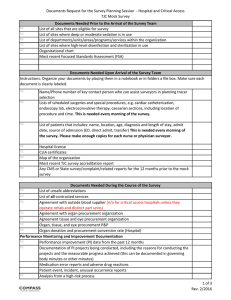
top 10 most frequently scored standards
advertisement

RISK ASSESSMENT Your friend on survey Kurt A. Patton President, Patton Healthcare Consulting, LLC RISK ASSESSMENT • You do it all the time in hospitals – Fall risk assessment – Suicide risk assessment – Hazard vulnerability assessment EM – Infection control risk assessment ICRA – ILSM evaluation – FMEA – EC rounds, quality audits, management rounds • All usually resulting in some change, intervention/mitigation strategy or redesigned process RISK ASSESSMENT • TJC Glossary: An assessment that examines a process in detail including sequencing of events; actual and potential risks; and failure or points of vulnerability; and that, through a logical process, prioritizes areas for improvement based on actual or potential impact(that is criticality) of care, treatment or services provided. 3 RISK ASSESSMENT, LESS FRIGHTENING DEFINITION • A formal, thoughtful evaluation of identified potential environmental hazards that demonstrates an assessment of the potential risk. This may validate your immediate impression that there really is no risk, or lead you to the conclusion that the risk is real and something should be done about it. 4 RISK ASSESSMENT AND A TJC SURVEY • Read the introduction to the LD chapter, somewhat intense • Read article from EC News May 2008, practical • Risk assessment and redesign can help you to do things better and more safely. • New concept for today: Risk assessment leading to no change, but validating your current process as safe and effective can be protective on a TJC survey. RISK ASSESSMENT EMBEDDED IN STANDARDS • • • • • • • EC.02.06.05 (ICRA) LD.04.04.03 (New process design) LD.04.04.05 (Patient safety program) NPSG.07.03.01 (MDRO) NPSG.07.05.01 (SSI) NPSG.07.06.01 (CAUTI) NPSG.15.01.01 (Suicide, patients and EOC) 6 RA HAS VALUE FOR TJC TOO • Surveyor subjectivity, surveyor opinion leading to findings and customer complaints is a dissatisfier • EP publication and A,B,C EP types was thought to prevent this subjectivity. • The principles of good process design was thought to help eliminate this subjectivity. • It was not enough REAL WORLD VALUE TO RA • Hospital complaint: The surveyor said this was dangerous, but we disagree and there is no standard that says we have to do it the way the surveyor suggested! We want this RFI removed! • TJC response: Did you do a risk assessment? – This gives them cover. They don’t have to conclude your process is risky, only that you failed to evaluate it as safe. TJC FINDINGS WHERE A RISK ASSESSMENT COULD HAVE HELPED • There are 3 entrances to this behavioral health clinic. • There are hazardous chemicals in the laundry room on behavioral health that could be harmful to patients. • The pneumatic tube delivery is into the hallway and that may lead to tampering of medications. VALUE OF RA • There are 3 entrances to this behavioral health clinic. – Its an outpatient clinic, not IDT, no SMI, no involuntary patients, no criminal offenders, no incidents in many years of incident analysis, patients use the patio for fresh air while waiting and entries are near parking lots. • TJC response: Did you do an RA? VALUE OF RA • There are hazardous chemicals in the laundry room on behavioral health. – The door is always locked. Patients are not permitted in the laundry room unless supervised by staff. Patients who are on suicide watch, 1:1, or close observation are not granted privileges to use the laundry room. • TJC response: Did you document an RA with this mitigation strategy? VALUE OF RA • The pneumatic tube delivery is into the hallway and that may lead to tampering of medications. – The delivery point is less than 10 feet from the nursing station. The tube makes a racket when a delivery arrives. Staff are in the hallway and will see and hear the delivery. • TJC response: Did you document a RA? Value of a Risk Assessment, cont. • A completed risk assessment that is presented to the survey team can be a point of protection during a survey or post survey clarification. • It means that your staff and leaders identified this as an issue, analyzed it, document that analysis and determined an appropriate course of action based on the risks…. HOW DO WE IDENTIFY THE POTENTIAL RISKS? • Think like a stranger seeing your units for the first time. • Set a very low threshold to identifying potential risk. • Think of risk assessment as your insurance policy to not be second guessed for decisions. • Risk assessment is not a tedious task, think of it as your best friend and protector. THINK OF RA THIS WAY 15 WHO CAN IDENTIFY THESE POTENTIAL RISKS FOR US? • Managers or department heads in their own areas if they can look with fresh eyes. • Cross departmental manager visits • Quality department staff, or the person who everyone else thinks is too cautious or nervous. • External mock surveyors When do you do a Risk Assessment? • Anytime you identify something that could potentially cause harm or have a negative effect on patient outcome • If you think something may be ok, but a hyper-vigilant surveyor may not… validate your processes are safe • Can be clinical or non-clinical DON’T BE FRIGHTENED BY THE TERM RISK ASSESSMENT • It does not have to be as thorough as your FMEA • It does not have to be labor intensive • You don’t need to schedule 6 months of meetings • You don’t need minutes of meetings • You do need to document your RA though. Sample Risk Assessment Tool is not Complex • This risk assessment tool is not a – Infection Control Risk Assessment – Hazard Vulnerability Analysis – FMEA Failure Modes and Effects Analysis assessment • It is a simple tool that can be used by staff – – – – To proactively identify things that could cause harm Assess the likelihood they will result in a negative outcome Assess the likelihood that the harm will be significant If necessary, implement an action plan – safeguards to prevent 20 Risk Assessment Step 1: • Identify the potential hazard and who might be harmed • Consider the situation from different view points using multidisciplinary approach – – – – What if it was night shift What if a small child was wandering and came across this What if the agency staff were unaware of our workaround What if, what if what if…. Risk Assessment Step 1a: cont. • A possible outcome is that your hospitals gets dinged by TJC so include the potential standard violation and the risk level associated with that standard issue: – – – – Situational Decision Rule (2) Direct Impact (3) Indirect Impact Scoring Category (A or C) • Can include: – – – – Data from incident reports Data from infection control Sentinel event alerts Literature search on best practice Risk Assessment Step 2: • Describe the safeguards already in place to prevent the potential harm • This can include: – – – – – – – – Structure – process – outcome What structures prevent harm? Possible training or staff education done to prevent harm? What processes or policies prevent harm from happening? Visual observation of the area/situation ongoing Data from incident reports Data from infection control Literature search to support your process Risk Assessment Step 3: • Assess the level of risk posed by the potential hazard and decide if the measures currently in place are adequate to prevent harm or should more be done… • Assess the risk on two scales: – Likelihood – assess the likelihood of harm occurring from the potential hazard – Severity – assess the possible severity of the outcome if the negative event occurred. • Place an “X” in the box corresponding with your score SLIGHTLY MORE COMPLEX USING 3 AXIS OR FACTORS • Likelihood/probability • Severity • Preparation or mitigation strategy – Always use this 3 axis technique for suicide hazards • Can add to complexity with 4 outcomes, using extreme above high Risk Assessment Step 3: cont • If the box checked is “low”, then submit to your safety manger, obtain their signature under “reviewed by” and date. Keep copy in your department, send copy to hospital quality. – You are done for now – Consider redoing the assessment at some point because conditions change and acceptance thresholds change • If the box checked in step 3 is medium or high risk, DO SOMETHING, complete an action plan Risk Assessment Step 4: The Action Plan • Implement an action plan when you decide we have to do something. • The goal is to reduce the chance of risk by implementing safeguards • What action is needed, what time frame, communication plan • Track completion, record and save • Reassess after the intervention The Action Plan MITIGATION STRATEGY • Not an action plan, but a strategy that is already in place that protects our patients from harm. • Always identify the mitigation strategy for suicide hazards. – Staffing, clinical screening, precautions, reassignment of high risk patients to another room. SPECIALIZED RISK ASSESSMENTS • Suicide hazards per NSPG.15.01.01 – EP 1: “Conduct a risk assessment that identifies specific patient characteristics and environmental features that may increase or decrease the risk for suicide. • EC.02.01.01 – EP 1: “The hospital identifies safety and security risks associated with the environment”. • Eye wash necessity is one example of this type or RA 31 IDENTIFYING SUICIDE HAZARDS • Look for and identify environmental features that could allow an unsupervised patient to injure themselves or others. • Use a very low threshold for potential risk • Use potential risks such as identified by NAPHS • https://www.naphs.org/Design%20Guide%205_1_FI NAL_051412.pdf • VA and ECRI also have tools that can help you identify potential suicide hazards. 32 IDENTIFYING SUICIDE HAZARDS • Don’t forget to include those parts of the ED which serve behavioral health patients, including the bathrooms they will use. 33 WHAT DO WE DO AFTER IDENTIFYING ALL THE POTENTIAL HAZARDS? • 1. Spend several million dollars to fix them all this immediately. • 2. Develop a multiyear plan to get them all fixed. • 3. Evaluate the degree of risk for each potential hazard and fix the most significant problems and develop a thoughtful mitigation strategy for those that cannot be immediately corrected. 34 WHAT IS A MITIGATION STRATEGY? • Create some safer rooms, clinically screen patients and: – Prioritize placement – Place on 1:1 supervision – Allow entry to some areas only when supervised 35 DOCUMENTING THE RISK ASSESSMENT • Can use the PHC tool and multiply: – Probability of use 1-3 – Outcome if used 1-3 – Detectability 1-3 • Worst possible outcome is 9, for immediate correction • Detectability: The most problematic because supervision may be inadequate. – Less easy to see inside the patients room, less still to see inside the patients bathroom. Make the less detectable areas safer first. 36 37 EYE WASH RISK ASSESSMENTS • Lots of scoring for failure to have an eyewash the past 2 years. • Plumbed eyewash requires weekly testing and annual inspection. • OSHA would mandate if you use corrosive chemicals. No choice or decision • Many chemicals used that are irritating to the eye. 38 EYE WASH RISK ASSESSMENTS • Non corrosive, but irritating chemicals can be evaluated using the risk assessment tool. – – – – – Evaluate the relative risk, for example pouring from one container to another, vs using a wipe that contains the chemical. High risk gets 3 points, low risk gets 1 point. Evaluate the relative risk based on hospital experience, your incident reporting system and the professional literature. Assign 3 points if you have reports and the literature reports this being a problem, assign 2 points if you have never experienced a problem and there is only one or very few reports in the literature. Assign 1 point if you have never experienced a problem and there are no reports in the literature. Evaluate the inherent staff mitigating factors such as staff always wearing PPE and eye protection. Assign 1 point if PPE and eye protection is available and staff routinely where it. Assign 2 points if eye protection is not available or not used. Evaluate staff preparation, or ability of staff to assist each other. If there is a splash, can staff guide, aid their coworker to a plumbed eyewash? Assign 1 point if there are always staff to assist, and 2 points if the worker is alone in this area. Evaluate how long it would take to get to a plumbed eyewash if needed. Assign 3 points if longer than 30 seconds, 1 point if less than 10 seconds, 2 points between 10 and 30 seconds. 39 MOST IMPORTANT TAKE AWAY • Risk assessment is not to be feared • Risk assessment is your insurance policy against being second guessed for failure to consider an issue. • Learn to do it early and often • Make sure multiple leaders have copies and awareness of the risk assessment. 40 Questions? Kurt@PattonHC.com