
(Evidence level II).
Guideline 3.1.2b Manual adjustment of ultrafiltration according to a fixed protocol based on changes in blood volume should not be performed (Evidence level II).
Guideline 3.2.1 Although sodium profiling with supraphysiological dialysate sodium concentrations and high sodium dialysate (≥144 mmol/l) are effective in reducing IDH, they should not be used routinely because of an enhanced risk of thirst, hypertension and increased inter-dialytic weight gain
(Evidence level II)
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 3.2.3 The use of a dialysate calcium concentration of
1.50 mmol/l should be considered in patients with frequent episodes of IDH, unless contra-indications are present (Evidence level II).
Guideline 3.2.4a In patients with frequent episodes of IDH, low
(0.25 mmol/l) magnesium dialysate should be avoided, especially in combination with low-calcium dialysate (Level II).
Guideline 3.2.4b Glucose-free dialysate concentrations should be avoided in diabetics (Opinion).
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 3.4.1 Cool dialysate temperature dialysis (35–36
°
C) or isothermic treatments by blood temperature controlled feedback should be prescribed in patients with frequent episodes of IDH
(Evidence level I).
Guideline 3.4.2 With cool temperature dialysis, dialysate temperature should be gradually reduced in steps of 0.5
°
C from
36.5
°
C until symptoms are controlled (Opinion).
Guideline 3.4.3 Dialysate temperatures <35
°
C should not be used
(Opinion).
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 3.6 A prolongation in dialysis time or an increase in dialysis frequency should be considered in patients with frequent episodes of IDH (Levels II–III).
Guideline 3.7 A treatment change to peritoneal dialysis should be considered in patients who remain refractory to interventions for the prevention of IDH (Opinion).
Guideline 4.1 In patients with frequent episodes of IDH, antihypertensive agents should be given with caution prior to dialysis depending on pharmacodynamics, but should not be routinely withheld on the day of haemodialysis treatment
(Evidence level III).
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 4.3 L-carnitine supplementation should be considered for the prevention of IDH if other treatment options have failed
(Evidence level III).
Guideline 6.1 The Trendelenburg position should be considered in the treatment of IDH. However, efficacy may be limited
(Opinion).
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 4.2 Midodrine should be considered if other treatment options have failed (Evidence level I).
Guideline 6.2 Ultrafiltration should be stopped during an episode of IDH (evidence level III).
Guideline 6.3.1 Isotonic saline should be infused in patients unresponsive to stopping ultrafiltration and Trendelenburg's position during an episode of IDH (Evidence level II).
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
Guideline 6.3.2 Infusion of colloid solutions should be considered in patients who remain unresponsive to saline infusion (Evidence level III).
Guideline 6.4 The development a centre-specific protocol, with stepwise interventions for the treatment of IHD should be considered (Evidence level III).
EBPG GUIDELINE ON HAEMODYNAMIC INSTABILITY
JEROEN KOOMAN, ET AL.: NEPHROL. DIAL. TRANSPLANT. (2007) 22 (SUPPL 2): II22-II44.
First-line approach
•
Dietary counselling (sodium restriction).
•
Refraining from food intake during dialysis.
•
•
•
Clinical reassessment of dry weight.
Use of bicarbonate as dialysis buffer.
Use of a dialysate temperature of 36.5
°
C.
•
Check dosing and timing of antihypertensive agents.
Second-line approach
•
•
•
•
•
Try objective methods to assess dry weight.
Perform cardiac evaluation.
Gradual reduction of dialysate temperature from 36.5
°
C downward (lowest
35
°
C) or isothermic treatment (possible alternative: convective treatments).
•
•
Consider individualized blood volume controlled feedback.
Prolong dialysis time and/or increase dialysis frequency.
•
Prescribe a dialysate calcium concentration of 1.50 mmol/l.
Third-line approach (only if other treatment options have failed)
Consider midodrine.
Consider L-carnitine supplementation.
•
Consider peritoneal dialysis.
ICW AND ECW IN CKD
• In CKD patients the BV i ECV stability is maintained by CONSTANT activation of regulatory mechanisms (CKD patients tend to be overhydrated)
• Acute overhydration – ICW stable till BW increse <2%
• In chronic overhydration ICW/ECW returns to normal
Uszko-Lencer NH, Bothmer F, van Pol PE, Schols AM. Measuring body composition in chronic heart failure: a comparison of methods.
Eur J Heart Fail. 2006, 8, 208-214.
CHRONIC OVERHYDRATION: DIAGNOSIS
• Physiological hanges in “functional” ECW (- 2L ubytku; + 5L) are symptomless !!!
• Chronic ECW expansion of up to 8% (1,2 L) is symptomless
• Oedema – TBW > +4% BW (2-4kg) (lungs up to 2L + mesentery and intestinal mucosa)
Woodcock T. E, Woodcock T. M. Revised Starling equation and the glycocalyx model of transvascular fluid exchange: an improved paradigm for prescribing intravenous fluid therapy. Br. J. Anaesth. 2012, 108, 384-394.
Essig M, Escoubet B, de Zuttere D, et al.: Cardiovascular remodelling and extracellular fluid excess in early stages of chronic kidney disease.
Nephrol. Dial. Transplant., 2008, 23 (1): 239-248.
DEHYDRATION EVALUATION: DIAGNOSIS
CLINICAL JUDGEMENET IS THE MOST IMPORTANT ELEMENT IN
OVERHYDRATION ASSESSMENT OF CHRONIC HEMODIALYSIS PATIENT
VASKO R, MÜLLER GA, RATLIFF BB, JUNG K, GAUCZINSKI S, KOZIOLEK MJ: CLIN EXP NEPHROL. 2013; 17: 563–568
OverHydration assessment:
(1) clinical judgment guided by a single clinical examination with
(2) multifrequency bioimpedance analysis (BIA) and
(3) complex systematic clinical approach.
• OHREF (Reference overhydration ), used as a standard, was calculated as the difference between pre-HD weight and DW determined by the managing physicians (dialysis physicians not participating in the study) using the long-term
(weeks to months) systematic clinical approach including patient history, symptoms, laboratory parameters and routine diagnostic techniques
(echocardiography, ultrasonography, chest X-ray), but not BIA.
• OHCLI (Clinical overhydration) represents the clinical judgment of two nephrologists (not involved in the treatment of study patients), which estimated
OHCLI guided by single clinical examination, patients’ history and symptoms.
They were not aware of patients’ DW and laboratory parameters.
CLINICAL JUDGEMENET IS THE MOST IMPORTANT ELEMENT IN
OVERHYDRATION ASSESSMENT OF CHRONIC HEMODIALYSIS PATIENT
VASKO R, MÜLLER GA, RATLIFF BB, JUNG K, GAUCZINSKI S, KOZIOLEK MJ: CLIN EXP NEPHROL. 2013; 17: 563–568
AIC – Akaike’s information criterion, VCCI vena cava collapsibility index
CLINICAL JUDGEMENET IS THE MOST IMPORTANT ELEMENT IN
OVERHYDRATION ASSESSMENT OF CHRONIC HEMODIALYSIS PATIENT
VASKO R, MÜLLER GA, RATLIFF BB, JUNG K, GAUCZINSKI S, KOZIOLEK MJ: CLIN EXP NEPHROL. 2013; 17: 563–568
…“clinical judgment of an experienced physician was the single most significant element in OH assessment, and showed the highest predictive value in combination with other variables…a combination of integrative clinical judgment with routine techniques is a precise and valuable tool in hydration status assessment in HD patients. BIA... may help to identify changes in body compartments not fully appreciated by clinical or biochemical assessment”.
SUMMARY
• VOLEMIA ≠ HYDRATION
• Hypertension hyperhydration verify dry body mass (clinical + bioimedance +
VCCI + chest x-ray)
• Hypertension + euhydration extend diagnostic procedures + medication (BB, ACEi)
• Hypotension – AVOID verify dry body mass (clinical + bioimpedance + VCCI + chest x-ray)
• Reduce ultrafiltration RATE (extended and/or daily HD, HDF)
• Extend diagnosis
• Midodrin?
• If acute replace volume (+ vasopressin?)