Site selection
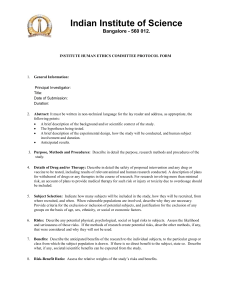
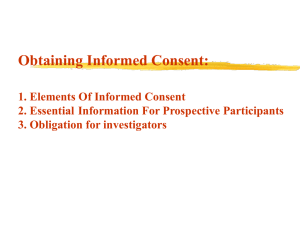
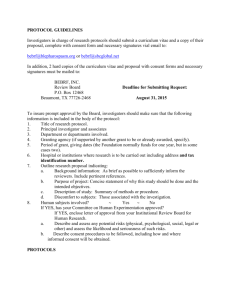
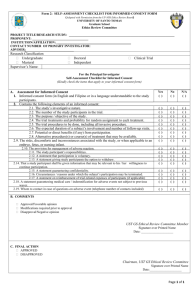
advertisement

Site Selection, Training, and Surveillance IMMPACT XVIII Richard Malamut, MD ICH GCP - The Most Important Requirement for a Clinical Study The 1996 International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) guidance on good clinical practice (ICH E6) The rights, safety, and wellbeing of the trial subjects are the most important considerations and should prevail over interests of science and society. 2 Clinical Study Time Points and Activities Study start – up Study conducted Protocol Sign Off First Patient In Study Design Clinical Study Report Last Patient Last Visit Last Patient In First Patient Screened Study closure Data Base Lock Patient Recruitment Statistical Analysis Plan Site Management (e.g. Study Visits) Vendor Selection KOM Informed Consent Medical Monitoring Inv. Meetings Countries and Sites Selection Site Activation Regulatory Submissions Clinical DB Creation Data Collection & Cleaning Site Audits Drug Supply Study Timelines Management Study Budget Management Study Documentation- TMF Vendor Oversight Inspection Readiness Data Analysis and report SITE SELECTION 4 Country Selection and Feasibility The process is led by the operational manager while involving various functions such as Commercial (country selection only based upon marketing plan), Clinical, regulatory and clinical supply Sponsor/CRO previous experience play a key role Quality of data from prior studies Compliance with study requirements in prior studies Success in recruiting high-quality patients in prior studies Disease indication prevalence Marketing authorization may depend upon the participation of that country in a global study The country list is impacted by protocol requirements (disease prevalence, placebo allowance, comparator not approved, standard-of-care, study procedures, etc.) Site selection and Feasibility Sponsor/CRO previous experience with the site play a key role Quality of data from prior studies Expert in the disease area Speed and facility of study start-up activities (e.g. IRB approval, contract finalization) Compliance with study requirements in prior studies Success in recruiting high-quality patients in prior studies Less common or more complex disease indications may require specialist sites with access to those patients (e.g., erythromelalgia) or with special skills in carrying out protocol requirements (e.g., NCS/QST) Site selection and Feasibility The proposed sites review the study protocol details under CDA and are asked to provide their willingness and capabilities to perform the study (man power, facility, recruitment potential, experience in clinical trials, participation in competitive studies) and any potential concerns they envision Sites found to be suitable for the study based on the above will be visited (Pre Site Selection Visit= PSSV) to confirm sites qualification to conduct the study properly If the Investigator has been previously inspected by the FDA or other government agency, confirm that any issues were addressed and resolved in a timely manner Site selection and Feasibility Compare site list with the following data lists and eliminate those listed from consideration for a Teva-sponsored study How can we do better—future research questions? Site selection Academic sites vs research sites (high quality vs high recruitment?) The lure of “fast-recruiting” countries—is quality maintained? If clinical study experience matters, how do we identify and encourage our future high-quality sites? What is the impact of recruitment speed and quantity upon study results? 9 TRAINING 10 Study Team Training Provide appropriate training to the study team (which includes Vendors, Sponsor functions, and study site personnel) Investigators’ Meeting GCP requirement ( Phase II-IV) The purpose of the Investigators’ Meeting is to train the team on the study protocol and processes Includes eligibility criteria, study procedures, Informed Consent process, safety reporting, Source Documentation, Investigator responsibilities, Site File Now may be a virtual IM via webex with multiple e-trainings occurring both before and after the IM Conduct periodic team meetings after IM (internal ,with vendors, and as needed with study site personnel) The Role of the Principal Investigator (PI) Ensuring that a clinical investigation is conducted according to the signed investigator statement for clinical investigations of drugs, the investigational plan, and applicable regulations Protecting the rights, safety, and welfare of subjects under the investigator’s care Controlling drugs, biological products, and devices under investigation Personally conducts or supervises the investigation May delegate tasks to appropriate members but is responsible for providing adequate supervision The investigator is accountable for regulatory violations resulting from failure to adequately supervise the conduct of the clinical study 12 Site Initiation Visit (SIV) SIV must occur prior to the first patient enrolment at site Ensure all regulatory documents are available and filed Ensure understanding of the study protocol, investigator informed consent, Investigator Brochure, Investigational Medicinal Product, etc. Prepare, train and set up site to conduct the study (equipment, internet connection, study drug storage capabilities, lab kits, etc.) Resolve any outstanding issues regarding site readiness (training, equipment needs, recruitment projection and obstacles, missing documents etc.) Informed Consent Training Informed Consent Process Informed consent is a process by which a subject voluntarily confirms his or her willingness to participate in the study The informed consent process is documented in an informed consent form (ICF). During the informed consent process, the subject is informed of all aspects of the study (study procedures, their purposes, risks and anticipated benefits) in a face-to-face discussion with the investigator The subject (or a legally acceptable representative) must sign and date the ICF before any study-related procedures are performed Many sponsors are now attempting to standardized the informed consent process to avoid introduction of potential bias by the PI or coordinator which may impact study results How can we do better—future research questions? Training What is the relative involvement of PIs and coordinators in study conduct? Is there any measurable difference in study conduct between F2F and virtual IM Is attendance at an investigator meeting sufficient to demonstrate study conduct proficiency and familiarity with the specific protocol? Should there be a mandatory national or international certification in clinical study conduct? Should we standardize the informed consent process across all sites and all studies? 15 STUDY SURVEILLANCE 16 Interim Monitoring Visits GCP requirement though sponsors have flexibility as to process Conducted by the monitor (CRA) who is the primary point of contact between the site and the sponsor Interim monitoring visits are conducted throughout the study- frequency is determined according to patients visit schedule, site recruitment and performance Preparation for internal QA and inspection audits with review of identified deficiencies Interim Monitoring Visits The purpose of the monitoring visit is to verify that Reported trial data is accurate, complete and verifiable from the source The conduct of the trial is in compliance with the protocol/amendments, GCP and regulatory requirements Proper study drug accountability, storage condition according to the protocol and temperature conditions Safety events are reported within the required timelines and via the appropriate channels Protocol violations are identified and reported as per local requirements Re-training is provided upon need Assist the sites in query resolution Source Documents Patient medical file= Source Document The medical file contains the patient’s medical history, all study visits summary, laboratory results (signed by the Inv.), ECG strips e-Source becoming more prevalent Source Data Verification (SDV) Comparing the data from the medical files (source) to the CRF and make sure all relevant information is accurately captured Crucial process to ensure proper patient diagnosis and potential exclusions due to unknown medical history Study site monitor responsibility to conduct the SDV either during site visit or remotely Teva currently follow 100% SDV policy—is this standard across sponsors? Should it be? Vendor Oversight Ongoing Training Monitoring Periodic Team Meetings: • • Vendors’ Management Share information and updates Discuss Study Related Issues, Global or country specific Financial Management Sponsor’s Oversight Audits Visits Vendor Oversight Global Outsourcing Requires Greater Sponsor Scrutiny While the idea to forge strategic partnerships to gain greater efficiencies is a growing trend, Sponsors need to be aware of the risks and take a more proactive role to ensure quality and compliance FDA warning letters (Sanofi-Aventis Oct 2007, J&J Aug 2009, ICON Nov 2009, Pfizer 2010 ) have made it very clear that Sponsors need to systematically evaluate and monitor their vendor’s activities throughout the course of outsourced clinical trials Teva implemented oversight activities within the regional vendor oversight model which applies to all Teva-sponsored studies from phase I to IV. The extent of oversight activities is outlined in the study-specific Vendor Management Plan (VMP) 22 Vendor Oversight Sponsor oversight activities include: Country and site selection and approval Review and approval of country and site-specific Informed Consent Forms (ICFs) Conduct of oversight visits Review of monitoring visit reports Review of protocol violations and deviations Monitoring the follow-up of Quality Assurance (QA) audit and inspection findings 23 Study Documentation- Trial Master File (TMF) Study Documentation- Trial Master File (TMF) those essential documents that individually and collectively permit the evaluation of the conduct of a trial and the quality of the data produced These documents serve to demonstrate the compliance of the investigator/site, CRO and the Sponsor with the standards of GCP and with all applicable regulatory requirements Documents that pre-define how the study will be conducted Protocols and amendments, regulatory approvals, study plans ICFs Study Plans Data collected during the study • • • Patient / Subject data Safety-related data Meeting minutes Summaries and analysis of the results Evidence of qualification to be part of the study and compliance with regulations and procedures • • • • Sponsor personnel Vendors (CROs and Laboratories) Physicians / Investigators and their personnel Investigational product Database Lock Ensure all outstanding issues are resolved (queries answered, lab samples accounted for and analyzed, serious adverse events reconciled, etc.) Ensure all final study documents are uploaded to the TMF and required trackers are complete Ensure posting of the updated study operational information and the study results in the appropriate registries MEDICAL SURVEILLANCE 27 Clinical Study Monitoring Safety monitoring Efficacy monitoring Clinical - Operational input Manage DMC and SC • Medical Monitoring during a study is a key study success factor focusing on 2 of the most important aspects of a trial: • Maintaining safety of participants • Assuring that high quality Safety and Efficacy Data is collected to support the regulatory application of the product • Requires a collaborative effort from the entire study team 28 The Clinical Study Monitoring Team Medical Monitor (MM) Outsourced role (in most cases) Responsible for ongoing medical monitoring of the trial Direct contact with sites (queries, mails, phone) Clinical Study Physician (CSP) In-house role Responsible and accountable for medical decisions and safety including -Issues escalated by MM -Oversight of MM activities -Trend analysis and benchmark comparison -DMC preparation and presentation 29 Medical Monitoring Plan Created jointly by CSP and Medical Monitor Describes the scope of medical monitoring during the trial e.g: Eligibility questions from sites SAE reports Medical queries Handling of alerts: Lab, ECG, disallowed medications Protocol violations Review of periodic reports 30 Clinical Study Medical Monitoringl | Confidential Safety Medical Monitoring Individual Patient Safety Track, review and query safety events - SAEs - AEs of interest - Lab and ECG panic alerts - Pregnancy - Other study specific measures - Continued Eligibility questions Population Trend Safety Analysis SAEs Abnormal Labs Discontinuations 31 Periodic Reports (PR) Ongoing disallowed medications Potentially Clinically Significant labs (e.g., liver function tests) New AEs of interest Cumulative number of events of interest How many cases of disallowed medications taken? How many AEs of interest thus far Protocol violation trends Early Termination reasons Suspicious medical history ( violation of inclusion/exclusion criteria?) 32 Clinical Study Medical Monitoringl | Confidential Medical Center Review The Institutional Review Board (IRB) or Ethics Committee (EC) is composed of various individuals that are knowledgeable in the process of clinical research and the regulations that surround it. This group of non-scientific and scientific experts comes together to review all documentation on a proposed study to determine if it is safe and ethical In some countries several sites may be associated under one central ethical committee During the review process questions, further clarifications and additional information both from the national level as well as the medical center level are addressed promptly Data Monitoring Committee & Clin Steering Committee The DMC is composed of independent physicians with expertise in the relevant therapeutic field and other relevant experts, such as a statistician in order to monitor the overall safety of the study patients. The DMC will receive safety data periodically. They will have the right to recommend discontinuation of the study for safety reasons The CSC is compose of a group of experts contributing to the planning of the study protocol, involved in discussions around patients’ eligibility Not all studies include a DMC or CSC 34 How can we do better—future research questions? Surveillance Should source document verification be a mandatory requirement? How do we ensure proficiency of medical monitors? DMC’s primarily evaluate patient safety. Is there a role for an independent committee that monitors study conduct? 35