Human Biology (BIOL 104)
advertisement

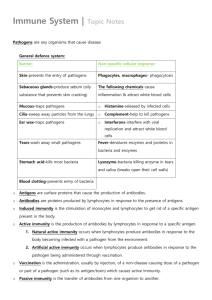
Human Biology (BIOL 104) Talk Seven: Blood and the immune system Chapters 8 and 9 Functions Of Blood • Transportation – – the blood transports dissolved gases, nutrients, hormones and metabolic wastes. • Protection – – the blood restricts fluid losses through damaged vessels. – Platelets in the blood and clotting proteins minimize blood loss when a blood vessel is damaged. • Regulation – Blood regulates the pH and electrolyte composition of the interstitial fluids. – Blood regulates body temperature. Composition Of Blood • Contains cellular and liquid components • A specialized connective tissue – Blood cells – formed elements – Plasma – fluid portion and fibrinogen • Blood volume – Males: 5 – 6 liters – Females: 4 – 5 liters • The pH of blood is about 7.35-7.45 Composition Of Blood From Wikimedia Commons, a freely licensed media file repository Composition of Whole Blood Composition of Whole Blood Composition of Whole Blood The Blood, a quick look A. Plasma • Liquid portion of the blood. • • • • • • • Contains: clotting factors, Hormones Antibodies dissolved gases Nutrients waste Copyright ©The McGraw-Hill Companies; used with permission Composition of Whole Blood The Blood, a quick look B. Erythrocytes - Red Blood Cells • Carry hemoglobin and oxygen. • Do not have a nucleus and live only about 120 days. • Can not repair themselves. Copyright ©The McGraw-Hill Companies; used with permission Composition of Whole Blood The Blood, a quick look C. Leukocytes – White Blood cells • Fight infection and are formed in the bone marrow • • • • • • Five types – neutrophil, lymphocytes eosinophils basophils monocytes. Copyright ©The McGraw-Hill Companies; used with permission Composition of Whole Blood The Blood, a quick look •D. Thrombocytes – Platelets. •These are cell fragment that are formed in the bone marrow from magakaryocytes. •Clot Blood by sticking together – via protein fibers called fibrin. Copyright ©The McGraw-Hill Companies; used with permission Blood Plasma • Straw-colored, sticky fluid portion of blood • Approximately 90% water • Contains: – Ions – Na+ and Cl– Nutrients – sugars, amino acids, lipids, cholesterol, vitamins and trace elements – Three main proteins Albumin (60%), globulin (35%), fibrinogen (4%) – Dissolved Gasses – including O2 and CO2 – Waste Products – other protein wastes such as urea Erythrocytes – Red Blood Cells (RBCs) • Oxygen-transporting cells – 7.5 µm in diameter (diameter of capillary 8 – 10µm) • Most numerous of the formed elements – Females: 4.3 – 5.2 million cells/cubic millimeter – Males: 5.2 – 5.8 million cells/cubic millimeter • Made in the red bone marrow in long bones, cranial bones, ribs, sternum, and vertebrae • Average lifespan 100 – 120 days RBC Structure And Function • Have no organelles or nuclei • Hemoglobin – oxygen carrying protein – Each RBC has about 280 million hemoglobin molecules • Biconcave shape – 30% more surface area Red Blood Cells Copyright ©The McGraw-Hill Companies; used with permission Erythropoietin • Produced in the kidney • Low Oxygen in blood signals production • Athletes: – Erythropoietin Injections – Blood Doping – Increase Viscosity Increase Blood Pressure! From Wikimedia Commons, a freely licensed media file repository RBC life span and circulation • Replaced at a rate of about 3 million new blood cells entering the circulation per second • Damaged or dead RBCs are recycled by phagocytes (in Spleen) • Components of hemoglobin individually recycled – Heme stripped of iron and converted to biliverdin, then bilirubin • Iron is recycled by being stored in phagocytes, or transported throughout the blood stream bound to transferrin Copyright ©The McGraw-Hill Companies; used with permission Leukocytes – White Blood Cells (WBCs) • Protect the body from infectious microorganisms • 4,800 – 11,000/cubic millimeter • Function outside the bloodstream in loose connective tissue • Diapedesis – circulating leukocytes leave the capillaries • WBCs have a nucleus and are larger than RBCs • Most produced in bone marrow • Lifespan of 12 hours to several years • Granular Leukocytes • Neutrophils: Most abundant. Have multi-lobed nucleus. – They are the first to respond to infection, and engulf pathogens during phagocytosis. – Eosinophils: Have bi-lobed nucleus • Known to increase in number in the event of parasitic worm infection and during allergic reaction. – Basophils: U-shaped or lobed nucleus. • In connective tissues release histamines along with Mast Cells From the wikimedia free licensed media file repository • Agranular Leukocyles – Monocytes: Largest of the white blood cells. • Differentiate into even larger Macrophages • Phagocytize pathogens, old cells and debris • Stimulate production of other white blood cells – Lymphocytes: Two types: • T-lymphocytes – Destroy any cell with foreign antigens • B-lymphocytes – Produce antibodies that combine with antigens – Target pathogens for destruction From the wikimedia free licensed media file repository White Blood Cells Type Of White Blood Cells % By Volume Of WBC Description Function Neutrophils 60 – 70 % Nucleus has many interconnected lobes; blue granules Phagocytize and destory bacteria; most numerous WBC Eosinophils 2–4% Nucleus has bilobed nuclei; red or yellow granules containing digestive enzymes Play a role in ending allergic reactions <1% Bilobed nuclei hidden by large purple granules full of chemical mediators of inflammation Function in inflammation medication; similar in function to mast cells Dense, purple staining, round nucleus; little cytoplasm the most important cells of the immune system; effective in fighting infectious organisms; act against a specific foreign molecule (antigen) Largest leukocyte; kidney shaped nucleus Transform into macrophages; phagocytic cells Basophils Lymphocytes (B Cells and 20 – 25 % T Cells) Monocytes 4–8% Summary of Formed Elements Platelets • Structure – Small cellular fragments; originate in bone marrow from giant cell megakaryocyte – Contain several clotting factors – calcium ions, ADP, serotonin • Function – Involved in stopping bleeding when a blood vessel is damaged; Process is called hemostasis Blood Cell Formation • Hematopoiesis – process by which blood cells are formed • 100 billion new blood cells formed each day • Takes place in the red bone marrow of the humerus, femur, sternum, ribs, vertebra and pelvis – Red marrow – actively generates new blood cells • Contains immature erythrocytes • Remains in epiphyses, girdles, and axial skeleton – Yellow marrow – dormant • Contains many fat cells • Located in the long bones of adults – Tissue framework for red marrow • Reticular connective tissue Cell Lines in Blood Cell Formation • All blood cells originate in bone marrow • All originate from one cell type • Blood stem cell (pluripotential hematopoeitic stem cell) – Lymphoid stem cells - give rise to lymphocytes – Myeloid stem cells - give rise to all other blood cells Human Blood Groups • A, B, AB, and o • First found during the Crimean war (1854 – 1856) – British Army Surgeon kept records of successful blood transfusions • A to A and B to B worked • A to B or B to A were always fatal • Also found that o was the universal donor – People with this type of blood can give it to anyone • AB type people can receive blood from anyone – Universal recipient. Why does this happen? Figure 7.4 Both type A and type B blood have specific carbohydrates which are on the surface of the blood cells. AB blood has both carbohydrates on the surface of the blood cells o blood has no carbohydrates Carbohydrates are: N-Acetylglucosamine, galactose and fucose Also known as antigens Why does this happen? http://learn.genetics.utah.edu/units/basics/blood/types.cfm Why does this happen? Figure 7.4 Antigen: Molecule that stimulates an immune response, especially the production of antibodies by plasma B cells. Antigens are usually proteins or polysaccharides. A person who receives incorrectly matched blood will make antibodies against the blood group antigens. Blood cells clump together in blood vessels with fatal results. Why does this happen? Figure 7.4 Controlled by three alleles Allele A – dominant has info for making antigen A Allele B – dominant has info for making antigen B Allele o – recessive produces neither antigen AA & Ao gives rise to A type blood BB & Bo give rises to B type blood AB is co-dominant - AB type blood oo is recessive – o type blood Rh Factor • There are four blood groups but eight blood types. • The Rh-factor!! • • • • 85% Positive (US population) 15% Negative Genetic factor Can cause Hemolytic Disease and death of infants. The genetics of the Rh factor • Another blood grouping system independent of ABo – the Rh-factor – Again, three genes (alleles): located very close together on the same chromosome. • First C & c, second D & d, third E & e • Unlike the ABo system there is no codominance, c, d, and e are recessive to C, D, and E. • ccddee is known as Rh-negative. All others Rh-positive. How common is your blood type? 46.1% 38.8% 11.1% 3.9% How common is your blood type? 34 Hemolytic disease • If a child is Rh+, a Rh- Mother can begin to produce antibodies Rh+ red blood cells – Rh factor crosses placenta and mother makes antibodies • In subsequent pregnancies these antibodies can cross the placenta and cause hemolysis of a Rh+ Childs red blood cells. – Can lead to mental retardation or death • Prevented by giving Rh- women a Rh immunoglobulin injection no later than 72 hours after birth. Attacks any of the babies Abs in mother before her own antibodies are produced Hemolytic disease Figure 7.5 (1) Hemolytic disease Figure 7.5 (2) Hemolytic disease Figure 7.5 (3) •Prevented by giving Rh- women a Rh immunoglobulin injection no later than 72 hours after birth. •Attacks any of the babies Abs in mother before her own antibodies are produced. Malaria – an agent of natural Selection • As any species evolves, biological differences among its population arise largely through natural selection. • Diseases are among the selective forces that can result in genetic differences among populations. • In disease-ridden areas of the world, natural selection acts to increase the frequency of alleles that confer partial resistance to a disease while decreasing the frequency of alleles that leave people susceptible to a disease. Malaria – an agent of natural Selection • New traits are produced by mutation and are then subject to natural selection. • The traits that survive are adaptations. • Malaria causes 110 million cases of illness each year – Close to 2 million deaths each year. • Rare before the invention of agriculture – Did much to change the selective pressure on human populations Malaria – an agent of natural Selection Figure 7.8 (1) Malaria – an agent of natural Selection Figure 7.8 (2) Malaria – an agent of natural Selection Figure 7.8 (3) Malaria – an agent of natural Selection Figure 7.8 (4) Malaria – an agent of natural Selection Figure 7.8 (5) Malaria – an agent of natural Selection Figure 7.8 (6) Malaria – an agent of natural Selection Figure 7.9 sickle-cell anaemia • Hereditary blood disorder • Characterized by an abnormality in the oxygen-carrying hemoglobin molecule in red blood cells that leads to a propensity for the cells to assume an abnormal, rigid, sickle-like shape under certain circumstances. • Almost 300,000 children are born with a form of sickle cell disease every year, mostly in sub-Sarahan Africa but also in other countries such as the West Indies, South Asia and in people of African origin elsewhere in the world. From Wikimedia Commons, a freely licensed media file repository A small change in a gene can have many phenotypic consequences. Figure 7.10 Malaria – an agent of natural Selection • Most victims of malaria are young children • Where malaria occurrence is high, so is the HBs allele – Odd, as Sickle Cell Anemia is nearly always fatal before reproductive age – HBs allele confers resistance to malaria • So in areas of high occurrence to malaria, the HBs allele may cause a genetic disorder, but increases the overall fitness of a population where malaria occurs. Malaria – an agent of natural Selection The Immune System • Immunity is the ability to react to antigens so that the body remains free of disease. – Disease is a state of homeostatic imbalance. • Can be due to infection or failure of the immune system. Primary Lymphatic Organs • Lymphatic organs contain large numbers of lymphocytes (White Blood cells). • Primary organs are:– Red Bone Marrow. • Site of stem cells. – Source of B lymphocytes. – Thymus Gland. Lymphocytes from bone marrow pass through to form T-lymphocytes • Produces thymic hormones (thymosin). • Aids in T lymphocyte maturation. Secondary Lymphatic Organs • Secondary lymphatic organs are places where lymphocytes encounter and bind with antigens. – – – – Spleen. Lymph nodes. Tonsils. Peyer’s patches. Lymphatic Organs Secondary Lymphatic Organs • Spleen – upper left of abdominal cavity behind stomach. Sectioned off by connective tissue- white pulp & red pulp. – White pulp – lymphocytes – Red pulp – filters blood. Blood entering the spleen passes through red pulp before it leaves (network of sinuses) – FRAGILE Secondary Lymphatic Organs • Lymph Nodes – occur along lymphatic vessels. Formed from connective tissue. – Packed full of Blymphocytes – As lymph courses through sinuses it is filtered by macrophages, which engulf pathogens and debris. – Also present- Tlymphocytes – fight infection and attack cancer cells Secondary Lymphatic Organs • Tonsils – patches of lymphatic tissue. • Perform the same function as lymph nodes – First line of defense • Peyer’s Patches – on the intestinal wall and appendix. Attack pathogens that ender the body by way of the intestinal tract. Nonspecific Defenses • Barriers to Entry. – Mucous membranes • Line respiratory, digestive, and urinary tract. – Oil gland secretions. • Chemicals that kill or weaken bacteria on skin – Ciliated cells. • Sweep mucus & particles into throat – Bacteria • Both in stomach and vagina, prevent pathogens from gaining a foot-hold. – Acid Innate Immunity • One important function of the immune system is to promote growth and repair after injury – Either via physical damage or microorganisms • The mobilization of innate immune cells to get rid of damaged cells or microorganisms is called inflammation • Small molecules called cytokines are also involved Innate Immunity • Inflammatory Reaction. – Tissue damage causes – tissue cells and mast cells to release chemical mediators. Innate Immunity • Inflammatory Reaction. • Histamine and kinins. – Capillaries dilate and become more permeable. » Skin reddens and becomes warm. – Proteins and fluids escape from tissue. Swelling occurs Innate Immunity • Inflammatory Reaction. – Proteins and fluids escape from tissue and cause swelling. » Swelling stimulates free nerve endings, causing the sensation of pain. Innate Immunity – Neutrophils and Monocytes migrate to site of injury. – Amoeboid – can change shape – squeeze through capillary walls and enter tissue fluid. – Neutrophils engulf pathogens –destroyed by hydrolytic enzymes when fused to a lysosome Innate Immunity • Macrophages: Monocytes change into these as they leave the blood and enter the tissues. – These are phagocytic cells – Can eat many (100’s) of pathogens and survive. – Eat old blood cells and bits of dead tissue – Stimulate the immune response. • Increase production of white blood cells in bone marrow Innate Immunity • Macrophages: Monocytes change into these as they leave the blood and enter the tissues. • Macrophages enter lymph vessels carring bacteria fragments to lymph nodes • This starts a specific immune response Protective protein system • Known as Complement proteins • Are activated when pathogens enter the body. • Complement certain immune responses. Protective protein system • Attract phagocytes. • Form holes in bacteria. • Interferon binds to receptors of non-infected cells causing them to prepare for possible attack Specific immunity • Antigen--shape on cell, allows recognition of self and detection of foreign cells. • Antibody--protein that recognizes and binds antigens. • Specific defenses respond to antigens. – Lymphocytes recognize an antigen due to antigen receptors whose shape allows them to combine with a specific antigen. • Immunity is primarily the result of the action of B lymphocytes and T lymphocytes. Natural Killer Cells • Natural killer cells kill virus-infected cells and tumor cells by cell-to-cell contact. – Large, granular lymphocytes. T Cells • Provide cell-mediated immunity. • Produced in bone marrow, mature in thymus. • Antigen must be presented in groove of HLA molecule. • Cytotoxic T cells destroy non-self protein-bearing cells. • Helper T cells secrete cytokines that control the immune response. T cells attack foreign cells directly • Killer cells (“cytotoxic”), or CD8+ is a main type B Cells • Provide antibody-mediated immunity against bacteria. • Produced and mature in bone marrow. • Reside in spleen and lymph nodes. – Circulate in blood and lymph. • Directly recognize antigen and then undergo clonal selection. • Clonal expansion produces antibody-secreting plasma cells and memory B cells. • The antigen selects which lymphocyte will undergo clonal expansion and produce more lymphocytes with the same type of antigen receptor – Some become memory cells – long term immunity to the same infection. – B-cells become plasma cells – fight infection • Make Antibodies – Apoptosis – when danger of infection is over, all plasma cells undergo programmed cell death Clonal selection Theory Specific Defenses • Antibodies • A large Y-shape protein produced by plasma cells that is used by the immune system to identify and neutralize foreign objects such as bacteria and viruses. • The antibody recognizes a unique part of the foreign target, called an antigen • Each tip of the "Y" of an antibody contains a paratope that is specific for one particular epitope on an antigen – allowing these two structures to bind together with precision From the wikimedia free licensed media file repository Specific Defenses • Antibodies • Using this binding mechanism, an antibody can tag a microbe or an infected cell for attack by other parts of the immune system • or can neutralize its target directly (for example, by blocking a part of a microbe that is essential for its invasion and survival). • The production of antibodies is the main function of the human immune system. From the wikimedia free licensed media file repository Specific Defenses • Antibodies • Classes. • IgG - Enhances phagocytosis • IgM - Activates complement proteins. • IgA - Prevents attachment of pathogens. • IgD - Antigen receptors on virgin B cells. • IgE - Immediate allergic response. From the wikimedia free licensed media file repository Induced Immunity • Active Immunity. – Immunization involves use of vaccines. – Contain an antigen to which the immune system responds. – Primary response. Secondary (booster) response. – Dependent upon the presence of memory B and T cells capable of responding to lower antigen doses. Induced Immunity • Passive immunity • occurs when an individual is given prepared antibodies. – Temporary. • No memory cells. • Primary and secondary injections Issue - Allergies • Occurs when your immune system reacts atypically to some antigens to which the host does not need protection. • Pollen, dust mites, cats, a hard days work! – Called Allergens • The atypical response produces a special antibody – IgE • A form of innate immunity Allergies • IgE binds to mast cells. • When a person later encounters the same allergen, the allergen binds to the IgE on the mast cell • This triggers the explosive release of histamine • Capillaries dilate and become more permeable. • Skin reddens and becomes warm. Proteins and fluids escape from tissue. Swelling occurs – Allergies • The large amounts of histamines released in an allergic reaction cause strong symptoms • Runny eyes, sneezing, or shortness of breath • Depends upon the tissue in which the mast cells were triggered Allergies • As allergy symptoms are caused by histamines, taking antihistamines stops the build up of histamines in the cells of blood vessels. • However, antihistamines do not stop the immune response or the release of histamines in mast cells • Other allergies are mediated by T-cells – Latex, poison ivy, dyes or chemicals in cosmetics or clothing – Antihistamines do not help in these allergic reactions Allergies • As each allergy is an antigen-specific immune response it shows memory and a greater response on the next exposure – This is why allergies get worse over time • Thousands of different substances can produce allergies in people – each triggered by a specific antigen-specific response – Why people are usually bothered by only a few • Appears to be inherited