- Integrative Medicine - University of Texas Medical Branch
advertisement

Translating the evidence about mindbody medicine into practice: Barriers
and issues in training
Victor S. Sierpina, M.D.
W.D. and Laura Nell Nicholson Family Professor
of Integrative Medicine
Professor, Family Medicine
University of Texas Medical Branch
Co-Investigators
Ruth Levine, MD
Professor of Psychiatry
University of Texas Medical Branch
John Astin, PhD
Senior Scientist
California Pacific Medical Center
San Francisco, CA
Alai Tan, MD, PhD
Assistant Professor
Office of Biostatistics
Department of Preventive Medicine and Community Health
University of Texas Medical Branch
Developmental Project 4
Barriers to Translation of Mind-Body Therapies to
Training and Practice in Family Medicine and
Psychiatry
Victor S. Sierpina, M.D.,
Ruth Levine, M.D.
John Astin, Ph.D.
• This project will identify barriers to evidence-based,
mind-body medicine being regularly taught in
training or implemented into practice
Developmental Project 4—Aims
• To survey residents and faculty at UTMB in family
medicine and psychiatry programs comparing
specialty responses.
• Introduce mind-body skills groups and training into
both family medicine and psychiatry residencies.
• Perform a subsequent national survey of family
medicine and psychiatry residency program directors
and chief residents
Working hypotheses
•
•
A number of specific factors can be
identified that block the integration of
MBM into patient care.
Personal exposure to MBM techniques
and experiences will improve the
acceptance of these methods among
clinicians.
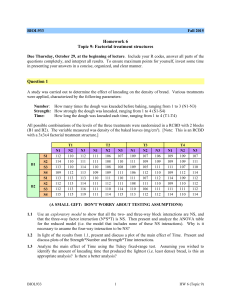
Barriers To Translation Model
• Informed by qualitative, quantitative studies
and literature review
• Survey designed around identified items
from focus groups*
*{Astin JA, Goddard T, Forys K. Barriers to the integration of mindbody medicine: Perceptions of physicians, residents and medical
students. EXPLORE: The Journal of Science and Healing. 2005}
From Research to Health Outcomes:
Translation Blocks to Mind-Body Medicine
CLINICAL RESEARCH CONTINUUM
Basic Science
Research
Translation from Basic Science
to Human Studies
Attitudes to
Use/Validity of MBM
Translation Block
Variables
Personal psychological
factors, need for control
Education, Culture, and
Belief System
Personal transformational
experiences
Peer support, medical culture
Practice environment, time
demands
Patient expectation
Self efficacy, expectation of
positive outcome
Clinical Science and
Knowledge
Translation of New Knowledge Into Clinical
Practice and Health Decision Making
Clinical Trials of
MBM
Improved
Health
•Attitudes to Use/Validity of MBM
•Clinical Practice of MBM
Variables
Peer support, medical culture
Practice environment, time
demands
Patient expectation
Self efficacy, expectation of
positive outcome
•Referral to MBM Practitioners
Previous findings—Astin’s National Survey
• 1/3 of physicians acknowledged importance
of psychosocial issues but doubted
addressing them would make much
difference in health outcomes
• A minority believed they had effective
training in these areas or desired more
{Astin, et al. J Am Bd Fam Prac in press, 2006}
Barriers
•
•
•
•
Poor training
Lack of self-efficacy/control
Lack of knowledge of evidence base
Inadequate time/reimbursement
{Astin, et al. J Am Bd Fam Prac in press, 2006}
Mind Body Medicine methods explored in
current survey
•
•
•
•
•
•
Biofeedback
Guided imagery
Hypnosis
Meditation
Relaxation therapies
Yoga and Tai Chi
Not specifically inquired
about:
• Cognitive behavioral
therapy
• Psychoeducational
approaches
Gender Difference in the use of MBM
80
75.7
70
62.2
Percentage
60
50
40
32.4
30
20
10
13.5
10.8
5.4
0
Often
Sometimes
Variables
Male
Female
Never
Assessment of MBM Approaches
90
80
70
60
50
40
30
20
10
0
High Belief FM
High Belief PSY
Anxiety
Depression
MBM Approaches in Treating
Various Disorders
60
50
Irritable Bowel
Fibromyalgia
Hypertension
Low Back Pain
40
30
20
10
0
High FM
High PSY
Factors that Limit Physician's
Interest in Using MBM
80
60
Poor Training
40
Lack of expertise
20
FM Greatly
PSY Greatly
Contributes
Inadequate
Reimbursement
0
Absence of qualified
practitioners
Insufficient clinic time
Factors that Limit Physician's Interest
in Using MBM - Cont'd
60
50
Absence of demonstrably
effectiveness
40
Lack of acceptance among
peers
30
Resistance of patients
20
10
FM Greatly
PSY Greatly
Contributes
0
Concern that patients feel
being discounted
Summary of findings
• There was little difference between physicians’
responses in the two specialties
• Substantial reports that barriers to the use of MBM
were largely based on lack of training, inadequate
expertise, and insufficient clinic time
• Lack of expertise and insufficient clinic time were
higher among family physicians than psychiatrists
• There was a high interest in both groups in learning
relaxation techniques and meditation and lower interest
in biofeedback and hypnosis
Summary of Findings
• Female physicians significantly more likely to utilize
MBM in both their own self-care and with patients
• Female physicians less likely to be concerned that
recommending these therapies would make patients
feel that their symptoms were being discounted
• Female physicians also had significantly higher
beliefs about the benefits of MBM on health disorders
than males in several of the conditions examined, with
a consistent, though non-significant trend in others.
MBM/Stress Management Curriculum
• SNAPSHOT VIEW
The Relaxation Response
• A mental focusing device
• A passive attitude to distracting thoughts
• Deep, relaxed, abdominal breathing
{Benson H, Stuart E. The Wellness Book, 1992}
Steps to eliciting the
Relaxation Response
1. Focus word
2. Sit quietly in
comfortable position
3. Close your eyes
4. Relax muscles
5. Breath slowly,
naturally, repeat focus
word
6. Assume passive
attitude
7. Continue 10-20
minutes
8. Daily practice
9. When distracting
thoughts occur,
return to focus word,
breathing
Stress Survival Strategies for
Health Care Professionals and
Patients
Victor S. Sierpina, MD
Nicholson Professor of Integrative Medicine
Department of Family Medicine
UTMB
Some intrinsic stressors in
Medicine
Staffing
Scheduling
Time pressures
Diagnostic
challenges
Malpractice
Sleep deprivation
and shift work
PTSD
Role ambiguity
among residents
Depressed
immunity
Patient related stressors
Communication issues with patients and
their families, verbal abuse
Violence
Exposure to infection: hepatitis, AIDS,
SARS, MRSA, DRE, other “bug du jour”
Drug seekers
Social, financial problems of patients
What Can Be Done About
Stress?
Biological interventions
Psychological interventions
Social interventions
Personal/social stress resilience
approaches
Music listening and
music making
Self reflection
Spiritual well-being,
prayer, religious
practice
Massage
Essential oils
Cognitive
behavioral
strategies
Biofeedback
Humor
Mindfulness based
stress reduction
Psychodrama
Imagery
Relaxation therapies
Some Simple Techniques
Deep breathing
Progressive Muscle relaxation
Music
Meditation
Future studies
• National survey of FM and Psych Residency
Directors and Chief Residents (IRB review of
revised on-line survey in progress)
• Evaluation of impact of MBM training on FM and
Psych residents personal and professional
practices (proof of concept to follow pilot)
• Focus on how MBM training can help programs
attain competencies in Professionalism
Manuscripts produced
• Sierpina V, Levine R, Astin J, Tan A. Use of
Mind-Body Therapies in Psychiatry and
Family Medicine Faculty and Residents:
Attitudes, Barriers, and Gender Differences.
Explore: The Journal of Science and Healing
{under review—2006}
Manuscripts produced
• Sierpina V, Astin J, Giordano J. Behavioral
and Mind-Body Therapies for Migraine and
Tension Headaches. Am Fam Phys {under
review—2006}
• Astin JA, Soeken K, Sierpina VS, Clarridge
BR. Barriers to the integration of psychosocial
factors in medicine: Results of a national
survey of physicians. J Am Bd Fam Pract. {in
press-2006}
Reference manuscripts
• Astin JA, Goddard T, Forys K. Barriers to the
integration of mind-body medicine:
Perceptions of physicians, residents and
medical students. EXPLORE: The Journal of
Science and Healing. 2005;1 (4):278-283.
• Astin J. Mind-body medicine: State of the
science, implications for practice. J Am Bd Fam
Pract. 2003;16:131-147
Acknowledgement
Supported by grants from the National Institutes of
Health:
• Mind-Body Exploratory and Development Grant
#1 R21 AG023951-01 from National Institute of
Aging and Office of Biobehavioral and Social
Science Research (VSS)
• #R01 AT00869-04 from the National Center for
Complementary and Alternative Medicine (JA)
• CAM Education Grant #1 R25 AT00586-01 from
National Center for Complementary and
Alternative Medicine (VSS)