Mansfield Delegate Pack 11 march 2014
advertisement

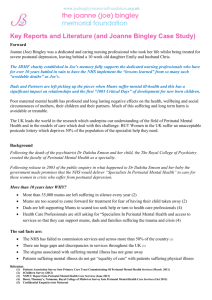
Living with Postnatal Depression A Fathers Story Presented by Chris Bingley Charity Registration Number: 1141638 Where to find this Why I am here …… Mums and Dads at Risk Statistics on postnatal depression show that: 2/3rds of mums will suffer a mood disorder during or after pregnancy: 1 in 2 mums suffer Baby Blues 15% Mums suffer Postnatal Depression 3% Mums suffer Severe Postnatal Depression 1 in 500 Mums suffer Puerperal Psychosis Maternal OCD Maternal PTSD 10% Dads who suffer from PND without treatment 50% Mums suffering in silence to afraid to seek help Based upon 201 ONS Birth Rates UK East Midlands 403,888 27,689 121,166 8,307 24,233 1,661 1,616 111 80,778 60,583 5,538 4,153 • NICE guidelines specify that those who suffer severe postnatal depression should be referred to a specialist perinatal psychiatrist – less than 37% of PCTs commissioned specialist services. • NICE Guidelines state the preferred treatment for severe PND or Puerperal Psychosis is hospitalisation in Mother and Baby Units (MBUs) – less than 91 beds exist with places for a maximum of 593 mums • Whilst 10% Dads suffer Postnatal Depression, Dads are not recognised by NICE – no specialist services are available for Dads either as Sufferers or Carers Dads and “Significant Others” Whilst Health Visitors and Midwives are the primary contact for Mums during pregnancy latest research shows mums are far more likely to turn to their partners for help and support than to Health Care professionals. A survey by Netmums and the Royal College of Midwives (Nov 2012) found: • Mums mainly (42%) turned to their husband or partner when they first talked about how they felt with only a third (30%) first mentioned it to a health professional. • Only a third of mums (30%) were told about the possibility of depression by their midwife and only a quarter ((27%) reported being asked how they felt emotionally during their pregnancy. • Nearly three-quarters (74%) of those surveyed said it often took a few weeks or more likely a few months before they recognised they had a problem. • Over a third of women who suffer depression during pregnancy have suicidal thoughts. The NHS currently does not commission or provide any support for Dads, family members or Significant Others who are expected to provide the support to those suffering from postnatal depression … as insufficient research has been done! Dads as “Carers” The NHS Choices Website gives as an example a “a Carer” is “someone looking after a person between mental health crisis”. "As a new father, it was very difficult. It was time for me to learn everything. • It's expected that 'you are the man' so you can manage. • It's never about how you are feeling, it was all about her. • It didn't matter what you did, nothing was good enough. There was the new baby, we had a new house and all the added other pressures that Michelle use to deal with and, most importantly, my wife's illness. I had to give up work for six months. The isolation was the biggest thing I felt hard to cope with. How was I going to tell my friends if I didn't understand myself? I was exactly like the people who still say "how can you be depressed" - with mental illness, you can't just snap out of it.” Mark Williams www.fathersreacingout.com Fathers Reaching Out aims to help men who suffer from perinatal mental illness and who are left responsible for caring for mums suffering from perinatal mental illness The crucial role “Carers” play, whether dads, partners, family members or friends, must be recognized by service providers…… even though NICE fails to mention “DADS” Best Practice Treatment National Perinatal Mental Health Project Report – A Review of Current Provision (2011) Peurperal Pscyhosis 1 in 500 Mums 1,412 per annum Severe Postnatal Depression 21,187 3% of Mums per annum Mild to Moderate Postnatal Depression 10% to 15% of Mums The Baby Blues 50% of Mums 84,750 per annum 353,124 per annum Numbers based on 706,248 live births in 2009 and the agreed rates of occurence Specialist Perinatal Mental Health Services Mother & Baby Units Specialist Perinatal Psychiatrists Non - Specialist (PNMH) Services Admittance to general psychiatric ward Crisis Home Resolution Teams – “gatekeepers” NHS Integrated Care Networks (Examples) Nottingham, Southampton, Birmingham, Glasgow, etc. Non-specialist services - lead by PNMH Champions with support of GP’s, Midwives, Health Visitors, Care Workers, volunteers, etc. 3rd Sector Support (Examples) Family Action - support program & befrienders Net Mums - online CBT & chat rooms House of Light - call-line and drop in groups Joanne Bingley Memorial Foundation raising awareness, training & education Joanne’s Story: A Reason to Act What’s Going Wrong ? Presented by Chris Bingley Charity Registration Number: 1141638 What’s going wrong? Why ? A National Scandal Mums and Dads at Risk Joe’s Pathway to Despair The NHS Response After Joe Died The Utter Devastation of Loss Support Following Bereavement The Independent Investigation The Coroners Inquest The “Lessons not Learned” The Francis Enquiry The True Costs of Failure The Consequences of Failure Why I am here Best Practice Treatment Why ….? Why Joe? • Joe was dedicated and caring nursing professional • Trained initially through Huddersfield Royal Infirmary to qualify as a Registered Nurse and then deciding to complete an Honours Degree at Huddersfield University • She spent 20 years working at Huddersfield Royal Infirmary where she was Sister on day surgery. • Her funeral attended by over 400 people included ex-patients and many of her colleagues from HRI • I felt all their eyes on me asking the same question that I kept asking myself… Why ? A National Scandal The death of Joanne (Joe) Bingley highlights a national scandal Over the last 10 years, despite Ministerial promises, the development of NHS Service Frameworks and NICE Guidelines the NHS has failed to commission Perinatal Mental Health Services across more than 50% of the country. • The Care Quality Commission has reported that 2/3rds of maternity Services are acting unlawfully, failing to follow care quality standards, • The Patients Association Survey found more than 50% of Mental Health Services are acting in breach of care standards – – – – failing to follow care quality standards,, failing to employ the required specialist perinatal psychiatrists,] failing to provide information to patients Failing to monitor compliance to care stanfards • 35,000 mums suffering in silence every year too scared to seek help (i.e. half of all mums affected by mild to moderate postnatal depression). • 86% of mums suicides whilst suffering mental illness are “avoidable deaths” • 10% of Dads suffer from PND but the NHS provides no support Joe’s Pathway to Despair ...1 of 3 • 2008 Previous termination, miscarriages and treatment for depression documented in Health Visitor records – NONE of the 5 mental health risk assessments described in the Kirklees Maternal Mental Health Care Pathway as the responsibility of Health Visitors completed, in breach of care quality standards and safe systems of work. • 18 Feb 2010 Emily Jane Bingley Born after 5 days in labour • 22 Feb 2010 Breast Feeding problems – 1st Hospital stay with positive results • 10 Mar 2010 Breast Feeding problems – 2nd Hospital stay • The medical records detail Joe’s un-consolable crying, anxiety, feelings of failure and the suspicions of Midwife she was suffering postnatal depression. But no clinical risk assessments completed, no referral and no information given to patient or husband • Treatment for her lack of hind milk and crying baby was to have Joe connected to a milk pump between feeds with intent to increase milk production over 10 days. • Treatment concentrated solely on the problems of Joe continuing to breast feed. • 14 Apr 2010 Easter Holiday emotional breakdown • GP diagnosis and starts drug treatment for Postnatal Depression and lack of sleep • 22 Apr 2010 Suicidal feelings and intent – plans to drive herself and baby into a wall • GP listens to options considered but ruled out as they would not guarantee death • Mental Health Crisis Team contacted, diagnosis severe postnatal depression Joe’s Pathway to Despair …2 of 3 • 22nd April - At initial assessment home care recommended as course of treatment with no other treatment options considered or discussed. No written information of any kind provided nor any information on support groups or how to care for wife. • 23rd April - Care Plan provided to the patient and the husband marked as provided to ‘The Carer’. But no information provided about ‘Carer Rights’ and no ‘Carers Risks Assessment’ as required by The Carers Acts, in breach care quality standards • At no point is any referral made to specialist perinatal psychiatric services or to a consultant of any kind, in beach of care quality standards and NHS Frameworks • 27th April – The Independent Investigation states that the clinical evidence substantiate that Joe should have been hospitalised at least 3 days before she died: Coroners Evidence regarding the visit by the Care Team that day: When Joe requested “please take me with you” her request was ignored and brushed aside by the care worker treating her that day. and Joe left the session in frustration (withdrawing from the treatment). Despite Joe’s medical record detailing her suicidal plans, a decline in mental health and her obvious state of anxiety the care worker never explored Joe’s state of mind even though she admitted to recognising a break-down in Joe’s relationship with her husband. Whilst sat in her car ready to leave, the husband (Chris) knocked on the care workers window to explain Joe had left the property without telling anyone. Despite having recorded the husband’s anxiety and distress in her notes, knowing his wife was suicidal, she told him to contact the police if his wife did not return and then drove away! Joe’s Pathway to Despair …3 of 3 • 29th April • Mental Health Crisis Team Dr and Nurse visit AM – husband (The Carer) not attending but patients mother in attendance: • The Dr for the first and only time during the entire treatment records signs of improvement, and decides there is no need to discuss alternate treatments • Health Visitors visit PM - husband (The Carer) not attending but paternal grandparents in attendance: • Recorded high levels of anxiety, despair, inability to cope, her feelings that mental health service wasting her time and her intent to withdraw from care • HV contacts Crisis Team Manager who over rules HV concern and ignores risks • HV raises her concerns of HV’s being unable to cope as she is told Crisis Team is planning to stop providing support, and she contacts her manager to log risks. • No-one contacts Husband (The Carer) to inquire of patients state or discuss risks prior to the Bank Holiday weekend. • 30th April 2010 - Joanne walks on railway tracks, throwing herself under a train • 4th May 2010 - On first day back at 9:05am the Crisis Team Manager contacts the Health Visitors, the medical records detail the purpose was to explain that at no time did Joanne show suicidal intent else they (The Crisis Team) would have taken action. The NHS Response after Joe died • Huddersfield Royal Infirmary - Excess stamp duty to pay for - Letter of condolences and apology for your loss • Mental Health Crisis Team Admin Dept - Patient Satisfaction Questionaire - Reminder to complete Patient Satisfaction Questionaire • • Mental Health Crisis Team Manager in discussion recorded by Health Visitors: - Patients husband has family support so do not contact for 6 to 8 weeks - Support for Crisis Team staff and HV staff affected by Joe’s death was to be organised through normal channels Mental Health Crisis Team Director and Manager - in a meeting held in the patients home with her husband and GP friend, prior to investigating Joe’s death: “Guidelines are just guidelines we don’t have to follow guidelines” “ These things just happen” The Utter Devastation of Loss ! 1 Corinthians 13: ….faith, hope and love; and the greatest of these is love ! • Love ….. your best friend is gone, taken herself away from you • Hope ….. there is none, your dreams and plans destroyed • Faith ….. shattered by the knowledge that these are “avoidable deaths” When nothing is left what do you live for? • Emily ….. Was too young to have a bond, babies just cry, eat, sleep and pooh! • What do you do when there is nothing left ……. what would you do ? Grief is a process ……. you have to keep going to get through it? • Everything is dark, you can see no end, you have to find strength within you • You find help … and follow a path …. until you find light and yourself again http://www.uk-sobs.org.uk/ Support following Bereavement Support for those whose life’s are left in tatters after bereavement needs to be dramatically improved. I had to learn for myself, without any NHS support, about the significant effects on my daughters long-term development that are expected as a result of the trauma her mother suffered and the impact it has had on her childhood development. Emily is • 12 times more likely to have a statement of special needs prior to age 16 • More likely to have a diagnosis of depression prior to age 16 I also had to learn of the increased risk she will suffer the same severe form of postnatal depression as her mum……… FROM 3% TO 6%“ Whilst there is a greater risk that my daughter will get knocked down by a bus at least IF that happened the universal service across the UK will provide acute care within the critical 60 minute window……. with PND > 50% of the UK has no access to acute care ! Survivors of Bereavement by Suicide http://www.uk-sobs.org.uk/ Winstons Wish http://www.winstonswish.org.uk/ The Independent Investigation Due to time constraints placed upon the investigation by the NHS it was agreed: • The investigation team was only able to review the clinical documentation, policy documents and staff written statements and records, without the benefit of investigators interviewing staff. • As the NHS were unable to identify investigators in Midwifery or Health Visiting, these areas were supposed to be reviewed and investigated at a later stage. The Results: 21 recommendations and actions for change including: •Specialist Perinatal Psychiatric Resource •New strategies and policies compliant to care quality standards •New and improved systems, processes and safe systems of working •Provision of written information to patients and carers •Mandatory contractual care standards and compliance measures The Independent Investigation concludes: “From the documentation there is evidence that Joanne Bingley should have been hospitalised on the 27th of April 2010 at least 3 days before her death. Further if she had been so treated would probably have made a full recovery” Coroners Inquest The criminal standard of proof beyond reasonable doubt, represents the evidential hurdle or threshold that the coroner had to consider for suicide or unlawful killing. He resolved to return a narrative verdict, and his 21 statements of fact include: • A personal and family history of mental health problems as well as significant adverse life events befalling her in the last 5 years of her life. • By the 22nd April her condition was such that she was referred to the Mental Health Services who responded promptly. At and around this time she was expressing suicidal ideation, low mood, anxiety and a poor sleep pattern. • At a meeting it was determined she could be treated at home. I have found as fact that no discussion of other therapeutic options took place………informed consent has not been obtained. (one of many unlawful acts) • Independent medical care advice commissioned from Dr Oates and Mr Ketteringham. I have accepted their view that the possibility of admission should have been part of the initial treatment care plan and discussed with the patient and her husband as a treatment option if she either became worse or did not improve. • I find as fact that her health fluctuated and did not improve. • It is also their evidence that on the 27 April, if not before, there was clinical indication to be admitted to a Mother and Baby Unit. • It would follow from this opinion that if admission had taken place Joanne Bingley in all probability would not have died on the date or in the manner that she did. The “Lessons not Learned” In December 2013, a little over 2 years after the Corners Inquest, the NHS Director of Nursing from the NHS trust that treat Joanne Bingley finally admitted in a statement issued into court that: • In all probability had specialist perinatal psychiatric treatment been offered, including the admittance to hospital in a specialist mother and baby unit, it would have been accepted. • Had specialist treatment been provided the patient, Joanne Bingley, would have been expected to make a full recovery. • Their (NHS Trusts) breach in duty of care was the probable cause of death Joanne (Joe) Bingley’s death was one of many avoidable deaths every year. The Independent Investigation into her death resulted in 21 recommendations for improvement and the NHS agreed an action plan with her husband to implement the “lessons learned” by September 2011. In April 2012 the Care Quality Commission reported on the NHS Trust that treated Joe: • Following complaints raised by the husband of a patient who had deceased (Joanne Bingley) their investigation found the NHS Trust had failed to implement “Lessons Learned” to acceptable care standards • Women in this specific user group (mums suffering severe PND) at risk • 2 other mums, being treated at home for severe PND, have since killed themselves The Francis Enquiry For the NHS to ‘place the quality of patient care, especially patient safety, above all other aims’ we must have candour when mistakes happen and acknowledge all medical errors. • Only 24 per cent of the 140 possible contributory factors identified by the inquiry team had been identified in local investigations at the time of the incidents. • So 76 per cent of the learning from the incidents had been missed; a situation that there is an urgent need to improve. • As well as the new statutory duty of candour, greater use will be made of incident data, including a commitment for CQC to consider each hospital’s review of serious untoward incidents as part of its pre-inspection activity. • NHS England is to launch a program of new patient safety collaboratives, which will be expected to provide expertise on learning from mistakes and help to provide a ‘rigorous approach to transforming patient safety’. “Avoidable Deaths” cost the economy in excess of £300m every year…. But this excludes costs of NHS negligence claims as currently £18bn is spent on fighting negligence claims, 1/5th of NHS Budget. The True Costs of Failure The costs of just one “avoidable death” like Joe’s would cover the costs of providing all mums and dads with the information they require and the extra mother and baby unit beds needed. The estimated cost of the emergency response (£2m) and the economic costs of closing the Trans-Peninne train line for several hours (£20m), hardly feels relevant when compared to the widespread human costs. Proper care would have cost: 15p for the JBMF information card for mums & dads (900,000 *25p = £176,000 per year for all mums) 2p for the JBMF Severe Postnatal Depression checklist/leaflet (22,000 @ 5p = £1,000 for all sufferers) just £17,000 for the 56 days treatment Joe needed to live! £318 per day for treatment in a Mother and Baby Unit Bed The sad fact is each year there are up to 66 maternal suicides due to psychiatric causes of which 86% are “Avoidable Deaths” (diagnosis and treatment was possible). A single “Avoidable Death” such as Joanne Bingley cost the economy in excess of £22m and cost the NHS over £1m in legal fees defending for 4 years the negligence claims, irrespective of any payout after finally admitting to a breach in duty of care. The Consequences of Failure The death of Joanne (Joe) Bingley caused horrific trauma to her husband, to Joe’s family and to her friends. But it also had a significant impact on the lives of many others. Many of those who witnessed Joe’s body being torn apart by the train, her internal organs being spread across the tracks, the blood pool that resulted and her upper torso being dragged along the tracks, until the train came to rest. were traumatised: The 2 train drivers off work needing treatment The members of public, off work needing treatment The 7 year old child waiting on the platform to go to school And many other people who had to deal with the incident All this suffering as a result of the NHS staff failing to obtain “informed consent”, failing to provide access to specialist perinatal health services and failing to admit Joe to a specialist Mother and Baby Unit, even though places were available at the time of her death in Leeds, Manchester and Nottingham. Following his wife’s death Chris was driven by his own grief and the despair to find out answers to his questions Why? At the Coroner’s Inquest the true consequences and costs of the failure to prevent what was an “avoidable death” was brought home to me when told of the many others affected, including the 7 year old child who witnessed Joe’s death ! Why I am here …. Why ? • Joe was a dedicated and caring nursing professional • In 20 years working at Huddersfield Royal Infirmary she enjoyed caring and treating those who were ill but also cherished her time mentoring and supporting others • There is a stepped change underway, back to the core values of “caring” and “putting the patient first” • It will take at least 10 years before significant improvements are seen in the provision of Specialist Perinatal Mental Health Services • The 3rd Sector, Family and Mental Health Services must work together to create the Integrated Care Networks required to fill the gaps in mental health care, “provide support for those suffering in silence” and “eliminate the unnecessary suffering” and “prevent the avoidable deaths” that devastate the whole family. Best Practice Treatment National Perinatal Mental Health Project Report – A Review of Current Provision (2011) Peurperal Pscyhosis 1 in 500 Mums 1,412 per annum Severe Postnatal Depression 21,187 3% of Mums per annum Mild to Moderate Postnatal Depression 10% to 15% of Mums The Baby Blues 50% of Mums 84,750 per annum 353,124 per annum Numbers based on 706,248 live births in 2009 and the agreed rates of occurence Specialist Perinatal Mental Health Services Mother & Baby Units Specialist Perinatal Psychiatrists Non - Specialist (PNMH) Services Admittance to general psychiatric ward Crisis Home Resolution Teams – “gatekeepers” NHS Integrated Care Networks (Examples) Nottingham, Southampton, Birmingham, Glasgow, etc. Non-specialist services - lead by PNMH Champions with support of GP’s, Midwives, Health Visitors, Care Workers, volunteers, etc. 3rd Sector Support (Examples) Family Action - support program & befrienders Net Mums - online CBT & chat rooms House of Light - call-line and drop in groups Joanne Bingley Memorial Foundation raising awareness, training & education The Joanne (Joe) Bingley Memorial Foundation Founders Statement How we help Parliamentary Commission into PNMH JBMF – Founders Statement Joanne, or Joe as she preferred to be called, was a nurse with over 20 years experience. She was dedicated, caring and diligent as are most health care professionals I have met. But Joanne was let down by the very NHS organisation that she gave everything to and just 10 short weeks after giving birth to her much longed for daughter Emily, whilst being treated for severe postnatal depression she took her own life. “The charity exists to ensure future generations such as my daughter have access to the appropriate care and support, that services adhere to care quality standards and to inspire sustainable change in the perception and provision of maternal mental health services in the UK” JBMF – How we help How the foundation delivers it’s aims: • Website and information leaflets - we provide information on what you need to know so dads, grandparents and friends can help. • We publish stories in national media, Twitter, Facebook and our website to encourage open discussion and raise awareness • Knowledge of ‘Best practice’ – legislation, care quality protocols, befriender and peer support groups, self help, supervision, etc; presenting at seminars and workshops to inform commissioners, dept health, parliament, etc. on patient and service issues. • We provide training & education workshops for professional health care workers and volunteers • We have supported research including: • The Patients Association survey of Primary Care Trusts • Kings College User Group • Through links with MP’s and other organisations we inform NHS policy makers and parliament of service user issues and expectations • Supporting the Maternal Mental Health Alliance we work with other organisations to deliver improvements in PNMH services. Parliamentary Commission Into Perinatal Mental Health Proposed Scope and Terms of Reference: The inquiry will provide an independent review and detailed investigation to understand and highlight policy areas and issues Why? has there been a failure to implement Specialist Perinatal Mental Health Care Services across the UK following parliamentary promises after the death of Daksha Emson. Why? has there been a failure to implement “lessons learned” from Independent Investigations Why? Dads and Significant Others are not recognised as Carers by NICE even though “Home Care” is the primary treatment offered by Mental Health Crisis Teams What? are the implications and costs to society and the economy: • Mums - Unnecessary Suffering in Silence and Avoidable Deaths • Dads - Suffering from PND and Caring for Partners • The breakdown of Family Relationships • Early Years Child Development • General Public • Businesses Productivity and Employer Costs What? are the recommendations and actions to reduce “the costs to society and the economy ” of the “unnecessary suffering” and “avoidable deaths” Finally Charity Registration Number: 1141638 Uncovering the truth “What I have uncovered about mental illness and the issues around it during my investigations and enquiries is both tragic and shocking. It is my hope and desire that by openly publicising the horrendous treatment given my wife and I that other people come forward and support my call for the implementation of the care standards and “lessons learned” required to prevent such catastrophic Never Events happening again.” Chris Bingley Founder My Inspiration My Inspiration: • Anthony Harrison, Angela Harrison Trust , on asking how he coped? “You make it through the grief somehow ……but the loss never leaves you” • Dr Margaret Oates, author of the Independent investigation into Joe’s death, on reporting the findings that Joe’s was yet another “avoidable death” “It needs someone who has suffered to stand-up and shout out …… .. people listen to patients with a voice….it’s a powerful voice” • Katherine Murphy, The Patients Association Chief Executive , on completing the survey showing the failure to commission services across over 50% of UK “We need one voice …. professionals, charities and user organisations together” • Albert Pike, What we have done for ourselves alone dies with us; What we have done for others and the world remains and is immortal Why I am here …… Why are you?