PA Department of Health Office of Health Equity
advertisement

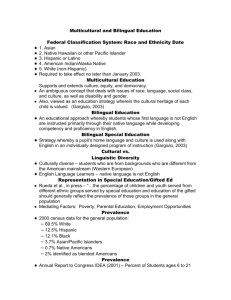
Health Disparities: Visions of a New Approach to Health Care Frank McClellan Beck Chair Professor of Law, Co-Director Center of Health Law, Policy and Practice Beasley School of Law at Temple University Seeing Patients: Unconscious Bias in Health Care The Story of Mr. Jackson • • • • • • • History of Heart Disease Diabetes High Blood pressure Heart Attack Emergency Room Visit Dies 6 hours later in treatment room Never seen by cardiologist at hospital Life Expectancy by Race and Gender 90 80.4 80 70 76.2 69.2 72.9 75.6 78.1 83.1 77.9 80.6 Years 60 Male Female Total 50 40 30 20 10 0 Black White Hispanic Race Source: CDC Vital and Health Statistics Report October 2010, United States Life Tables by Hispanic Origin, http://www.cdc.gov/nchs/data/series/sr_02/sr02_152.pdf - study from 2006 Work Life Expectancy by Age, Gender and Race ALL MEN AGE 1979-80 ALL WOMEN 1992-93 1997-98 1979-80 1992-93 1997-98 20 36.8 36.0 36.9 27.2 30.0 31.6 25 33.1 32.6 33.4 24.0 26.7 28.3 30 28.9 28.5 29.3 20.8 23.2 24.6 35 24.5 24.2 24.9 17.6 19.7 20.9 40 20.0 19.8 20.6 14.3 16.1 17.1 African-American Men Age 1992-93 Nonwhite Men 1997-98 1992-93 1997-98 White Men 1992-93 1997-98 20 29.4 29.4 30.6 32.2 37.0 37.7 25 26.8 26.5 27.9 29.4 33.4 34.1 30 23.4 22.9 24.5 25.7 29.2 29.8 35 19.8 19.1 20.7 21.8 24.7 25.4 15.9 15.4 16.7 17.9 20.3 21.0 40 Nonwhite includes African-American and Hispanic origin, Asians & Pacific Islanders, American Indians, and Alaskan natives Source: Work Life Estimates at Millennium's End: Changes over the Last Eighteen Years By: James Ciecka, Thomas Donley, and Jerry Goldman; Based on Data from the US Bureau of Labor Statistics (1986) and Ciecka, Donley, and Goldman (1995 and 1999); http://lmi.ides.state.il.us/lmr/worklife.htm Source: CDC, NCHS, Health, United States, 2008, Table 18 http://www.cdc.gov/nchs/data/hus/hus08.pdf & U nk no w n o an 4.4 La tin Am er ic 5.5 an ic/ h Hi sp So ut Cu ba n n 5.6 Ri ca n c 4.9 M ex ica pa ni 5 Hi s Is la nd er ive 8.1 O th er c Na t an 5.7 Pu er to ac ifi Al as ka Am er ic 10 Ce nt ra l& an /P In di an / 13.6 As i an c an i ca n Af ri No nHi sp W hi te c an Am er ic pa ni Ra ce s No nHi s Al l 5.8 er ic ca n Am Af ri W hi te Infant Mortality Rate per 1,000 Live Births 15 13.3 8.3 6.9 6.4 4.7 0 Age-Adjusted Death Rate per 100,000 Live Births 99.1 100 80 60 50.3 50.7 42.4 40 23.5 20 0 All Races Non-Hispanic White White African American Hispanic Source: National Vital Statistics Report, 56(16), 6/11/08: Deaths: Preliminary Data for 2006, Table 8, p32 http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_16.pdf Age-Adjusted Maternal Mortality Rate per 100,000 Persons 35 31.7 30 25 20 15 12.4 10 9.6 9.1 Non-Hispanic White White 8.2 5 0 All Races African American Source: CDC, NCHS, Health, United States, 2008, Table 42. http://www.cdc.gov/nchs/data/hus/hus08.pdf Hispanic Health Care Divided: Race and Healing a Nation EMERGENCY ROOM VISITS and ACUTE CARE BASED ON RACIAL DISPARITIES Percentage of persons by race with at least one emergency department visit in a 12 month period (2007) 50 Percentage 40 30 20 25.2% 17.9% 20.1% 10 0 Hispanic White Black Race Source: National Center for Health Statistics, Data Brief, May 2010 – Emergency Department Visitors and Visits: Who Used the Emergency Room in 2007? Tamyra Garcia, Amy Bernstein, and Mary Ann Bush Acute Care Visits to Various Providers Percentage Out of 354 Million Average Annual Visits Between 2001-2004 20% 7% Patients' Personal Physcians Emergency Departments Specialists Outpatient Departments 42% 28% Source: Where Americans Get Acute Care? Increasingly, It’s Not at Their Doctor’s Office by Stephen R. Pitts, Emily R. Carrier, Eugene C. Rich, Arthur L. Kellerman Average Annual Frequency of Acute Care Visits from 2001-2004 Hospital Outpatient Department 25.1 Setting All Other Specialties 71.8 General Pediatrics 45.7 General Internal Medicine 36.2 General Family/Practice 77 Emergency Department 97.9 0 20 40 60 80 100 Millions Source: Where Americans Get Acute Care? Increasingly, It’s Not at Their Doctor’s Office by Stephen R. Pitts, Emily R. Carrier, Eugene C. Rich, Arthur L. Kellerman Average Annual Ambulatory Visits by Setting Type of Visit Millions of Visits Annually 20012004 Routine Follow-up visits/nonillness visits 0.0 Follow-up acute visits/postoperative visits 6.2 Acute care visits Total 97.9 104.1 Source: Where Americans Get Acute Care? Increasingly, It’s Not at Their Doctor’s Office by Stephen R. Pitts, Emily R. Carrier, Eugene C. Rich, Arthur L. Kellerman Emergency Department Visits Within 12 Months Among Adults 18 Years and Older by Race/Ethnicity Percent of adults with one or more emergency department visits Year Race/Ethnicity 1997 2000 2006 2007 19 19.4 20.1 19.6 Black or African American 25.9 26.5 25.6 26.3 Hispanic or Latino 19.2 18.3 17.3 18.2 American Indian/Alaska Native 24.8 30.3 21.1 26.7 Asian 11.6 13.6 13.6 11.9 White Source: CDC and the National Center for Health Statistics - Health, United States, 2009 Report, Table 89, available at http://www.cdc.gov/nchs/data/hus/hus09.pdf#089 Visits per 1,000 Population PA, MD and IL Hospital Emergency Room Visits Per 1,000 Population 2005-2008 480 460 Pennsylvania Maryland Illinois 440 420 400 380 Pennsylvania Maryland Illinois 2005 2006 2007 2008 434 386 393 450 410 398 464 407 394 478 403 399 Year Source: The Kaiser Family Foundation, statehealthfacts.org, Hospital Emergency Room Visits Per 1,000 Population 2005-2008, available at http://www.statehealthfacts.org/comparemaptable.jsp?yr=63&typ=1&ind=388&cat=8&sub=94 Freedom Riders: 1961 and the Struggle for Racial Justice Gospel Choirs: Psalms of Survival in an Alien Land Called Home Long Walk to Freedom: The Autobiography of Nelson Mandela Unnatural Causes • Is inequality making us sick? • A four hour documentary exploring racial and socioeconomic inequities in health • California Newsreel • www.unnaturalcauses.org Unnatural Causes: Video Trailer http://www.unnaturalcauses.org/video_clips_detail.php?res_id=80 Health Disparities Communities of Color are Disproportionately Affected What is a “Health Disparity?” Conceptual Issues • Inequality • Difference in condition, rank • Lack of equality as of opportunity, treatment, or status • Inequity – Unfair and unjust – Unnecessary and avoidable “Health Disparity” in Public Health – Operational Definition • Quantitative measures: rates, percents, means… • The Quantity that separates a group from a reference point on a particular measure of health • Calls attention to differences in health between groups regardless of cause • Can be measured in absolute or relative terms Population of the United States by Race & Hispanic Origin: 2008 & Projected 2050 % Percent of Total U.S. Population 100 Non-Hispanic White 90 African American 80 American Indian / Alaska Native 70 66 Asian 60 Hispanic/Latino 46 50 40 30 30 20 10 15 14 1.6 5.1 15 9.2 2 0 2008 2050 Source: U.S. Census Bureau, 2008 National Population Projections, August 14, 2008 http://www.census.gov/Press-Release/www/releases/archives/population/012496.html Racial and Ethnic Minority Populations • • • • • American Indian/Alaska Native (AI/AN) Asian American Black or African American Hispanic or Latino Native Hawaiian or Other Pacific Islander (NHOPI) Other Populations By . . . • • • • • • Socio-economic status Geography (urban or rural) Gender Age Disability status Risk status related to sex and gender Age-Adjusted Death Rate per 100,000 Persons 1200 1016.5 1000 798.8 800 785.3 663.4 590.7 600 440.2 400 200 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 300 271.3 Heart Disease Cancer Stroke 250 222.7 211.1 200 207.8 183.8 182.6 157.3 141.8 150 123.2 113.3110.5 122.8 100 65.2 50 46.6 44.7 34.8 38.6 35.7 0 All Races White African American American Indian/Alaska Native Asian/Pacific Islander Hispanic Age-Adjusted Death Rate per 100,000 Persons 50 46.9 45 41.5 40 33.6 35 30 25 24.6 22.5 20 16.6 15 10 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 24.8 25 20 15.2 15.6 15 14.7 14.5 10 7.6 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 19.4 20 15 10 5 4.7 4.2 2.7 2.2 0.6 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 25 22.6 20 13.9 15 10 9.0 9.2 7.7 5 3.6 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic 30 Age-Adjusted Cases per 100,000 Persons 25.8 25 23.4 20 15 9.3 10 8.4 6.0 5 0 0.8 1.1 Multi Racial non-Hispanic White non-Hispanic Black American Indian / Alaska Native (AI/AN) Asian American Hispanic/Latino Native Hawaiian & Other Pacific Islanders (NHOPI) Source: CDC, MMWR, March 21, 2008 / 57(11);281-285, Trends in TB, US, 2007, Table: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5711a2.htm Age-Adjusted Cases per 100,000 Persons 3 2.3 2 1.2 1.1 1.1 1 0 White non-Hispanic Black non-Hispanic Source: CDC MMWR, V57, SS2, March 21, 2008, p5. http://www.cdc.gov/mmwr/PDF/ss/ss5702.pdf Asian/Pacific Islander Hispanic/Latino Age-Adjusted Death Rate per 100,000 Persons 300 271.3 250 211.1 207.8 200 157.3 141.8 150 113.3 100 50 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 250 222.7 200 183.8 182.6 150 123.2 122.8 110.5 100 50 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 70 65.2 60 50 46.6 44.7 38.6 40 34.8 35.7 30 20 10 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 60 55 53.3 50 45 40 35 30 25 24.5 22.6 18.5 17.6 20 15 10 10.4 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 60 55 58.4 52.6 53.1 50 45 40 34.1 35 30 25 25.7 22.4 20 15 10 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 50 45 43.2 45.4 40 35 30.6 30 29.1 25 19.3 20 14.9 15 10 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 35 32.8 30 25 24.1 23.4 20 15.2 15 15.0 12.2 10 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 24.8 25 20 17.5 16.9 15 12.0 12.4 11.2 10 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Age-Adjusted Death Rate per 100,000 Persons 25 21.7 20.3 20.4 20.2 20 16.8 15.5 15 10 5 0 All Races White African American American Asian/Pacific Indian/Alaska Islander Native Hispanic Landmark: The Inside Story of America’s New Health Care Law and What it Means for Us All Patient Protection and Affordable Care Act of 2010 (PPACA): Advancing Health Equity for Racially and Ethnically Diverse Populations http://www.jointcenter.org/hpi/sites/all/fi les/PatientProtection_PREP_0.pdf The Lost Art of Healing: Practicing Compassion in Medicine Preventive Services Under the PPACA • SEC. 1001 - Providing Free Preventive Care. All new plans must cover certain preventive services such as mammograms and colonoscopies without charging a deductible, co-pay or coinsurance. Effective for health plan years beginning on or after September 23, 2010. • SEC. 4002 - Preventing Disease and Illness. A new $15 billion Prevention and Public Health Fund will invest in proven prevention and public health programs that can help keep Americans healthy – from smoking cessation to combating obesity. Funding begins in 2010. • SEC. 4103 - The law provides certain free preventive services, such as annual wellness visits and personalized prevention plans for seniors on Medicare. Effective January 1, 2011. • SEC. 4106 - Improving Preventive Health Coverage. To expand the number of Americans receiving preventive care, the law provides new funding to state Medicaid programs that choose to cover preventive services for patients at little or no cost. Effective January 1, 2013. Source: Healthcare.gov, http://www.healthcare.gov/law/about/order/byyear.html Interim Final Regulations (IFR) and Preventive Care • Section 1001 of the Affordable Care Act amending section 2713 of the PHS Act, along with a set of interim final regulations (issued by the Internal Revenue Service, DHHS, and the Department of Labor on July 19, 2010 to implement provisions of health care reform) require that a group health plan and a health insurance issuer offering group or individual health insurance coverage provide coverage for the recommended preventive services without cost-sharing requirements for: 1. Evidence-based items or services that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force (Task Force) with respect to the individual involved. 2. Immunizations for routine use in children, adolescents, and adults that have in effect a recommendation from the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention (Advisory Committee) with respect to the individual involved. IFR and Preventive Care Continued… 3. With respect to infants, children, and adolescents, evidenceinformed preventive care and screenings provided for in the comprehensive guidelines supported by the Health Resources and Services Administration (HRSA). 4. With respect to women, evidence-informed preventive care and screening provided for in comprehensive guidelines supported by HRSA (not otherwise addressed by the recommendations of the Task Force). The Department of HHS is developing these guidelines and expects to issue them no later than August 1, 2011. Examples of Grade A and B Recommendations of the United States Preventive Services Task Force Topic Text Grade The U.S. Preventive Services Task Force (USPSTF) recommends screening and behavioral counseling interventions to reduce alcohol misuse (go to Clinical Considerations) by adults, including pregnant women, in primary care settings. B The U.S. Preventive Services Task Force (USPSTF) recommends screening for high blood pressure in adults aged 18 and older. A The USPSTF recommends screening mammography for women with or without clinical breast examination (CBE), every 1-2 years for women aged 40 and older. B Screening for cholesterol abnormalities: men 35 and older The U.S. Preventive Services Task Force (USPSTF) strongly recommends screening men aged 35 and older for lipid disorders. A Screening for cholesterol abnormalities: men younger 35 a The USPSTF recommends screening men aged 20 to 35 for lipid disorders if they are at increased risk for coronary heart disease. B Screening and counseling to reduce alcohol misuse Screening for high blood pressure Screening for breast cancer (mammography) Source: Healthcare.gov, www.healthcare.gov/center/regulations/prevention/regs.html Consumer Assistance Programs under the PPACA • Section 1002 - States that apply can receive federal grants to help set up or expand independent offices to help consumers navigate the private health insurance system. • These programs will also collect data on the types of problems consumers have, and file reports with the U.S. Department of Health and Human Services to identify trouble spots that need further oversight. • Goal is to help consumers: – file complaints and appeals; – enroll in health coverage; – get educated about their rights and responsibilities in group health plans or individual health insurance policies. Source: Healthcare.gov, http://www.healthcare.gov/law/about/order/byyear.html At Hospitals, New Methods with a Focus on Diversity • Going beyond hiring interpreters and offering translated paperwork to improve care • Example; nurse tells Latino patients at diabetes nutrition classes to avoid white bread, but does not mention tortillas, a staple of their diet • Blood sugars levels remained high until she asked them to bring in samples of food they ate at home • Source: N.Y. Times, 9-6-10 Provisions of the Patient Protection and Affordable Care Act Expanding Community Health Centers • SEC. 10503 – Community Health Centers and the National Health Service Corps Fund; “to provide for expanded and sustained national investment in community health centers” – appropriates new funding between fiscal years 2011-2015 $7 billion for services (to be increased to $11 billion under the President’s new proposal) $1.5 billion for the construction and renovation of CHCs $1.5 billion for the National Health Service Corps (which will place approximately 15,000 primary care providers in provider-short communities) Source: Text of H.R. 3590: Patient Protection and Affordable Care Act, available at http://www.govtrack.us/congress/billtext.xpd?bill=h111-3590 Provisions of the Patient Protection and Affordable Care Act Expanding Community Health Centers Continued… • SEC. 5508- Increasing Teaching Capacity; authorizes a new Title VII grant program for the development of residency programs at health centers and creates a new Title III program that provides payments to community-based entities that operate teaching programs, appropriate $125 million from 2010-2012 to carry this out • SEC. 5601 – Spending for Federally Qualified Health Centers $2.9 billion 2009-2010 $3.9 billion 2010-2011 $4.9 billion 2011-2012 $6.4 billion 2012-2013 $7.3 billion 2013-2014 $8.3 billion 2014-2015 Source: Text of H.R. 3590: Patient Protection and Affordable Care Act, available at http://www.govtrack.us/congress/billtext.xpd?bill=h111-3590 KEY PROVISIONS OF THE PATIENT PROTECTION AND AFFORDABLE CARE ACT CONTINUED… • SEC. 3501. HEALTH CARE DELIVERY SYSTEM RESEARCH: establishing the functions of the Center for Quality Improvement and Patient Safety of the Agency for Healthcare Research and Quality, among them is to make the research findings of the Center available to the public through multiple media and appropriate formats to reflect the varying needs of health care providers and consumers and diverse levels of health literacy KEY PROVISIONS OF THE PATIENT PROTECTION AND AFFORDABLE CARE ACT (H.R. 3590) • SEC. 5002. DEFINTIONS: Health Literacy (the degree to which an individual has the capacity to obtain, communicate, process, and understand health information and services in order to make appropriate health decisions) • SEC. 5307. CULTURAL COMPETENCY, PREVENTION, AND PUBLIC HEALTH AND INDIVIDUALS WITH DISABILITIES TRAINING: emphasizing collaboration between several groups (e.g. community-based organizations, licensing and accreditation schools, health professional societies) to adopt culturally competent measures • SEC. 5301. TRAINING IN FAMILY MEDICINE, GENERAL INTERNAL MEDICINE, GENERAL PEDIATRICS, AND PHYSICIAN ASSISTANTSHIP: preference and priority in awarding grants or contracts to qualified applicant accredited schools of medicine will go to those who provide training in culturally competency and health literacy (as one of other considerations) Cultural Competency Statutes • California • New Jersey • Massachusetts CULTURAL COMPETENCEY ACCREDITATION STANDARDS • • • • Medical Schools Nursing Schools Continuing Medical Education Continuing Nursing Education Human Experimentation • Tuskegee Syphilis Study • Jewish Chronic Hospital Case • Johns Hopkins Lead Study case: Grimes v. Kenney Kreiger Institute, Inc. 782 A. 2d 807 (Md. 2001)(court holds researchers have special duty to children and parents cannot consent to non-therapeutic research that poses a risk of harm to their children PROBLEM FOR GROUP DISCUSSION • 70 year old African American Male refuses to see orthopedic surgeon, stating: “I do not trust white doctors and I believe that whatever happens now is God’s will. I have led a good life.” Summary of Statutes and Accreditation Standards • Informative source: https://www.thinkculturalhealth.hhs.gov/ LIAISON COMMITTEE ON MEDICAL EDUCATION • STANDARDS for Accreditation of Medical Education Programs Leading to the M.D. Degree • ED-21 “must demonstrate an understanding of the manner in which people of diverse cultures and belief systems perceive health and illness and respond to various symptoms, diseases and treatments.” • ED 22 “must learn to recognize and appropriated address gender and cultural biases in themselves, in others, and in the process of health care delivery” • http://www.lcme.org/functions2010jun.pdf (last visited Aug. 27, 2010). The Importance of Poor Health Literacy Poor health literacy is a “stronger predictor of a person’s health than age, income, employment status, education level, and race.” -Report on the Council of Scientific Affairs, Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association, JAMA, Feb 10, 1999). Health Literacy: A Prescription to End Confusion EXTENT OF LOW HEALTH LITERACY • 90 million U.S. adults have low health literacy (nearly half of all U.S. adults) • The average annual health care costs of persons with very low literacy (described as reading at the grade two level or below) may be four times greater than for the general population • 75% of U.S. persons with chronic physical or mental health issues are in the limited literacy category • One study of Medicare enrollees found that 34 percent of English speakers and 54 percent of Spanish speakers had inadequate or marginal health literacy • A study of patients 60 years and older at a public hospital found that 81 percent could not read and understand basic materials such as prescription labels and appointments Note: Healthy People 2010 defines Health Literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” Sources: Healthy People 2010 (Chapter 11), Health Communication, U.S. Department of Health and Human Services; National Network of Libraries of Medicine, Health Literacy http://nnlm.gov/outreach/consumer/hlthlit.html PAYING FOR THE COST OF LOW HEALTH LITERACY (1998 STUDY) Low Health Literacy Leads to $73 Billion in Health Care Expenditures by Various Paye es $3.4 Medicare Employers $7.6 $28.3 $10.3 Patients Medicaid Other Public Other Private $11.5 Dollars in Billions $12.1 Source: National Academy on an Aging Society, Health Literacy Fact Sheet: Low Health Literacy Skills Increase Annual Health Care Expenditures by $73 Billion http://www.agingsociety.org/agingsociety/publications/fact/fact_low.html THE 2003 NATIONAL ASSESMENT OF ADULT LITERACY (NAAL) SURVEY • First large-scale national literacy study to have a component specifically designed to measure health literacy in adults and provide a separate health literacy score • Conducted with a nationally representative sample of 19,000 adults aged between 16 years and older • Adult performance measured on a range of healthrelated tasks (e.g. understanding dosing instructions for medication) • The NAAL definition of functional health literacy: the ability of U.S. adults to use printed and written health related information in English to function in society, achieve one’s goals, and to develop one’s knowledge and potential (does not measure the ability to communicate orally) Source: Sheida White, Assessing the Nation’s Health Literacy: Key Concepts and Findings of the National Assessment of Adult Literacy (2008) NAAL FINDING OF PERCENTAGE OF ADULTS AT EACH HEALTH LITERACY LEVEL BY RACE/ETHNICITY Multiracial 9 Race/Ethnicity American Indian/Alaskan Native 28 25 Asian/Pacific Islander 13 0% 9 7 52 25 19 18 31 34 20% 3 45 18 24 African American Below Basic Basic Intermediate Proficient 23 41 Hispanic White 59 41 58 40% 4 60% 2 14 80% 100% Percentage Source: Sheida White, Assessing the Nation’s Health Literacy: Key Concepts and Findings of the National Assessment of Adult Literacy (2008) KEY PROVISIONS OF THE PATIENT PROTECTION AND AFFORDABLE CARE ACT (H.R. 3590) • SEC. 5002. DEFINTIONS: Health Literacy (the degree to which an individual has the capacity to obtain, communicate, process, and understand health information and services in order to make appropriate health decisions) • SEC. 5307. CULTURAL COMPETENCY, PREVENTION, AND PUBLIC HEALTH AND INDIVIDUALS WITH DISABILITIES TRAINING: emphasizing collaboration between several groups (e.g. community-based organizations, licensing and accreditation schools, health professional societies) to adopt culturally competent measures • SEC. 5301. TRAINING IN FAMILY MEDICINE, GENERAL INTERNAL MEDICINE, GENERAL PEDIATRICS, AND PHYSICIAN ASSISTANTSHIP: preference and priority in awarding grants or contracts to qualified applicant accredited schools of medicine will go to those who provide training in culturally competency and health literacy (as one of other considerations) KEY PROVISIONS OF THE PATIENT PROTECTION AND AFFORDABLE CARE ACT CONTINUED… • SEC. 3501. HEALTH CARE DELIVERY SYSTEM RESEARCH: establishing the functions of the Center for Quality Improvement and Patient Safety of the Agency for Healthcare Research and Quality, among them is to make the research findings of the Center available to the public through multiple media and appropriate formats to reflect the varying needs of health care providers and consumers and diverse levels of health literacy KEY PROVISIONS of the PATIENT PROTECTION AND AFFORDABLE CARE ACT CONTINUED… • SEC. 3506. PROGRAM TO FACILITATE SHARED DECISIONMAKING: REQUIREMENTS FOR PATIENT DECISION AIDS - Patient decision aids developed and produced pursuant to a grant or contract shall present evidence about the risks and benefits of treatment options in a form and manner that is age-appropriate and can be adapted for patients, caregivers, and authorized representatives from a variety of cultural and educational backgrounds to reflect the varying needs of consumers and diverse levels of health literacy TITLE VI OF THE CIVIL RIGHTS ACT OF 1964 “No person in the United States shall, on the ground of race, color, or national origin, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity receiving federal financial assistance.” –Lau v. Nichols (1974) - the Supreme Court interprets language discrimination as equivalent to national origin discrimination Title VI of the Civil Rights Act of 1964 Alexander v. Sandoval (2001) – a class action suit against the Alabama Department of Public Safety for requiring that all state driver’s license tests be administered in English only; a divided Supreme Court held private individual actions to enforce the disparate impact regulations promulgated under Title VI are prohibited • A huge blow to equitable health care by undermining the ability to address systemic discrimination that takes place in the health care system Health Insurance Coverage Private Public Uninsured 80 70 60 50 40 30 20 10 0 White Black Hispanic/Latino Asian/Pacific Islander Other race/Multiple Races Health Insurance Coverage and Population Characteristics-all Ages, Medical Expenditure Panel Survey Home, http://www.meps.ahrq.gov/mepsweb/data_stats/summ_tables/hc/hlth_insr/2009/t1_a09.htm. Uninsured Persons and Uninsured Rate Between 1987-2009 50.7 million 16.7% Source: New England Journal of Medicine, Health Policy and Reform, Data Watch Sept. 22, 2010; U.S. Census Bureau, Current Population Survey, 1988-2010 Annual Social and Economic Supplements Uninsured Rates for the Nonelderly by Race/Ethnicity Individual State Rates (2008) United States (2008) 35 32.2 25 Percentage Percentage 30 20.6 20 18.5 12.7 15 10 5 50 45 40 35 30 25 20 15 10 5 0 45.2 25.9 19.7 18.9 14 16 10.4 9.3 Pennsylvania Maryland 0 Other White Black Race/Ethnicity 12 11.4 11 Illinois State Hispanic Other White Black Hispanic Note: 1.Nonelderly = 0-64 years of age, 2.Insufficent data available for PA’s uninsured nonelderly ‘other’ category Source: The Kaiser Family Foundation, statehealthfacts.org, http://www.statehealthfacts.org/comparetable.jsp?ind=143&cat=3 Distribution of Nonelderly Uninsured by Race/Ethnicity (2008) State Maryland 5.5% 35% Pennsylvania 33.3% 13% 9.5% 73.9% Illinois 4.8% 0% 47.9% 20% 40% 26.2% 20.8% 60% Other White Black Hispanic 26.5% 80% 100% Percentage Note: 1. Nonelderly = ages 0-64 years of age 2. Insufficient data for Pennsylvania’s ‘other’ race/ethnicity category of nonelderly uninsured 3. Persons of Hispanic origin may be of any race; all other racial/ethnic groups are non-Hispanic Source: The Kaiser Family Foundation, statehealthfacts.org, http://www.statehealthfacts.org/comparebar.jsp?ind=138&cat=3 HEALTH CARE DECISION-MAKING: LEGAL RIGHTS AND DUTIES • • • • PATIENT AUTONOMY PHYSICIAN AUTHORITY THIRD PARTY PAYER POWER PATIENT TRUST REALITY OF DECSIONMAKING • PROVIDERS SET STANDARD OF CARE • INSURERS SET STANDARD OF CARE • PATIENT AUTNTOMONY LIMITED BY ACCESS AND KNOWLEDGE PATIENTS’ KNOWLEDGE AND VALUES • HEALTH LITERACY • VALUES: CULTURAL, RELIGIOUS ECONOMIC • INFLUENCE OF FAMILY • INFLUENCE OF CHURCH • INFLUENCE OF MEDIA • INFLUENCE OF GOVERNMENT Three Important Books • James Jones, Bad Blood • Anne Fadiman, The Spirit Catches You and You Fall Down • Rebecca Skloot, The Immortal Life of Henrietta Lacks LAW OF INFORMED CONSENT • Canterbury v. Spence, 464 F.2d 772 (D. C. Cir. 1972) Patient has a right to know risks, benefits alternatives • Autonomy: Patient has a right to make decisions others consider irrational or unreasonable INFORMED REFUSAL • • • • Truman v. Thomas, 611 P. 2d 902 (Cal. 1980) Patient refuses pap smear Patient dies from cervical cancer Family sues patient’s family doctor who recommended pap smear but did not explain risk of not having the test done • Court rules doctor had duty to advise of risk of harm associated with refusing test Key Sources • Institute of Medicine Report – Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (2002), Edited by Brian Smedley, Adrienne Stith, and Alan Nelson • CDC Health Disparities and Inequalities Report 2011, MMWR, Vol 60 available at http://www.cdc.gov/mmwr/pdf/other/su6001.pdf • Institute of Medicine – Health Literacy: A Prescription to End Confusion (2004) • Patient Protection and Affordable Care Act, a study of key provisions available at http://www.jointcenter.org/hpi/sites/all/files/PatientProtect ion_PREP_0.pdf • The Kaiser Family Foundation, www.statehealthfacts.org