Work with Dangerous Clients
advertisement
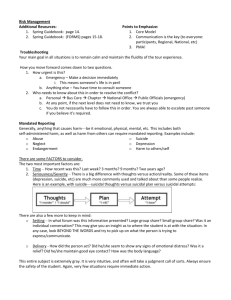
Work With Dangerous Clients G. P. Koocher, Ph.D., ABPP Assess the Patient for: Diagnosis History of violence Demographics Availability of potential victims Access to weapons Substance abuse Stressors Potentially Suicidal Patients Suicide is the most frequent mental health emergency: 1 out of 5 psychologists will lose a patient to suicide 1 out of 6.5 psychology trainees 1 out of 2 psychiatrists There is a heavy emotional toll on both survivors and clinicians Suicide is a frequent cause of malpractice suits 5.4% for psychology and 20% for psychiatry Potentially Suicidal Patients -2 Inpatients Suicide vs. Outpatients is more frequent in a psychiatric hospital setting. Hospitals are generally held to a higher standard than outpatient community practitioners. Few outpatient suicide malpractice cases go to trial. Potentially Suicidal Patients -3 Standard of Care Clinician is not expected to predict and prevent suicide. Clinician is expected to identify elevated risk or suicide and to take reasonable protective and riskreduction steps (where possible). Assessing Competence in Suicide Emergencies and Treatment Licensed professionals are expected to be able to handle emergencies. Practitioners should develop intervention strategies. Additional postgraduate training may be required. Potentially Suicidal Patients -4 Selected Demographics of Suicidal Patients 1.4% of all deaths are suicides. Adolescents and people over 65 are the most frequent age groups. Completion rate = male to female rate 3:1. Clinical diagnosis and suicide: Over 90% of suicides are associated with mental disorder. Patients with a major mental disorder are 10 times more likely to die by suicide. Potentially Suicidal Patients -5 Diagnoses and Suicide Major affective illness = 15% of deaths. Schizophrenia = 10%. Patients hospitalized for alcoholism = 2-3%. Patients with personality disorders (especially borderline personality) = 8%. Demographics Attempters = 10 - 20 times rate of completers Mainly female, personality disordered, multiple attempts Completers = 50 - 70% communicate intent in advance, chiefly to family members and significant others. Indicators of Suicide Risk History of prior attempts Acute perturbation Incident causing humiliation or shame Hopelessness about future (escape wish) Recent d/c from hospital (1 month/1 year) Constriction in ability to see alternatives to current state (escape wish) Availability of lethal means Chronic medical disorder with persistent pain History of impulsive, dangerous, or self-destructive behavior Strategies to Consider Hospitalization Strengthening the therapeutic alliance Intensifying the treatment Secure weapons Actively manage the patient’s environment Stepwise breaking of confidentiality Warning potential victims Additional protective actions. Indicators of Suicide Risk Contra Indicators to Risk Dependent children Recognition of the pain that suicide would cause relatives and friends Future significant positive events (e.g., wedding or birthday) Elevated Suicide Risk is a low-base rate event. Every patient should be asked about present and past suicidal ideation during the initial intake evaluation. No patient is “too healthy” to ask. Indicators of Suicide Risk Assessment When Ideation Is Present Mental status Plan (including feasibility, lethality, experimental actions, alternative plans) Severity of perturbation Panic attacks and severe insomnia Narrowed Loss rigid thinking of insight Inability to see alternatives to suicide Indicators of Suicide Risk Assessment When Ideation Is Present Information about prior attempts Patient’s perception of risk and ability to contract for safety Hopelessness about the future Available lethal means Availability of working support system Suggestive behavior (intention to die/survive) Feelings about hospitalization Indicators of Suicide Risk Assessment When Ideation Is Present Psychological Testing (e.g., Beck’s Helplessness/hopelessness Scales, MMPI-2) All instruments tend to overpredict No test can predict individual cases Consider testing especially when therapist is inexperienced or has countertransference issues Managed-care instruments may be helpful in accessing treatment resources Advance Preparations for Working With Suicidal Patients Self-Evaluation Personal feelings about suicide Current capacity to deal with suicidal patient Knowledge of Options and Resources Civil commitment criteria and procedures Connections to emergency crisis team, if any Connection to inpatient facilities Relationships with hospital staff Referral process Staff privileges Psychopharmacology knowledge base Advance Preparations For Working With Suicidal Patients-2 Develop Good Relationship With Knowledgeable Physician(s) Insist on medication evaluations Insist that medication recommendations be followed as a condition of your continuing to provide therapy Consult regularly with physician about prescriptions Keep good notes on all of the above Informed Consent With Suicidal Patients Inform patient and family, if appropriate, or responsibility to protect. Informed consent statement should contain notice to patient that you will break confidentially where appropriate, if necessary to protect. “If I believe you are at risk of killing yourself as a way of escaping the emotional pain that brought you to see me, from a therapeutic and human perspective, my only treatment goal is to keep you safe and alive. If this is unacceptable to you, then we probably need to get you to another therapist.” Support Systems and Suicidal Patients When Possible and Appropriate, Involve Significant Others in the Patient’s Treatment Pros and cons vary from person to person and time to time. Can family members be therapeutic allies? Especially important to maintain safety between sessions in outpatient treatment. Consider others such as clergy or friends when family is not available. Document all, even when involvement of others is contraindicated. Interventions With Suicidal Patient: Safety Contracts Commonly used technique with potential clinical value Not very effective risk-management strategy without strong alliance Reliance on contract alone is rarely good practice Doubtful value when patient is impulsive, substance abuser, or prone to decompensate or disassociate If psychologist contracts, must be available on 24/7 basis Interventions With Suicidal Patient: Hospitalization Hospitalization does not “prevent” suicides. Hospitalization may be the only safe intervention for some patients. Five potential conflicts: Good risk management Best clinical care Managed-care perspective Patient perspective Family perspective Interventions With Suicidal Patient: Outpatient Care Crisis Management Includes: Therapeutic activism Increased frequency of sessions and daily check-ins Delay of patient’s suicidal impulses Efforts to increase hope and reasons for living Availability 24/7 or adequate backup Clients must know backup arrangements Covering colleagues must be adequately briefed Interventions With Suicidal Patient: Outpatient Care-2 Maintain regular contact with prescribing physician Sole focus on treatment = safety Remove lethal agents Be alert to sudden changes in behavior Flights into health or decisions to divest Consistently involve significant others Consider day-treatment or other isolationreducing activities Document, document, document The Chronically Suicidal Patient Extraordinarily difficult to treat Suicide may be a part of defensive structure to escape pain Gestures often have secondary gain or are expressions of rage Regular consultation required Highly stressful on clinician; manage own emotional resources Be alert to countertransference Don’t do it if you doubt your own competence Avoid narcissistic feelings of personal responsibility leading to rage and burnout Special Considerations When Treating the Chronically Suicidal Patient Conflict between ability to provide good treatment and avoid abandonment (ES 4.09) 4.09 Terminating the Professional Relationship. (a) Psychologists do not abandon patients or clients. (See also Standard 1.25e, under Fees and Financial Arrangements.) (b) Psychologists terminate a professional relationship when it becomes reasonably clear that the patient or client no longer needs the service, is not benefiting, or is being harmed by continued service. (c) Prior to termination for whatever reason, except where precluded by the patient's or client's conduct, the psychologist discusses the patient's or client's views and needs, provides appropriate pretermination counseling, suggests alternative service providers as appropriate, and takes other reasonable steps to facilitate transfer of responsibility to another provider if the patient or client needs one immediately. Special Considerations When Treating the Chronically Suicidal Patient -2 Appropriate termination is key Consultation is necessary (with both senior colleagues and prescribing physician) Termination during hospitalization may be appropriate Consult with managed-care case manager when appropriate Consider referral to group program Record-keeping When Treating the Dangerous (to Self or Others) Patient Keeping good records is a must. Never alter a record. Include discussions with managed-care company if there is disagreement about frequency of treatment or hospitalization. Think out loud about whether to appeal. Get records of past treatment, especially hospitalizations. Maintain records per legal requirements (nature and duration). Getting Consultation on Dangerous Patients Especially important where hospitalization is rejected by managed- care company. Identify consultants before you need them. Use peer consultation group. Vicarious liability. Arms-length, formal, paid consultation is the best protection. Explore all contingencies and options. Be sure your supervisees and assistants consult with you. Postvention: After the Event In General Self care Bereavement reactions: mourning the patient’s death Safer if done in personal therapy than in consultation Be careful what you say and to whom; limit selfrecrimination to confidential relationships Post-mortem conferences Becoming a standard practice for managedcare companies and hospitals Can be helpful for closure Insist on complete confidentiality protections with written assurance from company or agency attorney. Postvention: After the Event With Patient’s Family Often an important risk management tool and a helpful thing to do. Important part of therapist’s own coping. At funeral or in giving condolences, avoid revealing your status and remain in background. Any substantive interaction with patient’s family should be in private. Avoid doing more than condolences until own feelings are worked through. Be aware of confidentiality issues that survive patient’s death. Postvention: After the Event With Patient’s Family Executor/heirs at law may waive privilege. Good idea to get waiver from family With appropriate waiver therapist may discuss case in general, but may also withhold details the patient would have wanted kept private. Do not provide records without valid subpoena. Demonstrate that therapist cared about patient and empathizes with loss. Any sessions should be supportive and psychoeducational. Postvention: After the Event A Session With Patient’s Family Focus session on grieving process and its importance If treatment is needed, refer to someone else. Survivors’ coping may include anger at therapist. Referral may feel like abandonment. Decision Model per Leon VandeCreek Break Confidentiality High Build rapport Involve significant others Hospitalize Intensify therapy and Manage environment Violence Risk Low Build Rapport Weak Shift focus to violence management Therapeutic Alliance Strong