Medication Teaching
advertisement
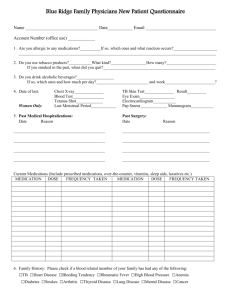
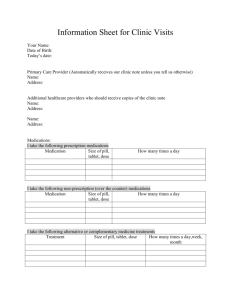
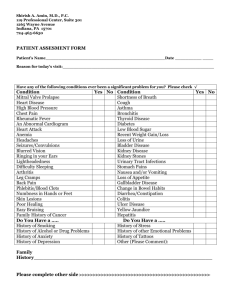
Medication Teaching What Parents Should Know Nadya Nalli, BSc.Phm Paediatric Academic Multi Organ Transplant Pharmacist The Hospital for Sick Children Pharmaceutical Care Pharmacist • Accepts that he/she will be directly responsible to the patient Patient • becomes a partner in care rather than recipient of care Paediatric Practice Spectrum • Neonate adolescent Patient & parent/caregiver dynamics Medication teaching Who Why When What How = = = = = audience purpose urgency content media WHO? / Audience Adult vs child • Learning capacity Age variant • Style Several theories (adult and child) Operational stages (Piaget) Learning Style Inventory Audience • Experience/perspective Acute vs chronic illness Cultural differences • Language fluency Audience Terminology • common vs medical • definition of terms • acronyms/short forms • familiarity with system Why? / Purpose Although essential in disease management, if taken improperly, medications can also be the source of significant morbidity and mortality Major underlying causes of patient adverse drug events have been associated with defects in drug knowledge dissemination Purpose Non-compliance and drug misadventure are more likely to occur when patients are prescribed many medications Drug misadventure is more likely when patient medication regimens are changed. One should not consider possible risks associated with taking particular medicines in isolation from the likely beneficial effects. For most people there will be only a single benefit that is sought, but the potential risks are often multiple. Purpose Pharmaceutical Care has been the pharmacist’s approach to improving medication use Pharmaceutical care is the responsible provision of drug therapy designed to meet a defined outcome individualized for a specific patient. When? / Urgency Stress is a barrier to learning Prioritize information Flexibility Follow-up What? / Content Reason for use • goals of therapy • time frame of effect Schedule • dose time; potential for flexibility • drug-drug, drug-food, drug-disease issues Content Potential/expected adverse effects • monitoring at home • urgency Management of adverse effects • plan Content Dose Administration • route (po/pr/ng,gt,jt/topical/sc/iv) • dose form manipulation • strategies • problem solving skills Content Drug coverage • ODB (Trillium/HCP/WF) or private plan • OOP (out of province) patients • fiscal year/family cap • co-pay • Rx vs OTC • paperwork (LUF vs. sect 8 approval) Media Verbal summary Verbal + written summaries Innovative material • Colour coding • Braille Medication schedule Teaching & Self Medications 6A/4D Background • Paediatric Academic Multi-organ Transplant • 40+ transplants/year (heart, lung, liver, kidney and small bowel) • single or combined • Deceased donor or living related* • full organ or split* Teaching & Self Medications 6A/4D Philosophy: • learning occurs in an environment where safeguards and resources are available in order to optimize care • family-centred care • multi-disciplinary approach Teaching & Self Medications 6A/4D Consent • discuss goals of program with caregiver(s) and or patient (if age appropriate) • obtain written consent; place in chart • set a time that is mutually convenient • determine need for interpreter Teaching & Self Medications 6A/4D Teaching • initially didactic (~ 1 hour) • progression to didactic/interactive • limit setting by caregiver re: amount of information given per session • follow-up sessions as required • documentation! Teaching & Self Medications 6A/4D Medication Summary • individualized • includes standard oral/iv medications • includes name(s), reason for use, adverse effects and special instructions Case 7 yr old male; 2 weeks post renal tx • • • • • • • • • Tacrolimus 3mg po q12h Mycophenolate mofetil 250mg po q12h Prednisolone 5mg po daily Trimethoprim sulfamethoxazole 60mg po q daily Nystatin 100,000u swish/swallow qid Ganciclovir 150mg iv daily Magnesium hydroxide 400mg++ po bid Phosphate sodium 15mmol po bid Ranitidine 75mg po qhs Medication Summary for Transplant Patient, July 2004 Name of Drug What is it For? Side Effects Special Instructions - take dose on time Tacrolimus (FK) (Prograf) - to prevent rejection - tremors - may blood pressure - may magnesium levels - may potassium levels - kidney damage (dependent on level) - take with food or juice (no grapefruit juice) or on an empty stomach, but always take it the same way. - if vomit dose in: <1/2hr: take again 1/2-1hr: take 1/2 amount > 1hr: do not need to re-take *Repeat dose only once* - if diarrhea tell transplant nurse - seizure (dependent on level) - may cause hair loss - check with the transplant nurse first before starting any new medicine - 0.5mg, 1mg, 5mg capsules, also 0.5mg/ml HSC suspension that is stored at room temperature and must be shaken before each dose - FK blood levels are measured in the morning before your morning dose Teaching & Self Medications 6A/4D Accommodation of Preferences • dose form (solid vs liquid) • dose form (size vs volume) • dose schedule (where applicable) Teaching & Self Medications 6A/4D Medication Administration Record (MAR) • individualized • double checked • updated every shift • adaptable, where possible Medication Schedule for Transplant Patient Time Medication 8am Tacrolimus (FK) Mo Tue We Thu Fri Sat Sun (0.5mg/ml susp’) Mycophenolate mofetil (MMF) (100mg/ml susp’n) Prednisolone (1mg/ml liquid) Cotrimoxazole (8mg TMP/ml susp) Nystatin (100,000u/ml susp) 11am Magnesium hydroxide (33mg++/ml susp) XXX XXX XXX XXX Teaching & Self Medications 6A/4D Medications • individualized • 7 day supply • provided in lock box (room temp meds) • template for optimal storage Teaching & Self Medications 6A/4D Drug Plan • determine type & extent of drug coverage • if private, give DINS to parents • if ODB, identify limited use vs sect. 8 vs full • if OOP patient, identify all potential payors Teaching & Self Medications 6A/4D Drug Plan • explore compassionate supply avenues • referral to Trillium if required (Ontario patients only) • liaise with social worker (if required) and discharge planner Teaching & Self Medications 6A/4D Life Issues • concomitant/new medications • alcohol/recreational drug use • sexual activity • travel Teaching & Self Medications 6A/4D Discharge Prescription - continuity of care • ensure appropriate drug/dose • ensure optimizations/preferences included • communicate with outpatient pharmacy to ensure medication supply, convey information (patient/caregiver consent)