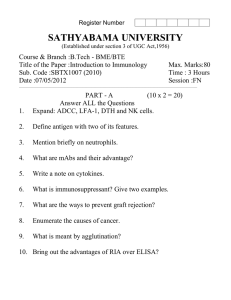
Second-Lecture-MHC
advertisement

Clonal Diversification of Lymphocytes Review of last lecture Whenever immature pre-T Cells recognize self-antigens, they are programmed to autodestruct in the Thymus Thymus Bone Marrow 98% pre-T cells die in the thymus Whereas Mature T cells proliferate when they contact antigens Treatments for Autoimmune diseases - Wipe out the mature B cells // Reboot – some exceptions Sjögren's Syndrome When immature pre-B Cells recognize self-antigens then they auto-destruct in the Bone Marrow Bone Marrow Tolerance to self substances Clones of Mature B Cells proliferate when contacting antigen One clone of B cells (B lymphocytes) by definition will only bind to one type of antigenic determinant e.g., either to outside determinant #1 or to #2 or to #3 1 Antigen 2 3 Mature B Cells B Cell B Cell clone #2 clone #1 Fc region 1 Antigen 2 3 Fab region B Cell clone #2 B Cell clone #1 After proliferating, many antigen stimulated B Cells differentiate into Plasma Cells Plasma Cell clone #1 Plasma Cell clone #2 Multi-clonal antibodies Multiclonal Stimulation Activation of specific clones of B cells Polyclonal Activation (non-specific activation of all B cell clones in the area by i.e., endotoxic LPS) Poly-CARBOHYDRATE ANTIGEN - repeating antigenic determinants PROTEIN ANTIGEN NO repeating Antigenic determinants B Cell B Cell IgM Requires T Cell help IgM IgG IgA Help comes via soluble substances produced by stimulated Helper T Cells Th Tc Helper T Cells CD 4 positive Helper T Cells help B Cells and Cytotoxic T Cells Cytotoxic T Cells CD 8 positive T LYMPHOCYTES T Cells T Cells have T Cell Receptors on their surface Not antibodies Helper T Cell clones Antigen The antigenic determinants are hidden within the antigen (are not yet processed), and need to be associated with a MHC 2 product Antigen Presenting Cells Bind in some cases via surface antibody (sometimes passively absorbed) or via complement deposited on the antigen then Phagocytize the antigen (see the lecture handout). Followed by DIGESTION of the antigen that must occur without infecting the cell. Note Ab and complement neutralize the antigen. Antigen Presenting Cells DO NOT Have T Cell Receptors All types of Antigen Presenting Cells (APC) continually produce Major Histocompatibility Complex Class II Products (MHC Class 2 Products) that are produced inside the cell move to the surface then and stay on the cell surface These MHC 2 products are only on cells which digest and then present the digested fragments of the antigens to Helper T cells Types of Antigen Presenting Cells: Macrophages and Macrophage-like cells Dendritic Cells (And Pre-dendritic Cells) B Cells (B lymphocytes) Types of Antigen Presenting Cells: Macrophages and Dendritic Cells have Fc-Receptors and Complement Receptors. Thus these types of APC also can become Armed with low levels of polyclonal Ab-Ag complexes via the Ab that may be weakly fitting (very weak affinity) at the beginning of the infection B Cells (B lymphocytes)-- monoclonal Ab Low levels of Ab to many substances Antigen Toll-Like Recptors Complement Receptors Antigen Presenting Cell must bind and digest the antigen Major Histocompatibility Complex (MHC) Class 2 Molecule GROOVE for an internal antigenic fragment (exposed after antigen was fragmented by host cell proteases) PLASMA MEMBRANE Antigen Presenting Cell e.g., macrophage Major Histocompatibility Complex MHC Class 2 Molecule GROOVE for an antigenic fragment ( fragmented by host cell proteases ) PLASMA MEMBRANE Antigen Presenting Cell Digested Fragments of the Antigen then Associate with MHC Class 2 products. Antigenic Determinants are now presented to helper T cells. APC binds to antigens and phagocytizes them. Then digests them and associates them with MHC 2 products. T cell receptor Helper T Cell With a correct T Cell Receptor CD4 CD4+ Antigen Presenting Cell (APC) APC binds to antigens and phagocytizes them. Then digests them and associates them with MHC 2 products. Interleukins liberated. Molecules that stimulate/help any type of T cells and any B cells that have contacted their antigenic determinants Helper T Cell With a correct T Cell Receptor CD4+ Antigen Presenting Cell (APC) Major Histocompatibility Complex Products MHC Also termed HLA Human Leukocyte Antigens After the T Cell Receptor binds to the antigenic fragment within the appropriate MHC product, then cells are close enough together so that Class 2 products interact with CD4 on Helper T Cells Major Histocompatibility Complex (Products) Type 1 (MHC Class 1) Class 1 products are always being produced on virtually all host cells. Major Histocompatibility Complex (MHC) Class 1 Product GROOVE Beta 2 Microglobulin PLASMA MEMBRANE SYNTHESIZED VIRAL FRAGMENTS in the Infected Host Cell series of different small synthesized viral fragments-Virally become associated Infected with MHC 1 products Host being produced by Cell the host cell SYNTHESIZED VIRAL FRAGMENTS series of different small synthesized viral fragments these associate with MHC 1 products Virally Infected Host Cell a bud or pocket of intact virus particles ready to leave the host cell Before it dies, the virally infected cell becomes a viral factory Major Histocompatibility Complex (MHC) Class 1 Drawing of the MHC 1 Molecular Complex Note the GROOVE outside surface PLASMA MEMBRANE Normal Host Cell One Major Histocompatibility Complex (MHC) Class 1 product associates with one of the many viral fragments synthesized within the host cell. Then the MHC-1 + viral fragment travels to the surface. Other MHC class 1 products associate with other synthesized viral fragments. synthesized GROOVE for small viral fragment GROOVE containing one small synthesized viral fragment PLASMA MEMBRANE Virally Infected host cell MHC-1 + synthesized viral fragments Other MHC class 1 products associate with other synthesized viral fragments. synthesized GROOVE for small viral fragment PLASMA MEMBRANE MHC-1 + Infected host cell synthesized viral fragments To Review: SYNTHESIZED VIRAL FRAGMENTS bind the MHC 1 molecule, while inside the virally infected cell, then move to the cell surface. Virally Infected Host Cell Cytotoxic T Cell is stimulated (only) when encountering the complex of the Specific Antigenic Fragment (recognized by its T- Cell receptor) and the MHC Class 1 product series of different small synthesized viral fragments associated with MHC-1 on the infected cell’s surface Cytotoxic T Cell Virally Infected Host Cell T cell receptor Cytotoxic T Cell With a correct T Cell Receptor CD8+ CD8 Virally Infected Host Cell Cytotoxic T Cell With a correct T Cell Receptor CD8+ Virally Infected Host Cell From Another A Cytotoxic T Cell With another correct T Cell Receptor clone CD8+ Virally infected cell is terminated via direct damage and via signals to self-destruct Previous Pop Quiz Question 1: You recently saw a patient with severe inflammatory periodontal disease. Over twenty different specific B lymphocyte clones were detected in the tissues immediately surrounding the infected periodontal pockets. After several days the B cells in this area were again tested and several of the B cells clones had a higher affinity (or better fit) for the same antigens. How do Specific B cell clones recognize antigens? And why did the fit (affinity) become higher for selected clones? Question 2: Pregnant ladies are advised not to receive x-rays because rapidly dividing cells are very susceptible to DNA damage. Describe fetal T cell clonal development. What would be the possible consequences of x-rays on fetal T cell clonal development? Previous Take-Home Open-Book Examination from Dr. Boackle Along with T cells, monocytes/macrophages, and high numbers of PMNs (polymorphonuclear leukocytes), a curiously elevated number of B lymphocytes and plasma cells are observed in the inflamed tissues in periodontal disease. What specific and non-specific mechanisms might be responsible for the observed numbers of stimulated B cells in these periodontal tissues? What are Toll-Like receptors and what are their possible roles in periodontal disease, especially in face of the infection with gram-negative bacteria? P Primary and secondary signals are needed for the proper stimulation and function of specific T cells (T lymphocyte clones) and of specific B cells (B lymphocyte clones) that are present in the periodontal tissues. Indeed, specific immune responses to periodontal organisms certainly occur. Describe how those lymphocytes first arrived in the inflamed periodontal tissues, then describe in detail the respective primary and secondary signals that stimulate the activation and proliferation of specific T cells (T lymphocyte clones) and of specific B cells (B lymphocyte clones)-be sure to discuss antigen presentation. Fully explain the reasons that each signal or contact is needed for proliferation of these specific lymphocytes. Quoted from TH2 Produce Defense against Parasitic worms, allergy, asthma TH1 Undifferentiated T Helper Cell TH17 Treg Defense against intracellular pathogens Defense against extracellular bacteria, autoimmunity, cancer Immunosuppression Upon antigenic stimulation, naïve CD4+ T cells (Undifferentiated T Helper Cells) undergo proliferation and differentiate into cytokine-producing T helper (T(H)) effector cells. T(H)2 cells produce IL-4, IL-5, and IL-13 cytokines, and mediate immunity against extracellular pathogens and allergic reactions; whereas T(H)1 cells secrete effector cytokine IFNgamma and regulate cell-mediated immunity. Directly Quoted from Pappu BP, Dong C. Curr Protoc Immunol. 2007 Nov;Chapter 6:Unit 6.25. Quoted from TH2 Produce Defense against Parasitic worms, allergy, asthma TH1 Undifferentiated T Helper Cell TH17 Defense against intracellular pathogens Defense against extracellular bacteria, autoimmunity, cancer Treg Immunosuppression Recent studies have identified a novel T(H) subset, called T(H)17, TH(IL-17), or inflammatory T(H) (THi) cells, characterized by the production of a proinflammatory cytokine, IL-17, and regulating inflammatory responses. Thus TH17 cells may play a role in the pathogenesis of Rheumatoid Arthritis. Simvastatin (a statin) induces IFN-gamma, IL-4, and IL-27 production in monocytes, which together inhibited IL-17 transcription and secretion in CD4(+) T cells. Could statins represent a promising therapeutic approach for multiple sclerosis and other chronic inflammatory diseases? Zhang et al 2008 J. Immunol.;180:6988-96. Quoted from TH2 Produce Defense against Parasitic worms, allergy, asthma TH1 Undifferentiated T Helper Cell TH17 Treg Defense against intracellular pathogens Defense against extracellular bacteria, autoimmunity, cancer Immunosuppression Treg play a critical role in the maintenance of peripheral tolerance to self-proteins. However Tregs may also facilitate early protective responses to local viral infections by somehow allowing a timely entry of immune cells (natural killer cells, dendritic cells, and T cells) to the site of infection. Concomitantly, Tregs help to prevent bystander damage to host tissues. Lund et al., Science. 2008 Apr 24