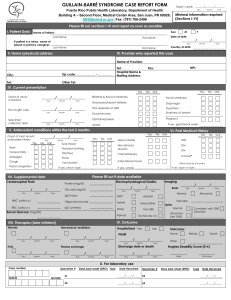
Guillain-Barre Syndrome
advertisement
July 30, 2008 PTE Guillain-Barre Syndrome Background & Definition Described in 1916 by Guillain, Barre, and Strohl Acute-onset immune-mediated disorder of the peripheral nervous system Aka acute inflammatory demyelinating polyradiculoneuropathy (AIDP) Clinical Features and Diagnosis Incidence rates are 1-2 per 100,000 population Lifetime likelihood of any individual acquiring BGS in 1:1000 M=F; occurs at any age Often predated by unremarkable infection (i.e. URTI/GI infections) by 10-14 days (examples include Campylobacter jejuni, CMV, Mycoplasma pnemonia, EBV, influenza virus) Usually begins with abrupt distal, relatively symmetrical onset of paresthesias, followed by progressive limb weakness Rapid progression with ~50% of patients reaching clinical nadir by 2 weeks and >90% by 4 weeks 80-90% of patients will become non-ambulatory during illness pain is prominent in ~50% Examination o Ascending dsistal and often proximal relatively symmetrical weakness o Sensory exam often normal in early phase o Widespread areflexia or hyporeflexia is the rule o Often develop cranial nerve weakness—facial or pharyngeal weakness Diaphragmatic weakness due to phrenic nerve involvement 1/3 of hospitalized patients require mechanical ventilation Autonomic dysfunction seen in >50%--usually manifest as tachycardia but may included arrhythmias, hypotension, hypertension, and GI dysmotility Diagnosis o Clinical suspicion o Elevated CSF protein (with normal cell count) found in ~50% of patients initially, but occurs in >90% at clinical nadir o EMG demonstrates features of demyelination (temporal dispersion, significantly slow conduction velocities, prolonged distal and F-wave latencies) Very low compound muscle action potentials (CMAP) is associated with poor long-term outcome o MRI of Spine/Brain useful to rule out mimics of GBS (myelopathy or infiltrative or compressive causes of polyradiculoneuropathy) may support diagnosis by showing enhancement of involved nerve roots or cranial nerves July 30, 2008 o no diagnostic value in antiganglioside antibody values Signs/Symptoms suggestive of alternate diagnoses o Intact reflexes despite generalized weakness o Asymmetric weakness o Fever during the initial presentation o Electrodiagnostic freatures inconsistent with an acquired demyelinating polyneuropathy PTE July 30, 2008 PTE July 30, 2008 PTE Variants Axonal injury occurs to some degree in many cases of GBS In severe GBS, significant secondary axonal damage will develop and impact the degree of residual damage and thus long-term outcome Variations of GBS include: o Severe axon loss o One particular fiber type (sensory or autonomic) is predominantly affected o Regional or markedly asymmetric distribution o Differences in abruptness or onset and time to reach nadir Miller-Fisher Syndrome o Classically present with external ophthalmoparesis, areflexia, ataxia o Generally a benign self-limiting condition o Almost all treated and untreated patients return to normal activities within 6 months of disease onset Acute axonal neuropathy form of GBS o Accounts for 5-10% of cases in North America o Characterized by immune attack directed at axons rather than Schwann cells and myelin o Course protracted with poor outcome; most patients require mechanical ventilation within a few days of symptom onset and only ~20% ambulating at 1 year July 30, 2008 PTE Mimics Pathophysiology Acute Inflammatory Demyelinating Polyradiculoneuropathy o Most common form of GBS o Pathologic characteristics of demyelination, lymphocytic infiltration, and macrophage-mediated clearance of myelin July 30, 2008 PTE o Epitopes on surface of infectious agents (C. jejuni, CMV, mycoplasma pneumonia, influenza virus) are similar to those on surface of peripheral nerves o Complement-fixing IgG antibodies bind to peripheral nerve gangliosides inducing autoimmune injury o Demyelination may occur throughout the length of the nerve; nerve terminal axons are also damaged Acute Axonal Neuropathy o Often follows infection with C. jejuni o AgG and complement mediated disorder (like AIDP); target epitopes are surface of axolemma of motor fibers o Antibody binding may cause conduction block, and thus may recover quickly if this antibody binding reversed before the development of significant axonal degeneration Miller Fisher Syndrome o Key difference from AIDP or acute motor axonal neuropathy is activation of anti-GQ1b and anti-GT1a antibodies that target oculomotor and bulbar nerves Management Immunotherapy o Plasma exchange Administered as one plasma volume, 50mL.kg, on five separate occasions over 1-2 weeks Shown to be cost-effective given decreased hospital stay Should be administered to nonambulant patients with GBS within 4 weeks and for ambulant patients within 2 weeks of symptom onset Data supports 2-4 plasma exchanges depending on severity Side Effects: hypotension, speticemia, pneumonia, abnormal clotting, complications from central venous access, hypocalcemia Contraindications: major hemostatic disorders, unstable cardiovascular status, active infection, pregnancy o IVIg Administered 2g/kg totatl divided over 2-5 days Give to patients with GBS who require aid to walk within 2 weeks or 4 weeks of neuropathic symptom onset Significant adverse effects: renal failure, myocardial infarction, vomiting, meningismus, ATN, thromboembolic events, anaphylactic reaction in those with IgA deficiency (risk 1:1000) o Steroids No role Choose PE or IVIG, but not both July 30, 2008 PTE Supportive Care Mortality from GBS is ~5%; up to 20% for ventilated patients o Causes: Pneumonia, ARDS, sepsis, PE, cardiac arrest Relapses in ~10%; consider repeat EMGs to check for CDIP (chronic demyelinating inflammatory polyneuropathy) Respiratory o Mechanical ventilation required in 20-30% of GBS patients o Predictors of imminent respiratory arrest (“20/30/40 rule”): VC<20mL/kg, max inspiratory pressure <30cm H2O, or max expiratory pressure >40cm H2O o Need for mechanical ventilation associated with Time from onset to admission <1 week Facial weakness Inability to cough Inability of lift head off of pillow Atelectasis on CXR Autonomic dysfunction o Mean duration of mechanical ventilation is 2-6 weeks Autonomic Dysfunction o Symptoms of cardiac, hemodynamic, GI, bladder o Most common pattern is sympathetic overactivity with parasympathetic underactivity o Urinary retention in up to 1/3 o Gastrointestinal motility disorder in 15% Long-term Issues 40% of hospitalized patients will require inpatient rehabilitation Persistent Symptoms and Disability o Recover is slow and can take years; majority of recover occurs over the first 6 months o Persistent disability in 20-30%; 2/3 will report significant disturbed sensation/loss of power at 1 year o Erasmus GBS Outcome Score (EGOS) Immunization o May increase risk of GBS by 1-2 per million o For patients who have GBS, immunizations are not recommended during the acute phase of GBS and porbalby not during a period, possible of 1 year, after onset of GBS; decisions about future immunization should be made on a case-by-case basis July 30, 2008 PTE References Burns, TM. Guillan-Barre Syndrome. Seminars in Neurology. 28(2):152-67, 2008 Apr. Green, DM. Weakness in the ICU: Guillain-Barre syndrome, myasthenia gravis, and critical illness polyneuropathy/myopathy.. Neurologist. 11(6):338-47, 2005 Nov. Hall & Schmidt. Critical Care: Just The Facts. 2007. pp218-220.