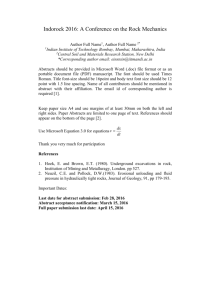
Informed Consent - Oregon Counseling Association
advertisement

Oregon Counseling Association Valley River Inn – Eugene, OR 2013 Fall Conference Pre-Conference Workshop Ethical Issues in 21st Century Clinical Practice November 7, 2013 Presenter: Douglas S. Querin, JD, LPC, CADC-I Introductions & Overview Who we are …. & Why we’re here 3/22/2016 3/22/2016 2 Caveats Today’s Comments are Not … Legal Advice Treatment Advice In lieu of Consultation/Supervision ___________________ Our Focus: How to Manage the Clinical Environment … from an Ethical Perspective 3/22/2016 3 Socrates had it Right… Dialogue & Interaction … Help us Learn Comments & Questions … Are Encouraged! 3/22/2016 3/22/2016 4 A Preliminary Observation Learning vs. Being Reminded 3/22/2016 5 Another Preliminary Observation Mental Health Professions & Codes Similarities vs. Differences 3/22/2016 6 Our Road Map I. Principles & Values II. Ethics vs. Law III. Informed Consent IV. Boundaries V. Reporting Misconduct 3/22/2016 7 Now …. a Word about “Ethics” Professional Ethics Basic Characteristics 1. Regulate Conduct 2. Determined by Consensus 3. Change over time 3/22/2016 3/22/2016 9 Our Goal Today …. Pulling Back the Curtain on Prof’l Ethics Professional Ethics Largely Informed by….. Moral Principles 1. Do No Harm 2. Promote Client Welfare 3. Promote SelfDetermination 4. Honor Faithfulness (Keeping Promises) 5. Honor Equality 6. Be Truthful 3/22/2016 11 11 Professional Ethics Also Informed by…. Laws Insur./Managed Care Social Trends/Policies Clinical Standards Technology Professionalism The Result: Competition between …. Laws, Ethics Codes, Morals, Clinical, Professional, and Social Responsibilities 3/22/2016 3/22/2016 13 13 AND … Competition between Individuals & Institutions Client THERAPIST 14 Deciding between Competing Ethical Responsibilities? 15 15 Let’s Assume …. An ethical issue has arisen in your clinical practice. There are potentially serious consequences to your client depending on how you handle the matter. You resolve the matter and the outcome is very poor. After the fact, you are asked: What Plan did you have, what Factors did you consider, and what Resources did you rely on, in reaching the decisions you did in handling this matter? How would you like to be able to respond? 16 Having an Ethical Decision-Making Model Just Might be … a Good Idea !!! “While there is no specific ethical decision-making model that is most effective, counselors are expected to be familiar with a credible model of [ethical] decision making …” Do we have a Plan (i.e., Credible Model)? ACA Code of Ethics, Statement of Purpose, p. 3, (2005) 3/22/2016 17 How is Professional Conduct Regulated? 1. Licensing Boards & Professional Associations 2. Legal Actions Organiz’l Rules, Ag’mts, Contracts 3. 3/22/2016 (E.g., EAPs, Employers, Agencies, etc.) 18 18 A Brief Legal Primer The Law 19 Legal Actions (1) Criminal: Government actions; Sanctions include fines or imprisonment (2) Civil: Actions (non-criminal) by one Party claiming, gen’ly damages against another (3) Administrative: Actions by State Regulatory Agencies (e.g., Licensing Boards) 3/22/2016 20 Civil Law Action: Malpractice (1) Duty: Professional’s Responsibility to “Clients” (and others !) to conform to Recognized Standards of the Professional Community (2) Deviation: From those Standards (aka Negligence; Breach of Duty) (3) Damages: Physical, Emotional, Economic Injury or Loss (4) Direct Link: Causal Connection 3/22/2016 21 The Realities of Civil Litigation (i.e., Malpractice) Fees & Costs Proof/Elements of Case Time & Expense Justifying Time & Expense The “Major Case” rule Such as …… 3/22/2016 22 Licensing Board Complaint vs. Malpractice Claim Lic. Board Complaint One issue: Regs violated? Lawyer unnecessary No fees or costs Relatively quick resolution Malpractice 4 Issues: Duty, Deviation, Direct Cause, Damages Lawyer necessary Attorney fees Expensive/lengthy Now a word or two about … Informed Consent In the Beginning…. … there were Doctors 3/22/2016 25 What did Hippocrates tell us? “… I will prescribe regimens for the good of my patients according to my ability and my judgment …..” That is….. Physician knows best Dr. was “The Decider” Patriarchal; limited patient Autonomy 3/22/2016 26 Informed Consent Gone Awry In the Name of Medicine…. Historically, Informed Consent was: Physician’s Prerogative Not Patient’s Right Egregious Consequences: Tuskegee, Ala. 1932 3/22/2016 27 Patients’ Rights – Have Evolved Consumers Lawyers Canterbury v. Spence, 464 F.2nd 772 (1972), et al. Doctor’s Prerogative Patient’s Right 28 Chestnut Lodge Osheroff vs. Chestnut Lodge (1980) Informed Consent & Psychotherapy 29 Today Informed Consent is ….. 1. Req’d in All Health Care Professions 2. Client’s Fundamental Right - To Knowingly Accept or Refuse Tx 3. Professional’s Affirmative Duty 4. An Active, not passive, Duty 3/22/2016 30 Remember…. Informed Consent = Permission to Tx Permission to Treat Requires…. (1) Capacity…of this Client (2) Voluntariness…by Client (3) Sufficiency of Info to Client 3/22/2016 32 Quality of Informed Consent (1) CONTENT – What’s Delivered (2) PROCESS – How Delivered (3) TIMING – When Delivered 3/22/2016 33 CONTENT (Clinical Considerations, Laws, Regs, Codes, Risks) Extent/nature of services Limits of confidentiality Risks/rights, alternatives Uncertain outcome Right to accept/refuse Tx Right to participate in Tx planning Fees, Cancellations, & Collection policies Taping, Recording, Observation of Sessions 3/22/2016 34 CONTENT Information to Provide Termination/Interruption of Service Both Planned & Unplanned Custodian of Record Inform Client of Supervision Parental Consent Issues; Group Therapy Issues Coordination of treatment with other Tx Providers _____________ I/C Rules Apply to Each Person in Client Unit (i.e., individual, couples, families, groups) 3/22/2016 35 CONTENT The Challenge Finding the Right Balance Too Much Detail: Legalistic & Confusing Too Little Detail: Unhelpful & Misleading 3/22/2016 36 Informed Consent : PROCESS Delivery Options 1. In Writing 2. Verbally BOTH …are Necessary 3/22/2016 37 Informed Consent - Written Informed Consent is too often viewed as a Risk Management Tool … … a Legal Document … for Organiz’l Protection … to get Signed ASAP Client Understanding ….. …. is often Not the Priority! 3/22/2016 38 Plain Language Some Recommendations 1. Signatures: By All Parties 2. Copies: To All Parties 3. Document: Receipt … & Client’s Understanding AND 4. Plain Language, when possible See, Flesch Readability Calculator See, http://www.cdc.gov/healthliteracy/pdf/SimplyPut.pdf 3/22/2016 39 PROCESS – VERBAL Informed Consent…Does Not end with client’s signature on written document 3/22/2016 40 TIMING When to Inform Client Clients Change: Issues may change Clinical needs may change Interventions may change All the reasons for obtaining Informed Consent in the first place continue to exist throughout therapy!!! Continuing Responsibility 3/22/2016 41 What Ethics Codes tell us about Informed Consent Address it at Start of Therapy… …and Throughout Therapy: “… as early as feasible” and as “circumstances may necessitate” (AAMFT) “reassessed throughout” (AMHCA) “ongoing part” of counseling (ACA) 3/22/2016 42 Thorough Informed Consent Benefits Research suggests: >Client Autonomy >Respect >Trust >Buy-in >Adherence to Tx Plan >Speed of Recovery < Anxiety 3/22/2016 43 Boundaries & Multiple Relationships Drawing Lines Wearing Different Hats & 3/22/2016 44 Boundaries Do we need them? Why? 3/22/2016 45 Boundaries – 3 Types 1. Classic/Traditional Boundaries 2. Boundary “Crossings” 3. Boundary “Violations” 3/22/2016 46 Boundary Types 1. Traditional /Classic Psychoanalytical perspective “Blank Slate” Transference Process Keep Physical & Emotional Distance Discouraged: Out-of-office Contact, Selfdisclosure, Touch, Expressions of Familiarity/Warmth; Gifts 3/22/2016 47 Boundary Types 2. Boundary “Crossings” Modern Trend (“Crossings”): Crossing Traditional Boundaries Beneficial to Client/Supervisee Low risk of harm Not Unethical per se Look at Context Multicultural Influences Acceptable w/in Prof’l Community See e.g., ACA Code, Section F.3., p. 14. 3/22/2016 48 Boundary “Crossings” Common Examples Therapist Self-Disclosure Accepting Modest Gift Gentle Touch or Hug Attending Formal Ceremony Rural Communities Realities Inadvertent Boundary Crossings Grocery store, movie theatre, etc. Generally, occur by Choice/Chance 3/22/2016 49 The Internet Assume your clients will see….. 1. All Online postings with your name 2. All your Facebook pages & postings (and other social media sites) – unless secure privacy settings 3. All photos and other info posted by your “friends” that may identify you, unless they too have secure privacy setting 4. Match.com – Internet dating Search Yourself Regularly on Internet http://www.zurinstitute.com/onlinedisclosure.html Boundary Types 3. Boundary “Violations” Signif Departure/Prof’l Standards Potential for Serious Harm: Therapeutic Neutrality Power Diff.; Exploitation Threat to Relationship & Process “Violations” – Start w/ Boundary Crossings and Progress; Occur Intentionally … Not Accidentally 3/22/2016 51 Is this a “Crossing” or a “Violation”? Considerations Client/Clinical – Presenting issue, mental status, age, gender, culture, social support, etc. Setting – In-Pt/Out-Pt, rural, etc. Therapy – Orientation, stage of therapy, etc. Therapist – Age, gender, experience, etc. Prof’l Community - Standards Purpose – Intent of therapist/client, etc. Possible Consequences – Harm, “MULTIPLE RELATIONSHIPS” Basic Features Additional, Non-Therapeutic Relationship Client Becomes something more: Friend, business associate, lessor/lessee; romantic partner; debtor/creditor, fellow church, board member, etc. Multiple Boundary Crossings/Violations Always some Potential Risk 3/22/2016 53 Multiple Relationships Variations & Considerations Concurrent or Consecutive Promising a Future Relationship Includes Family Members & Significant Others Generally Irrelevant: Which relationship began first Who initiated; Client consent Whether occurred by chance/choice Professional vs. Non-Professional Length of Time; When began (start, middle, end of therapy) 3/22/2016 54 Multiple Relationships Three Types (1) Sexual/Romantic Relationships (2) Non-Sexual/Non-Romantic (3) Professional Role Changes 3/22/2016 55 Sexual/Romantic Relationships Ethics Codes Current Clients/Supervisees: All Codes Prohibit Many Codes: Prohibit Relationships w/Client’s Family Members/Significant Others Former Clients: Most Codes Prohibit; w/differing time limits; ACCBO, NAADAC, NASW totally prohibit Former Romantic Partners: Prohibited Former Supervisees: Most Codes Silent No “True Love” Exceptions!!! 3/22/2016 56 Sexual/Romantic Relationships Sobering Statistics Sexual violations – 20% - 35% of licensing board complaints filed against counselors & therapists (Falvey, 2002, p. 76) “Across eight national self-report surveys, …nearly 7% of male & 2% of female therapists reported engaging in sex with at least one client.” (Ibid.) 3/22/2016 57 Sexual/Romantic Relationships Sobering Statistics Therapist-Client sexual relationships make up: 18% of Malpractice claims 41% of Malpractice claim payouts 20% Licensing Board Complaints Pope, K. S., & Vasquez, M. J. T. (2001). Ethics in psychotherapy and counseling: A practical guide. San Francisco, CA: Jossey-Bass. 3/22/2016 58 Sexual/Romantic Dual Relationships Demographics Primarily middle-aged Male therapists Primarily younger Female clients Single Most Predictive factor? Risk Management “Vicarious Liability” – Liability for the conduct of those over whom you have a right/duty to exercise control At Risk: Supervisors, Agencies, Employers 3/22/2016 59 Multiple Relationships (2) Non-Sexual/Romantic Threshold Questions Therapeutic Benefit? What’s the Purpose? Potential Impairment of Prof’l Judgment? Harm to Client/Others? Repairable? Discussed w/Client? Informed Consent? Consultation? Documentation? Unavoidable? (e.g., Rural/Specific Client Pop.) Accepted Standards w/in Prof’l Community? 3/22/2016 60 Multiple Relationships Non-Sexual/Romantic The Ethics Codes Ethics Codes – all essentially the same Potential Harm Test: Avoid M/R with Clients & Supervisees that create risk of harm: impair judgment/objectivity, risk exploitation, result in undue influence Potential Benefit Test: Avoid M/R unless “Potentially Beneficial ” (See, ACA – A.5.d & F.3.e.) 3/22/2016 61 Multiple Relationships with ….. Former Clients Factors Considered by Ethics Boards: Amount of time passed since therapy Nature and duration of therapy Client’s personal history & diagnosis Likelihood of adverse impact/exploitation Discussed/Planned Before End of Therapy Informed Consent - Thorough Consultation & Documentation in File 3/22/2016 62 Multiple Relationships (3) Changing Professional Role Changing Professional Roles Examples: Changing from Couples, Family, Group Individual Counseling…and vice versa Practice Tips when Changing Roles a. Obtain Informed Consent: Advise of Potential Consequences & How information from First Role may affect Second Role b. Therapy Forensic Role (and vice versa): Risky! c. Consult when appropriate; Always Document 3/22/2016 63 Multiple Relationships Risk Management - Tips Prior to & During M/R 1) Obtain Signed Informed Consent 2) Identify & Discuss issues, risks, benefits 3) Suggest 2nd opinion 4) Clarify client’s right to w/draw 5) Periodically Revisit & Document - Rationale/Potential Benefit - Consequences & Risks 3/22/2016 64 The Take-Away 1. Boundaries & Dual Relationships are NOT inherently unethical 2. They may be Therapeutically Appropriate … or Potentially Harmful 3. They must to be carefully evaluated, cautiously used, appropriately documented Multiple Relationships Risk Management Caveat If issues are raised about Propriety of a Multiple Relationship… …the Professional will bear The Laboring Oar 3/22/2016 66 Reporting Prof’l Misconduct Self-Reporting ORS 676.150 Duty to Self-Report All Codes: Prohibit - Practicing while “Impaired” Must Self-Report (10 days): Misdemeanor/Felony – Conviction Felony – Arrest Most Codes require Self-Reporting (often w/in 30 days): Civil Lawsuits (practice related) Prof’l & Regulatory Sanctions Failure to Self-Report Potential Discipline 3/22/2016 68 Reporting: Other Health Care Professionals ORS 676.150 Licensed* Health Professionals must Report Other Licensees, including Licensees of Other Health Licensing Boards, who engage in: (a) “Prohibited Conduct” OR (b) “Unprofessional Conduct” * Includes regulated pre-licensed professionals 3/22/2016 69 Reporting Professional Misconduct of Others “Prohibited Conduct” = Criminal Acts… (1) … against a patient or client, or (2) … such acts that create a risk of harm to a patient or client 3/22/2016 70 Reporting Professional Misconduct of Others “Unprofessional Conduct” = Conduct … unbecoming a licensee, or detrimental to the best interests of the public, contrary to recognized standards of licensee’s professional ethics endangers the health, safety or welfare of a patient or client Failure to Report Potential Discipline Reporting Professional Misconduct of Others Reporting licensee must have “reasonable cause to believe”; Includes credible hearsay Shall make report to appropriate licensing board Exception: When state/federal law prohibits disclosure (e.g., Therapist – Client Confid’ty) Confidential Communications are protected; Exempt from reporting Report w/in 10 days Civil Immunity – reports made in “good faith” 3/22/2016 72 Reporting Professional Misconduct of Others Some Scenarios Supervision & Consultation The client reveals misconduct by another health care professional Observations at the dinner party The inebriated professional Ethical Issues in 21st Century Clinical Practice* Thank you ! ____________________ Douglas S. Querin, JD, LPC, CADC-I dsquerin@comcast.net 3/22/2016 74