Update on Food Allergies: 2010
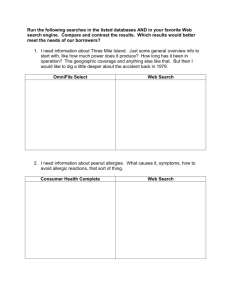
advertisement

Update on Food Allergies: 2011 William Parker, MD Head, Division of Allergy and Immunology Dayton Children’s Objectives Definitions and statistics Know the current recommendations regarding immunizations in children with egg allergy Food allergies in the school setting Be familiar with the latest information regarding prevention and treatment of food allergy Key issues in the latest practice parameters for management of food allergy Food-induced allergic disorders IgE dependent Disorder Key features Typical age Common foods Natural course Urticaria and angioedema Ingestion/skin contact, acute 20%, chronic 2% Children > adults Primarily major allergens Depends on food Oral allergy syndrome Pruritus, mild edema of oral cavity Adults/older children>young Raw fruits and vegetables, cooked tolerated Varied, may fluctuate with pollen season Rhinitis and asthma Rarely isolated or sole symptom unless inhaled Infant /child > adult unless occupational Major allergens ; Depends on food wheat, egg and seafood occupation Anaphylaxis Rapidly progressive, multiple organ systems Any Any but peanut, tree nuts, shrimp fish, milk, egg Depends on food Food-associated exercise-induced anaphylaxis Triggered only if food followed by exercise Older children and adults Wheat, shellfish and celery most described Presumed persistent Food-induced allergic disorders IgE associated/cell-mediated Disorder Key features Pathology Typical age Common foods Natural course Atopic Dermatitis Associated with food in 35% of children with moderate to severe rash Might relate to homing of foodresponsive T cells to the skin Infant > child > adult Major allergens, especially egg and milk Typically resolves Eosinophilic esophagitis, enteropathy Symptoms vary with site/degree of eosinophilic inflammation Esophageal: dysphagia and pain Eotaxin and IL-5 Any Multiple Likely persistent Food-induced allergic disorders Cell-mediated Disorder Key features Pathology Typical age Common foods Natural course Dietary protein enterocolitis Chronic : emesis, diarrhea, poor growth, lethargy Re-exposure: emesis, diarrhea, hypotension (15%) 2 hrs later Increased TNF-alpha response, decreased response to TGF-beta Infants Milk, soy, rice, oat, wheat Usually resolves Dietary protein proctitis Mucus-laden, bloody stools Eosinophilic inflammation Infants Milk, including through breast feeding Usually resolves Average hospital discharges per year of children with any diagnosis related to food allergy 10000 9000 8000 7000 6000 5000 4000 3000 2000 1000 0 1998-2000 2001-2003 2004-2006 Diagnosing food allergy History What symptoms Quantity and how prepared Time between ingestion and symptoms Similar instances or tolerance in past Other factors necessary (e.g., exercise) How long since the last reaction What food A few foods account for about 90% of reactions Prevalence of Food Allergy Food Milk Egg Peanut Tree nuts Wheat/soy Fish Shellfish Sesame Overall infant/child 2.5% 1.5% 1% 0.5% 0.4% 0.1% 0.1% 0.1% 5% adult 0.3% 0.2% 0.6% 0.6% 0.3% 0.4% 2% 0.1% 3% to 4% Food allergens-Cow’s milk Most common food allergy in young children Casein fraction 80% of proteins Whey fraction 20% Lactoglobulins, bovine Ig’s and albumin Casein proteins are most immunogenic Lactoglobulins and BSA in whey also important >90% will react to goat/sheep milk About 10% react to beef Food allergens-chicken egg Most common IgE-mediated food allergy Egg white contains 23 different proteins ovomucoid, ovalbumin, ovotransferin Ovomucoid is responsible for most reactions and has a unique structure 70% of egg allergic children can tolerate extensively heated/baked products Bread, cakes, cookies Vaccines in egg-allergic children Vaccine ACIP Red Book PI MMR/MMRV May be used May be used Use with caution, cites AAP Influenza Consult a physician Contraindicated Contraindicated Rabies Use with caution No recommendation Use with caution Yellow fever Contraindicated Contraindicated Protocols given Vaccines in egg-allergic children FluMist has a very low ovalbumin content No pediatric data and effect of respiratory route unclear Fluarix and Fluvirin have low ovalbumin content No data on FluLaval or Agriflu Affluria very low Not indicated below age 9 Fluzone has the highest Only product approved for ages 6-23 months Amount still relatively low Vaccines in egg-allergic children Skin testing not universally recognized as helpful Prospective and retrospective studies-reactions rare Rabies vaccine Imovax not made in chick embryro 2-dose approach becoming popular 10% of dose followed by 30 minute observation, then 90% Recent EP recommendation stated ‘insufficient evidence’ to make broad recommendations, but felt that current ACIP, AAP Red Book, and PI recommendations ‘may be too conservative’ How should you vaccinate the eggallergic child? Skip the immunization Use the 2 dose method Give 10% of dose Wait 30 minutes, give the remainder of vaccine Use the same brand product for booster if possible Same lot is not necessary You should be prepared for anaphylaxis – unlikley • Or Refer to an allergist Food allergens-peanut Which of the following foods should be avoided by patients allergic to peanut? a. Mike-Sells potato chips b. Penn Station french fries c. Chick-fil-A products d. all of the above e. none of the above Food allergens-peanut Most common pediatric food allergy above age 4 Peanut butter patented in 1865, hydrogenated oils added in 1922, first brand – Skippy At room temp has no vapor phase containing protein Refined/commercial peanut oil safe, pressed oils retain some allergenicity Cross-reactivity to other beans – 5% Food AllergensTree nuts Walnuts 34% Cashew 20% Almond 15% Pecan 9% Pistachio 7% Hazelnut Brazil nut <5% Pine nut Macademia nut Cross-reactivity 35% higher for cashew-pistachio almond-hazel, walnut-pecan Food allergens-shellfish 2% or more of adult population Crustacea-lobster, crab, shrimp, crawfish Extensive cross-reactivity within group, little to mollusks or radiocontrast media Mollusks-oysters, scallops, clams, squid, snails, mussels Raw vs cooked makes little difference Food allergens-fish Several hundred species in class Osteichthyes Extensive cross reactivity on testing, modest but clinically relevant on challenges Most patients allergic to fresh cooked tuna or salmon can tolerate canned product Reactions to airborne allergen emitted during cooking not uncommon Food allergens-wheat Several important proteins Globulins and glutenins in IgE mediated disease Gliadins in celiac disease Albumin in Baker’s asthma Extensive cross reactivity between wheat, rye, and barley on testing, 20% on challenges Similarities to grass proteins may account for clinically irrelevant positive tests to wheat and other grains Diagnosing food allergy Skin prick testing (SPT) Positive tests suggest, negative tests essentially confirm (>90% NPV) Increasing SPT wheal size is correlated with increasing likelihood of allergy, not severity Testing with fresh food preparation helpful for fruits and vegetables Diagnosing food allergies Food-specific IgE antibodies Several available assays Increasingly higher values correlate with likelihood of reaction but not severity Exceedingly high values at diagnosis may reflect poor prognosis for outgrowing allergy Mean level for 5 yo at which 50% react (kUa/L) Milk 2 Egg 2 Peanut 5 Diagnosing food allergies Food-specific IgE antibodies Positive Predictive Values Negative Predictive Value Food kUa/L PPV kUa/L NPV Egg infants<2 7 2 95% 90% .6 90% Milk infants<1 15 5 95% 95% .8 1.0 95% 90% Peanut 14 99% .35 85% Fish 20 99% .9 95% Soy 30 73% 2 95% Wheat 26 74% 5 95% A 5 year old child presents with atopic dermatitis for evaluation of food allergy. Results of the diagnostic evaluation are listed below. Which of the following foods would be most likely to induce a clinical reaction on a DBPCFC? egg milk soy wheat Prick skin test wheal 8mm 3mm 5mm 10mm Specific IgE kU/L 7 0.35 5 15 Treatment options Natural history 80% of milk allergic children and 66% of egg allergic children are tolerant by age 5 30% of wheat allergy outgrown by age 4, 60% by age 8 25% of soy allergy gone by age 4, 45% by 6, 69% by 10 Only 20% of peanut allergic children become tolerant Recurrence of allergy after tolerance reached is rare 4% of patients who do not eat peanuts regularly suffer recurrence Treatment options Active therapy Standard subcutaneous immunotherapy Modified protein vaccine Anti-IgE antibodies Probiotics, Chinese herbal FAHF-2 Oral immunotherapy Promising studies in milk, egg, and peanut Some epi doses required in all studies Desensitization but not tolerance, continued regular ingestion of food required Effects of Infant Feeding on Development of Atopic disease In high-risk infants, exclusive breast-feeding for 4 months has been shown to decrease the risk of: A) asthma B) atopic dermatitis C) food allergies D) all of the above E) none of the above Effect of Introduction of Solid Foods Past AAP recommendations were to delay: Solid foods until 4-6 mos cow’s milk until 12 mos In at risk infants delay egg until age 2 and peanuts, tree nuts and fish until age 3 More recent prospective studies are conflicting, raising “serious questions about the benefit of delaying solid foods” past 4-6 mos, including highly allergenic foods Is Early Introduction of Peanut Protective? Jewish children ages 4-19 living in London and Tel Aviv; 10,786 questionnaires/82% returned Questionnaires completed by high school students and parents of primary school age pt Questionnaire positive pts confirmed with skin tests or specific IgE (>95% + predictive value) or oral challenge Mothers questioned about solid food consumption during the first year of life Is Early Peanut Protective? Prevalence of peanut allergy in UK was 1.85% and in Israel was 0.17% (P<.001) Age of introduction of egg, soy, wheat, and tree nuts similar between the 2 groups By 9 mos 69% of Israelis were eating peanut compared to 10% in UK Median monthly consumption in infants 8-14 mos was 7.1 g in Israel vs 0 g in UK (P<.001) Consumption 8 times monthly, mostly peanut butter Rate of peanut allergy was 10 times higher in UK children vs Israeli children and was not explained by differences in gender, rate of atopy, or socioeconomic status Du Toit G, et al J Allerg Clin Immunol. 2008; 122:984-991 Is Early Egg Protective? 2,589 Australian infants enrolled, age 11-15 months Egg allergy confirmed in 231 children Later introduction of egg associated with increased risk Compared to infants eating eggs at 4-6 months Odds ratio 1.6 for introduction at 10-12 months Odds ratio 3.4 for introduction after 12 months Duration of breastfeeding had no effect How early is too early? 503 infants being evaluated for suspected milk or egg allergy 301 infants with history of immediate reaction 202 infants with mod-severe AD and positive test Peanut sIgE of 5 or higher in 28% of patients Peanut consumption during pregnancy associated with a 3fold higher risk of sensitization Highest odds ratio of 4.99 in subgroup of 71 infants never breastfed Maternal diet during pregnancy Previous AAP recommendations Lactating mothers of high risk infants should avoid peanut and nuts and consider eliminating milk, eggs, and fish 2003 study – no effect of peanut intake 2006 Cochrane review – no effect of maternal exclusion diet Current AAP recommendations Lack of evidence that maternal dietary restrictions during pregnancy or lactation play a significant role Recent EP agrees…”does not recommend restricting maternal diet during pregnancy or lactation as a strategy for preventing the development or clinical course of food allergy” LEAP study Learning Early About Peanut Allergy 500 children enrolled between 4-8 months of age History of egg allergy and/or atopic dermatitis No personal or family history of peanut allergy Randomized to intervention group fed peanut 3 times a week or control group Skin and blood tests at 1, 2.5, and 5 years Oral challenge at 5 years of age Food Allergies in School “Fear and Allergies in the Lunchroom”, 5 Nov 2007 What’s a parent to do? Peanut-free schools? Food allergy tables? How many Epi-Pens or Twinjects? Where are they kept? When are they used? Skin contact? Airborne exposure? Deaths in the U.S. in 2005 (all ages) Food allergies Lightning strikes Insect stings Malnutrition Accidental drowning Accidental poisoning Flu and pneumonia 18 48 82 3,003 3,976 23,618 63,001 Sources: National Center for Health Statistics, Centers for Disease Control and Prevention Management of Food Allergies in Schools A patient in which of the following age groups is at greatest risk of food-induced fatal anaphylaxis? a) preschool students b) elementary school students c) high school students Parents and food labels 91 parents of children reviewed 23 product labels, asked to name the food allergen present in the food product 7% (4 of 60) identified all 14 products containing milk 22% (6 of 17) identified all 7 products containing soy 54% (44 of 82) identified all 5 containing peanut Results were better for egg and wheat Food labeling for allergens Food Allergen Labeling and Consumer Protection Act Passed in 2004 8 major food allergens Milk, egg, peanut, tree nuts, soy, wheat, fish, crustacean shellfish Highly refined oils and their derivatives are exempted Does not regulate voluntary disclaimers ‘may contain traces of….”, “made in the same factory as…..” 20,241 manufactured food products-17% contained warning 100 products with voluntary labeling regarding milk 34 had detectable milk residues o 61% -”may contain” o 33% - “shared equipment” or “shared facility” Food Allergies in School Where do the majority of school-related anaphylactic food reactions occur? a) cafeteria b) school bus c) classroom d) gym class Self-administered epinephrine Two commercially available devices 33-66 lbs – 0.15 mg >66 lbs – 0.3 mg Kept on person vs in classroom vs in office ? When to use ? Hx asthma or prior episode? 19% of food-induced episodes used 2nd dose 25% of episodes occur without prior diagnosis Peanut Butter at school 30 school-aged children with peanut allergy DBPC inhalation challenge for 10 minutes No objective sx, one subjective SOB DBPC patch testing No systemic reactions, 40% mild local rash Various hand cleaning methods all effective except alcohol-based hand sanitizers Summary Statements For high risk infants, exclusive breastfeeding for 4 months vs milk formula decreases atopic dermatitis and milk allergy in first 2 years Infants with moderate to severe atopic dermatitis have a 3040% incidence of food allergy Exclusive breastfeeding for 3 months protects against wheezing in early life, but not against allergic asthma occurring beyond age 6 Summary Statements No convincing evidence for use of soy-based formula for allergy prevention In high risk infants who are not exclusively breastfed for 4-6 months or are formula fed there is modest evidence that atopic dermatitis may be delayed or prevented by use of hydrolyzed formulas Extensively hydrolyzed more effective Higher cost should be considered No studies on use of amino acid-based formulas No current convincing evidence that delaying solid food beyond 4- 6 month of age is protective for allergic disease Including highly allergenic foods like fish, egg, and peanut Food Allergy Update-2011 Food allergies affect 5% of children A few foods account for >90% of reactions Accurate diagnosis includes history and careful interpretation of in vivo and in vitro testing Encouraging studies regarding oral desensitization for milk and peanut No significant evidence-based support for many current infant feeding and school management practices Questions? References Young MC, Munoz-Furlong A, Sicherer S. Management of food allergies in schools: A perspective for allergists. J Allergy Clin Immunol 2009; 124:175182 Greer FR, Sicherer SH, Burks AW, et al. Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Timing of Introduction of Complementary Foods, and Hydrolyzed Formulas. Pediatrics 2008; 121 (1):183-190 Park A. Going Nuts Over Nut Allergies. Newsweek 9 March 2009:p 41-45 Sicherer SH and Sampson HA. Food Allergy. J Allergy Clin Immunol 2009; 125:1-10 Expert Panel. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel. J Allergy Clin Immunol Dec 2010; 126:S5-S56 Early feeding practices High-risk infants – 1 first-degree relative Partially hydrolyzed whey Good Start Supreme Partially hydrolyzed whey/casein Enfamil Gentlease Extensively hydrolyzed casein Nutramigen, Alimentum, Pregestimil Free amino acid-based Neocate, EleCare GINI Study Conclusions Incidence of AD at 1 yr in exclusive breastfed, breast plus EH formula, breast plus CM was 9.5%, 9.8%, and 14.8% At 3 yrs incidence was 6%, 6%, and 12% PH-whey more effective than EH-whey, neither as effective as EH-casein Breast or breast plus EH formula reduce but do not prevent majority of cases of AD No effect on incidence of asthma German Infant Nutrition Intervention Study 2252 high risk infants enrolled by day 14 Randomly assigned to supplements of one of 3 hydrolyzed formulas or cow’s milk formula 889 infants exclusively breastfed for 4 months 945 introduced randomly to one of above No solids before 6 mos of age 418 noncompliant or drop-outs, highest in the extensively hydrolyzed casein group Von Berg et al, J Allerg Clin Immunol 2003; 111: 533-540 Breastfeeding and prevention of Atopic Dermatitis 2001 meta-analysis of 18 prospective studies Over 4000 children followed for 1-5 yrs (4.5) Exclusive breastfeeding for 3 months protected against development of AD Cohort as a whole (OR : 0.68) Infants with family history of allergy (OR : 0.58) No effect on infants with no family history of allergy Breastfeeding and Asthma Meta-analysis in 2001 found exclusive breastfeeding was protective Strongest with family history of atopy (OR 0.52) Cochrane review in 2002 found no effect More recent study distinguished between infant viral-induced wheezing from asthma in older children with allergies and PFT changes Increased risk of asthma at age 13 if breastfed Decreased of recurrent wheezing of infancy