PowerPoint
advertisement

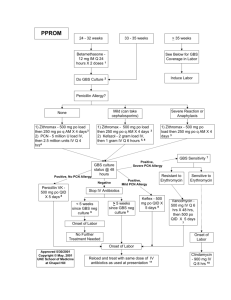
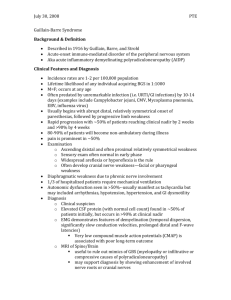
الجامعة االسالمية-غزة. كلية علوم الصحة قسم العلوم الطبية املخبرية وبالتعاون مع مؤسسة أطباء بال حدود. ضمن مشروع التعلم الخدمي ()Service learning اشراف الدكتور: عبد الرؤوف املناعمة (GBS) BACTERIA :GROUP B STREPTOCOCCI INTRODUCTION • GBS Bacteria is the leading infectious cause of early neonatal morbidity and mortality in the United States. • Initial case series reported case-fatality ratios as high as 50%. STREPTOCOCCUS AGALACTIA GROUP B , BETA- HEMOLYTIC STREPTOCOCCI: • General characteristics :. • Gram positive • Hemolysis on Sheep Blood Agar is mostly beta hemolysis. • Catalase negative • The group antigen is a cell wall polysaccharide composed of N_acetylglucoseamine, galactos, and rhamanose. GBS Hemolytic • It hydrolysis hippurate to benzoic acid and glycine. • It is resistant to bacitracin antibiotic disk (and could be differentiated from S. pyogens which is a beta _hemolytic and sensitive to this antibiotic). STREPTOCOCCUS AGALACTIA: Habitat: It is a part of the normal oral and vaginal flora . Approximately 5-15% of healthy population carry S. agalactia in the nasopharynx. It can be found in pharynx and gastrointestinal tract. It could be present in a various site in the newborn and this the most important. ACQUISITION OF GBS DURING BIRTH PATHOGENICITY: 1. Puerperal sepsis. 2. Endocarditis. 3. Neonatal infection (Pneumonia, septicemia and meningitis. 4. Bovine mastitis. Mortality rate 5-10%, Inversely proportional to birth weight. SPECIMEN COLLECTION • Swabbing both the lower vagina and rectum (through the anal sphincter) increases the culture yield substantially compared with sampling the cervix or the vagina without also swabbing the rectum . • GBS isolated can remain viable in transport media for several days at room temperature however, the recovery of isolates declines during 1–4 days, particularly at high temperatures. • Even when appropriate transport media are used, the sensitivity of culture is greatest when the specimen is stored at 4°C before culture and processed within24 hours of collection. CULTURE OF THE ORGANISM : • 1. On general media : e.g. :,Blood Agar S. agalactiae produces larger colonies and more translucent to opaque colonies surrounded by a zone of beta _hemolysis. • 2. Selective media(streptococcal Selective Agar(SSA)which contains the following inhibitory chemicals: • Crystal violet in low concentration, • Colistin , • Trimethoprim _sulphamethoxazole • in 5% sheep blood agar. CATALASE GBS – catalase negative HIPPURATE HYDROLYSIS TEST: • Group B streptococci contain enzyme hippuricase which can hydrolyze hippuric acid. • The products of the hydrolysis of sodium hippurate are sodium benzoate and glycine . • Glycine could be detected by the addition of ninhydrin which is an oxidizing agent which also gives a purple color with glycine. Purple color is positive for hippurate hydrolysis CAMP TEST: • The hemolytic activity of staphylococcal beta lysine on RBCs increased by an extracellular factor produced by S.agalactia called the CAMP factor. • This test is don by making a single streak of streptococcus on sheep blood agar perpendicular to a strain of staphylococcus aurous known to produce betalysine . • The positive result is expressed by a zone of increased lysis assuming the shape of an arrow head at the junction of the two streak lines. CAMP Test Positive zone of enhanced hemolytic activity (GBS) BILE ESCULIN: • This test detect the ability of the organism to grow in the presence of bile and its ability to hydrolyze esculin and the production of glucose production of and galactos esculetin. • Esculetin reacts with iron salts to for a dark brown or black complex. • This test is performed in an appropriate medium containing bile, esculine, ferric citrate as a source of ferric ions, and sodium azide to inhibit the growth of gram negative bacteria. • This test used to differentiate group D streptococci (positive), and Streptococcus (negative) LATEX AGGLUTINATION; • Antibody coated latex particles serves as the basis for several commercially available systems for direct detection of bacterial and other microbial antigens in body fluids . • Latex agglutination tests are also available to detect antibodies that develop during certain bacterial infection. • The advantages of agglutination test is rapidity and its relative sensitivity. LATEX AGGLUTINATION TEST: Positive agglutination is present Negative agglutination GBS GBS is not present Identification Tests from Enrichment Broth • Direct testing for GBS from broth can occur AFTER incubation in enrichment broth • The following methods are supported for direct testing of the enrichment broth: – DNA probe – Latex agglutination test – Nucleic acid amplification testing (NAAT) Antimicrobial Susceptibility Testing Antimicrobial Susceptibility Testing Standard: Penicillin (PCN) or ampicillin Alternatives: • PCN-allergic and low risk for anaphylaxis: cefazolin • PCN-allergic but high risk for anaphylaxis depends on susceptibility to clindamycin & erythromycin – If susceptible to clindamycin (including lack of inducible resistance) clindamycin – If unknown or not susceptible vancomycin Susceptibility of GBS: • All susceptible to penicillin, ampicillin, cefotaxime, and vancomycin, however: – Erythromycin resistance: 46% – Clindamycin resistance: 24% Clindamycin & Erythromycin Resistance among GBS isolates, 2000-2008 Isolates are from CO, GA, MD, MN, NY, and OR. 2007 data excluded Antimicrobial Susceptibility Testing • CLSI recommends using either: – Disk diffusion – Broth micro dilution • FDA-cleared/approved commercial system may also be used – Testing for inducible clindamycin resistance • D-zone or other validated test Antimicrobial Susceptibility: Etest & Disk Diffusion Zone of inhibition of growth for clindamycin is ≥19 mm (susceptible Erythromycin MIC = 0.19µg/ml Etest Disk Diffusion Zone of inhibition of growth for erythromycin is ≥21 mm (susceptible Procedure for D-zone Testing to Detect Inducible Clindamycin Resistance • Use swab to make suspension from 18-24 hr. growth of GBS in saline or Mueller-Hinton broth • Dip sterile swab in adjusted suspension • Inoculate entire surface of Mueller-Hinton sheep blood agar plate • Place erythromycin (15µg) disk & clindamycin (2µg) disks 12 mm apart – Incubate for 20-24 hrs at 35C in 5% CO2 • Blunting of inhibition zone around clindamycin disk adjacent to erythromycin disk are considered D-zone positive – If D-zone positive, report as clindamycin resistant D-zone Test Result for GBS Blunting of the inhibition zone indicating inducible clindamycin resistance Antimicrobial Susceptibility Test Broth Microdilution Dilution Low High concentration MIC 0.06 µg/ml Penicillin MIC 8 µg/ml Erythromycin Sterile control (MIC) Minimum Inhibitory Concentration Growth Control Other changes: Bacteriuria • 2002 guidelines required labs to report ANY quantity of GBS found in urine cultures • Required great deal of lab time • Studies of bacteriuria as evidence of ‘heavy’ colonization have used ≥104 CFU/mL as cutoff • Difficult with available data to determine significance of lower colony counts • 2010 recommendation is to report positive urine cultures with ≥104 cfu/mL of GBS ANTIBIOTICS: Note that antenatal antibiotics not shown to have benefit for vaginal colonisation with Group B streptococci. 1.2 g IV Benzyl penicillin initially and then 0.6g 4 hrly during labour. If penicillin allergic (and no history of anaphylaxis), cephazolin 2g initially then 1g 8hrly If prior anaphylactic reaction to penicillin the either vancomycin 1g 12 hrly, or clindamycin 600mg 8hrly are indicated. (NZ guidelines recommend vancomycin but clindamycin is fine if Gp B strep isolated and known to be susceptible.) This will decrease incidence of invasive disease in new-borns by approximately 90%, most effective if antibiotic started more than 4 hrs before delivery. If maternal chorioamnionitis (intra-partum fever with two of the following signs: foetal tachycardia, uterine tenderness, offensive vaginal discharge or increased maternal WCC) then penicillin alone is insufficient. Broad spectrum abx required eg Amoxycillin clavulanate RECOMMENDATIONS RECOMMENDATIONS • Pregnant women should undergo vaginal-rectal screening for GBS colonization at 35-37 weeks. • Intrapartum antibiotic prophylaxis (IAP) is recommended for: • o Women who delivered a previous infant with GBS disease • o Women with GBS bacteriuria in the current pregnancy • o Women with a GBS-positive screening result in the current pregnancy o Women with unknown GBS status who deliver at less than 37 weeks’ gestation, • have an intrapartum temperature of 100.4F or greater, • or have rupture of membranes for 18 hours or longer. • • Penicillin remains the preferred agent with ampicillin an acceptable alternative . RECOMMENDATIONS • personal hygiene. • Doctors and nurses are recommended to wash your hands before and after each screening process. • Sterilization of instruments used in the process of birth after each case. • The need to wear gloves at every screening process for pregnant women by doctors and nurses. • Change beds linens after each case in order to avoid the transfer of the microbe. RECOMMENDATIONS • Laboratory methods for the isolation, identification or detection of GBS should be made available at the Ministry of Health Labs • Updated algorithms for GBS screening and intrapartum chemoprophylaxis for women with preterm labor or preterm premature rupture of membranes, • A change in the recommended dose of penicillin-G for chemoprophylaxis, • Updated prophylaxis regimens for women with penicillin allergy. • A revised algorithm for management of newborns with respect to risk for early-onset GBS disease . MAIN MESSAGES • GBS infection/colonization is an essential part of mother/child care. • Every pregnant women should be examined for the presence of this microbe • Vaginal and rectal swabs are preferred for the lab detection • Several methods are available for the detection including culture, serology, and NAAT • Intrapartum antibiotic administration proved effective in preventing diseases for both mother and neonates نشكر لكم حضوركم وحسن استماعكم • مع حتيات: • خديجة طالل الحلو • ياسمين جالل الدنف. • حنين التلبانى. • أريج راشد الدريملي. قسم العلوم الطبية املخبرية