Fourth Class Powerpoint Slides
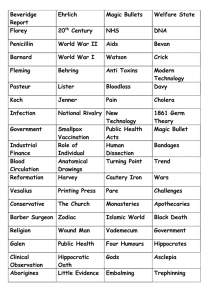
advertisement

PA 574: Health Systems Organization Session 4 – April 24, 2013 Collecting resources Distributing Resources Both should seek to support and not driving the system – i.e. reflect system goals, not create them… Goals: • Protect against financial risk (income and/or health based) • Provide health services to populations Purpose • Risk: Economic fairness • Services: Population health Mechanisms (generally) • Risk: More individual/market justice/private good • Services: More population/social justice/social good Broad public taxes (income) • Generally progressive and least related to health states (risk) Specific public taxes (wages) • Less progressive, may have some relation to health states Specific private “taxes” (insurance premiums) • Not progressive, tied to health states (groups or individual) Direct payment (out-of-pocket) • Regressive(?), directly linked to health states Any of these can be mixed together… Means of collecting resources can be used to define system types • Finance aligns with and supports system goals and underlying structure • Direction of determinism is important – support or driver? Universalism as important goal • Universalism requires “fair” collection policy • Guard against selection – avoiding unhealthy or letting people use without contributing Beveridge Classic – Broad public tax based collection tied to public run universal system Beveridge Neo-Classic – Broad public tax based collection disbursed through private universal system Bismark Classic – Specific public tax based collection run through private universal collection and disbursement systems Bismark Neo-Classic – Specific public and private tax based collection run through private universal collection and disbursement systems Mixed systems – combinations of above “Not-so-classics” – versions of above, or mixed but not universal and usualy very limited Beveridge Classic – Broad public tax based collection tied to public run universal system Beveridge Neo-Classic – Broad public tax based collection disbursed through private universal system Bismark Classic – Specific public tax based collection run through private universal collection and disbursement systems Bismark Neo-Classic – Specific public and private tax based collection run through private universal collection and disbursement systems Mixed systems – combinations of above “Not-so-classics” – versions of above, or mixed but not universal and usually very limited Beveridge Classic – British NHS, Norway/Sweden(?) Beveridge Neo-Classic – France, Canada, New Zealand Bismark Classic – Germany, Austria Bismark Neo-Classic – Netherlands, Switzerland Mixed systems – US, Australia “Not-so-classics” – Many developing countries and parts of US system (market?) Beveridge Classic – VA Beveridge Neo-Classic – Medicaid Bismark Classic – Medicare Bismark Neo-Classic – Most large businesses, PPACA “Not-so-classic” – US individual/small business market before PPACA? Universal coverage through: • Individual mandate to purchase insurance • Tax based support for insurance purchase up to 400% FPL • Works through existing private insurers/providers Looks mostly like Bismarck Neo-classic model (as would Massachusetts) Vermont looking to do Beveridge NeoClassic Overall upgrade for individual/small business insurance market from “not-soclassic”? Not much discernible difference All (but not-so-classics) can accommodate universal coverage No clear differences in Triple Aim outcomes • France has been rated best and its Beveridge Neo-classic • Use of private provider systems seems to have some edge in patient experience of care • Single payer (Beveridge) seems to have slight edge in cost Slight differences in approaches regarding fairness/equity • Beveridge really only income based (general taxes, little direct pay • Bismarck is generally income & health status based, with more direct payment Bismarck may be more administratively complex • Example: Health insurance exchanges under PPACA – price of individual satisfaction(?) Two considerations: • “Fair” payment to provider • Best “value” to payer/consumer History: • “Natural”/”Open” approach to reimbursement • “Fair” payment = pay providers based on what they decide to do (“open”) and what they see as “fair”. • Best “value” determined by “natural” system of professional ethics. • Cost inflation with limited value challenges this • How to create reimbursement that embraces Triple Aim? “Piecemeal” Payment – Fee-for-Service: • Payments for increments of treatment process • Based on use of “structure” – process piece done by whom/where • Retrospective – based on what was done Examples: • “Natural” – Usual and Customary Charges (UCC), market/contract based fees • “Rational” – Resource Based Relative Value Units (RBRVU) – establish fee based on constructed average efficient provider/practice financials Medicare did RBRVUs – raised primary care fees and lowered specialty fees Episode or Case Rate Payment: • Payments for discrete but locally complete pieces of care • Combines pieces of treatment into “whole” cases or episodes of care • Prospective – based on what you should do in specific case/episode Examples: • “Natural” – place/process specific – Diagnostic Related Groups (DRGs) for inpatient care, Resource Utilization Groups (RUGs) for nursing home care, Pre-natal global fees – single fee for all pre-natal care • “Rational” – Place/Process spanning – “true” episode – “bundled” payments – single fee for knee/hip replacement that includes pre- and post-surgical care Global Budgets/Capitation Payments • Payments for comprehensive care of specific population • Payment per individual whether they use services or not (capitation), sums to total payment (global budget) • Prospective – based on expectation of population/individual outcomes – not specifically what is done Examples: • “Natural” – personal health specific – private insurance premiums • “Rational” – community health based/income neutral – “universal” (whole group) coverage – large business model, Medicare/Medicaid, managed care/ACOs/CCOs Achieving Triple Aim requires reimbursement that embraces, incentivizes, and supports all three aims • Fee-for-service worst – doing more means more money regardless of value • Case/episode better – doing more likely is better • Global budget best – doing more (or less) isn’t the issue – doing better is… But..organization/system & payment interrelated, so must be aligned: • Need orgs that can “handle” new, better payment • • • • methods Need new data and measurement effort – identifying episodes, populations, and actual outcomes Need numbers – larger orgs – prospective payment based on risk Need boundary spanning orgs/relationships Whole system perspective – how one thing effects other things across system (“true” value assessment) This is where we are going – or trying to – Triple Aim orgs/systems supported by appropriate financing and reimbursement

![1927.] Obituaries 181 ALBERT JEREMIAH BEVERIDGE Albert](http://s3.studylib.net/store/data/008265495_1-dbb1462976881bcdd0f4f3f4ff281742-300x300.png)