Blood Collection
advertisement
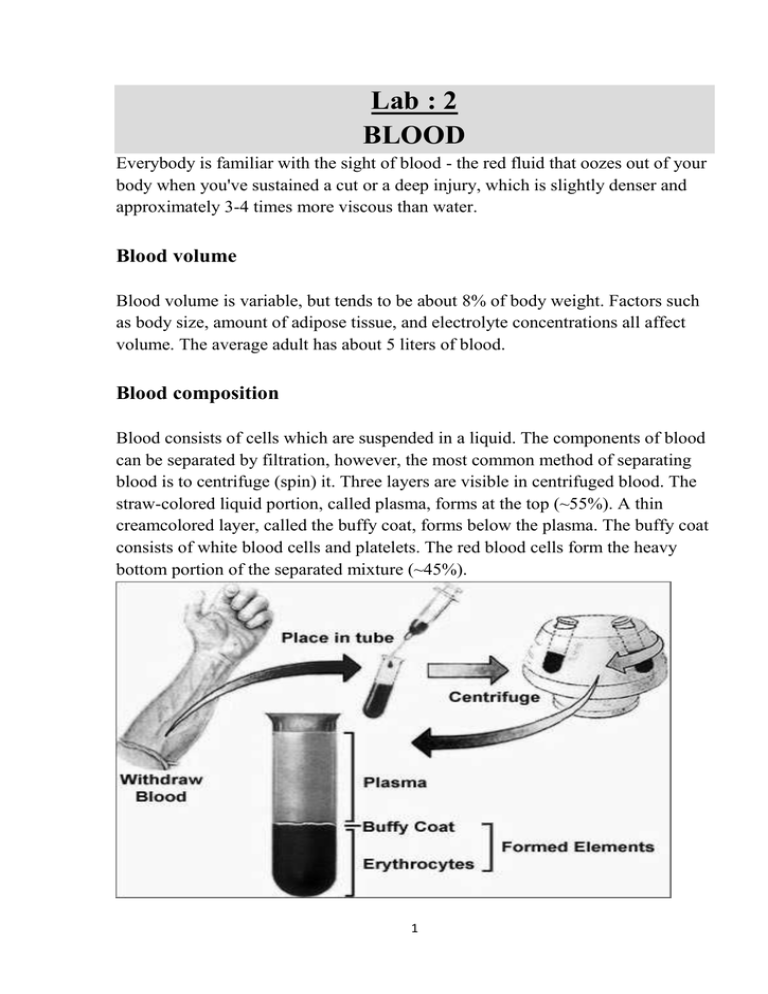
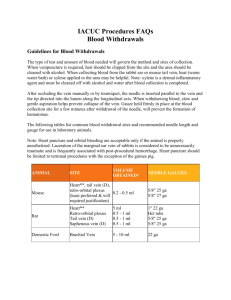
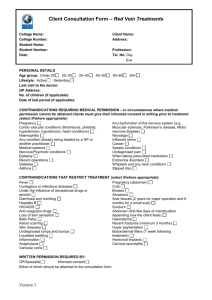
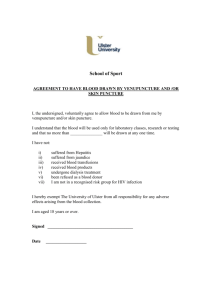
Lab : 2 BLOOD Everybody is familiar with the sight of blood - the red fluid that oozes out of your body when you've sustained a cut or a deep injury, which is slightly denser and approximately 3-4 times more viscous than water. Blood volume Blood volume is variable, but tends to be about 8% of body weight. Factors such as body size, amount of adipose tissue, and electrolyte concentrations all affect volume. The average adult has about 5 liters of blood. Blood composition Blood consists of cells which are suspended in a liquid. The components of blood can be separated by filtration, however, the most common method of separating blood is to centrifuge (spin) it. Three layers are visible in centrifuged blood. The straw-colored liquid portion, called plasma, forms at the top (~55%). A thin creamcolored layer, called the buffy coat, forms below the plasma. The buffy coat consists of white blood cells and platelets. The red blood cells form the heavy bottom portion of the separated mixture (~45%). 1 1-The plasma The Plasma is a straw colored liquid, most of which is water. It makes up 55% of the blood and serves as a transport medium for blood cells and platelets. By far the greatest constituent of plasma is water, which accounts for >90% of the total volume. Other constituents fall into the following main categories: Ions (Na+, Cl-, etc) Plasma proteins (albumins, globulins, fibrinogen, etc) Dissolved gases (O2, CO2) Circulating Nutrients (glucose, amino acids, etc) Circulating Tissue products (urea, creatinine, lactate, etc) Circulating Hormones (insulin, adrenaline, etc) The water in the plasma is an important solvent for ions such as Na+, Cl-, K+, etc. It also dissolves nutrients like simple sugar, lipids, amino acids and vitamins. Sometimes, it would help transport enzymes and hormones, but that depends on the activities of the body. Serum: Plasma differs slightly from what is termed serum, which is generally taken to mean the fluid part of the blood which remains after the blood has coagulated (clotted). 2-The red blood cells The red blood cells form a major part of the blood. These are the familiar discotic shaped cells which make up 99% of the cells in the blood. They are the principal carriers of the red colored hemoglobin molecules. Hemoglobin is an iron containing protein and binds about 97% of all oxygen in the body; hence, the most principled function of red blood cells is to carry oxygen gas around the body. Although they do carry a little carbon dioxide sometimes, most of this unwanted gas is transported by the plasma 3- The white blood cells The white blood (leukocytes) cells are a vital source of defense against external 2 organisms. White blood cells also serve as 'sanitary engineers' cleaning up dead cells and tissue debris that would otherwise accumulate to and lead to problems. There are five classes of leukocytes: neutrophil, eosinophil, basophil, monocyte and lymphocytes. 4-The platelets These are not true cells but fragments of cytoplasm from certain bone marrow cells. They play a part in the clotting of blood. Plasma and platelets in clotting: If damage occurs to a blood vessel, circulating platelets immediately get trapped at the injury site. On accumulating the platelets 'plug' the leak in the vessel providing a first step in damage control. This mechanism is supplemented by 'blood coagulation', or clotting, which is the most important means of defense against bleeding. As mentioned plasma contains several dissolved proteins. Fibrinogen is a rod shaped soluble protein which in the presence of a catalyst thrombin gets converted to an insoluble protein fibrin. The combined action of the platelets and 'fibrin web' is sufficient to prevent a dangerous loss of blood. In cases where the formation of fibrin and hence formation of a clot is impaired due to some reason (e.g. a genetic disorder as in hemophilia) a person is at great risk of bleeding to death. BLOOD CELLS 3 ANTICOAGULANTS Most hematology and coagulation procedures must be performed on whole blood or plasma. There for, as soon as the blood is withdrawn from the patient, it is mixed with an anticoagulant to prevent coagulation. The three most commonly used anticoagulants in the hematology laboratory are discussed below: 1-EDTA Is generally available as the sodium, dipotassium or tripotassium salt of ethylene diamine tetra acetic acid. It is used in concentration of 1.5(±.25). EDTA prevents coagulation by binding the calcium in the blood (calcium is required for blood coagulation). Excessive concentration of EDTA cause: 1- 2- Shrinkage of the red blood cells leading to decreased hematocrit increased MCHC, falsely low ESR. Degenerative changes in the white cells and the platelets will swill and break up causing a falsely increased in platelet counts. 2-Sodium citrate Is used for coagulation studies in a concentration of 1 part 0.109M sodium citrate (tri sodium citrate dehydrate) to9 part whole blood. Sodium citrate prevents coagulation by binding the calcium of the blood in a soluble complex. 3-Heparine May be used in concentration of 15 to 30 units/ml of whole blood. its may cause clumping of platelets and white cells. Coagulation is prevented by interaction with anti thrombin III and subsequent inhibition of thrombin. 4 Blood Collection The medical technologist most often comes in contact with a patient during the process of blood collection. The patient in a hospital is anxious, fearful, and in ill health. He is anxious about his physical condition; he fear because he does not know what will happen next; his disease may or may not be life threatening; and he is physically uncomfortable as a result of his disease or injury. He is also separated from his family. For these reasons it is important for the medical technologist to show the patient at all time the kindness and understanding that can mean so much. When the technologist is dealing with a child his approach is doubly important. This may be the first time the child has had a blood test. If it turns out to be terrible experience it will be remembered and feared for the child for many years. Therefore it is important to gain the child trust before proceeding with blood collection. The child should be informed of what is going to happen; if the child is told that the puncture will not hurt the child trust will be lost because this statement is generally is not true. Blood specimens are commonly obtained from patient's vein (Vein puncture). Under some circumstances a skin puncture will be used for this purpose. Irrespective of the method used certain techniques are common to all phlebotomy procedures: 1- Check the request form: A requisition form must accompany each sample submitted to the laboratory. This requisition form must contain the proper information in order to process the specimen. The essential elements of the requisition form are: Patient's surname, first name, and middle initial. Patient's ID number. Patient's date of birth and sex. Requesting physician's complete name. Indicating the test(s) requested. Source of specimen. This information must be given when requesting microbiology, cytology, fluid analysis, or other testing where analysis and reporting is site specific. Date and time of collection. Initials of phlebotomist. 5 2-The correct patient identification: Is critical for hospital patients this is accomplished by checking the identification wrist band for the correct name and hospital identification number. The procedure for out patient is not as easy. The phlebotomist should ask the patient for his or her full name and any other information specific for the patient that can be verified by the requisition form. 3-The correct specimen identification: A properly labeled sample is essential so that the results of the test match the patient. The key elements in labeling are: Patient's surname, first and middle. Patient's hospital identification (ID) number. Date, time and initials of the phlebotomist must be on the label of each tube. 4- Safety and infection control Because of contacts with sick patients and their specimens, it is important to follow safety and infection control procedures. PROTECT YOURSELF Wear gloves and a lab coat or Change gloves after each patient or when contaminated. Wash hands frequently. Dispose of items in appropriate containers. Dispose of needles immediately upon removal from the patient's vein. Do not bend, break, recap, or recapped needles to avoid accidental needle puncture or splashing of contents. Clean up any blood spills with a disinfectant such as freshly made 10% bleach. If you stick yourself with a contaminated needle: o Remove your gloves and dispose of them properly. o Squeeze puncture site to promote bleeding. o Wash the area well with soap and water. o Record the patient's name and ID number. 6 PROTECT THE PATIENT Place blood collection equipment away from patients, especially children and psychiatric patients. Practice hygiene for the patient's protection. When wearing gloves, change them between each patient and wash your hands frequently. Always wear a clean lab coat or gown. 5- Preparation of the puncture site: The puncture site should be cleaned by rubbing vigorously with a pad moistured with 70% isopropanol. The area is the dried with sterile gauze. Once the phlebotomy site has been cleaned the decontaminated area should not be touched. MICRO SAMPLE TECHNIQUE Micro sampling refers to blood collection by skin puncture and is frequently used in the following types of patients: 1- Infants less than 6 months of age generally don’t have a large blood supply, and it is dangerous to remove the volume of blood involved in vein puncture. 2- In young children: If only a small amount of blood is needed, a skin Puncture is performed on the finger. 3- When an adult has poor veins, when the veins can't be used of intravenous (IV) infusions, or in the case of a severely burned patient the patient, the patient, the finger may be used as a phlebotomy site. Reagent and equipment: 70% isopropyl alcohol. Sterile gauze pads - for application on the site from which the needle is withdrawn. Gloves - can be made of latex, rubber, vinyl, etc.; worn to protect the patient and the phlebotomist. Sterile disposable blood lancet 7 Procedure: Follow the procedure as outlined above for greeting and identifying the patient. As always, properly fill out appropriate requisition forms, indicating the test(s) ordered. Verify the patient's condition. Fasting, dietary restrictions, medications, timing, and medical treatment are all of concern and should be noted on the lab requisition. Position the patient. The patient should sit in a chair, lie down or sit up in bed. Hyperextend the patient's arm. Location of the puncture site: The best locations for finger sticks are the 3 rd and 4 th fingers of the nondominant hand. Do not use the tip of the finger or the center of the finger. Avoid the side of the finger where there is less soft tissue, where vessels and nerves are located, and where the bone is closer to the surface. The 2nd (index) finger tends to have thicker. The fifth finger tends to have less soft tissue overlying the bone. Avoid puncturing a finger that is cold or cyanotic, swollen, scarred, or covered with a rash. When obtaining blood from infants less than 1 year of age, blood is generally obtained from the heel of the foot. The site chosen should be on the inside (medial) or the outside (planter surface) of the foot. An imaginary line may be drawn from the middle of the large toe to the heel, and a line from between the fourth and the fifth toes of the heel. The area outside of these two lines is acceptable for puncture. The puncture depth: For finger stick, the puncture should be no deeper than 3.1 mm because the distance between the skin surface and bone will vary from 3.1 to 10.9 mm. The distance to the bone is only 1.5 to 2.4 mm in infants 6 months old, so the finger is not used in this age group of infants unless special devices are used. For the heal puncture The depth of the puncture at any time must not be 8 more than 2.4 mm in order to avoid damage to the bone. Because the blood supply for the infant's heal is located between 0.35 and 1.6mm below the surface of the skin, the puncture need not to be any deeper than 1.6 mm. Performance of a skin puncture: The puncture site should not be cold; otherwise it must be warmed either by rubbing the site, hanging the hand or applying hot gauze on the puncture site. Using a sterile lancet, make a strong, fast and deep skin puncture just off the center of the finger pad. The puncture should be made perpendicular to the ridges of the fingerprint so that the drop of blood does not run down the ridges. Wipe away the first drop of blood, which tends to contain excess tissue fluid. Collect drops of blood into the collection device by gently massaging the finger. Avoid excessive pressure that may squeeze tissue fluid into the drop of blood. 9 Have the patient hold a small gauze pad over the puncture site for a couple of minutes to stop the bleeding. Dispose of contaminated materials/supplies in designated containers. Label all appropriate tubes at the patient bedside. Deliver specimens promptly to the laboratory. Discussion 1. Blood from a skin puncture is a mixture of venous, arterial, and capillary blood. The concentration of some constituents in the blood will differ between skin puncture blood and an arterial or venous specimen. Because of this, test reports should indicate if the blood sample was obtained from a skin puncture. 2. Excessive massaging or squeezing of the finger or foot will cause tissue juice to mix with and dilute the blood. This will result in erroneous and increased clotting of the blood. 3. Since a deep puncture is not any more painful than a superficial puncture, it is best to go deep enough the first time thereby avoid puncturing the patient a second time. 4. Excess crying will affect some test result (most notably, the white blood cell count may increase considerably). It is advisable to wait 30minutes to 1 hour following a crying episode before obtaining the blood specimen. 5. The thumb, big toe, and ear lob should not be used as a skin-puncture site for phlebotomy. 10 6. Misidentification of a patient is series error and can have disastrous implication for the patient. 7. Betadine (iodine) should not be used routinely to clean the phlebotomy area because contamination with this substance will cause some erroneous test results (falsely elevated potassium, uric acid, and phosphorus results). 8. Skin must be dried before puncture to avoid mixing of blood with alcohol and hemolysis of blood, and to avoid hemoconcentration. 11 VEINPUNCTURE A veinpucture must be performed with care. The veins of a patient are the main source of blood for testing and the entry point for medications, solutions, and blood transfusions. Because there are only a limited number of easily accessible veins in a patient, it is important that everything be done to preserve their good condition and availability. Part of this responsibility lies with the medical technologist. The ideal procedure is to have the patient lie down. If this is not possible, the patient should sit in a sturdy, comfortable chair with his or he arm firmly supported on a table or chair arm and easily accessible to the technologist. A patient should never stand or sit on a high stool during any process of blood collection. Reagent and equipment: Tourniquet. Alcohol Wipes - 70% isopropyl alcohol. Gauze sponges - for application on the site from which the needle is withdrawn. Adhesive bandages / tape - protects the veinpucture site after collection. Gloves - can be made of latex, rubber, vinyl, etc.; worn to protect the patient and the phlebotomist. Sterile disposable syringes, the choice of a syringe are governed by the amount of blood required. Sterile, disposable needle. The choice of needle depends on the size of the vein. The most commonly used needles are 20, 21, and 22 gauge. The higher the gauge number, the smaller the inner diameter (bore) of the needle. The length of the needle also chosen according to the depth of the vein, the most commonly used depth is 1.5 inch. 12 For vaccutainer system: Evacuated Collection Tubes - The tubes are designed to fill with a predetermined volume of blood by vacuum. The rubber stoppers are color coded according to the additive that the tube contains. Various sizes are available. Blood should NEVER be poured from one tube to another since the tubes can have different additives or coatings (see illustrations at end). Needles - The gauge number indicates the bore size: the larger the gauge number, the smaller the needle bore. Needles are available for evacuated systems and for use with a syringe, single draw or butterfly system. Holder/Adapter - use with the evacuated collection system. Needle disposal unit - needles should NEVER be broken, bent, or recapped. Needles should be placed in a proper disposal unit IMMEDIATELY after their use. Procedure: Procedure for vein selection Although the larger and fuller median cubital and cephalic veins of the arm are used most frequently, wrist and hand veins are also acceptable for veinpucture. Palpate and trace the path of veins with the index finger. Arteries pulsate, are most elastic, and have a thick wall. If superficial veins are not readily apparent, you can force blood into the vein by massaging the arm from wrist to elbow, tap the site with index and second finger, apply a warm, damp washcloth to the site for 5 minutes, or lower the extremity over the bedside to allow the veins to fill. Performance of a venipuncture: Approach the patient in a friendly, calm manner. Provide for their comfort as much as possible, and gain the patient's cooperation. Identify the patient correctly. Properly fill out appropriate requisition forms, indicating the test(s) ordered. Verify the patient's condition. Fasting, dietary restrictions, medications, timing, and medical treatment are all of concern and should be noted on the lab requisition. 13 Prepare the blood collection assembly, the needle is firmly adjusted to the tip of the syringe, a check is then made to see that the plunger is not stick with the barrel. Position the patient. The patient should sit in a chair, lie down or sit up in bed. Hyperextend the patient's arm. Apply the tourniquet 3-4 inches above the selected puncture site. Do not place too tightly or leave on more than 2 minutes. The patient should make a fist without pumping the hand. Select the veinpucture site. 14 Median basalic Median Cephalic Cephalic vein Prepare the patient's arm using alcohol swab Cleanse in a circular fashion, beginning at the site and working outward. Allow to air dry. Grasp the patient's arm firmly using your thumb to draw the skin taut and anchor the vein. The needle should form a 15 to 30 degree angle with the surface of the arm. Swiftly insert the needle through the skin and into the lumen of the vein. The needle should be in the bevel up position (needle opening facing upward). When the last tube to be drawn is filling, remove the tourniquet. Remove the needle from the patient's arm using a swift backward motion. Press down on the gauze once the needle is out of the arm, applying adequate pressure to avoid formation of a hematoma. Dispose of contaminated materials/supplies in designated containers. Mix and label all appropriate tubes at the patient bedside. Deliver specimens promptly to the laboratory. 15 Discussion: 1. There are certain areas are to be avoided when choosing a site of vein puncture: Extensive scars from burns and surgery - it is difficult to puncture the scar tissue and obtain a specimen. The upper extremity on the side of a previous mastectomy - test results may be affected because of lymphedema. Hematoma - may cause erroneous test results. If another site is not available, collect the specimen distal to the hematoma. Intravenous therapy (IV) / blood transfusions - fluid may dilute the specimen, so collect from the opposite arm if possible. Otherwise, satisfactory samples may be drawn below the IV by following these procedures: 16 Turn off the IV for at least 2 minutes before veinpucture. Apply the tourniquet below the IV site. Select a vein other than the one with the IV. Perform the veinpucture. Draw 5 ml of blood and discard before drawing the specimen tubes for testing. 2. Hematoma forms under the skin adjacent to the puncture site - release the tourniquet immediately and withdraw the needle. Apply firm pressure. Causes of hematoma: The needle may have gone through the vein. Remove the needle before removing the tourniquet. The needle may not fully penetrate the upper most wall of the vein. (Partial penetration may allow blood to leak into the soft tissue surrounding the vein by way of the needle bevel). Failure to apply pressure to the veinpucture site. 3. To prevent hemolysis (which can interfere with many tests): Mix tubes with anticoagulant additives gently 5-10 times Avoid drawing blood from a hematoma Avoid drawing the plunger back too forcefully, if using a needle and syringe, and avoid frothing of the sample Make sure the veinpucture site is dry Avoid a probing, traumatic veinpucture Massaging, squeezing, or probing a site 17 4. Prolonged tourniquet application (no more than 2 minutes) may cause: Hemoconcentration which is defined as increased concentration of larger molecules and formed elements in the blood of non-filterable elements (i.e. proteins). May lead to vein collapse. Tissue ischemia. 5. Air must never be pumped into a vein because a few cubic centimeters of air pumped into a vein could cause death. 6. Plunger of syringe must not be pulled pack with too much force, to avoid hemolysis of blood, or the force may pull the wall of the vein down on top of the bevel of the needle causing the blood flow to stop. 7. A technologist should not stick a patient more than two times. If the blood sample has not been obtained after the second trial, it is advisable to call another technologist. By this time, both you and the patient have lost confidence. 8. In some instances, it is almost impossible to locate a vein in the arm. In such cases, the veins of the lower arm, wrist, or hand may be used. The technologist should not perform a vein puncture in the ankle or foot. 9. When a vein puncture must be carried out on a small child, it is very important to release the tourniquet when the blood stars to enter the syringe. Children's veins are small and collapse quickly because blood is removed from the vein faster than enters it. 10. If an incomplete collection or no blood is obtained: Change the position of the needle. Move it forward (it may not be in the lumen) Or move it backward (it may have penetrated too far). 18 Adjust the angle (the bevel may be against the vein wall). Loosen the tourniquet. It may be obstructing blood flow. Re-anchor the vein. Veins sometimes roll away from the point of the needle and puncture site. 11. If blood stops flowing into the tube: The vein may have collapsed; remove the tourniquet to increase venous filling. If this is not successful, remove the needle, take care of the puncture site, and redraw. The needle may have pulled out of the vein. Hold syringe firmly during drawing blood and keeping the index finger alongside the hub and brancing index on the patient arm. 19