Lessons Learned from a CIT Call Gone Bad
advertisement
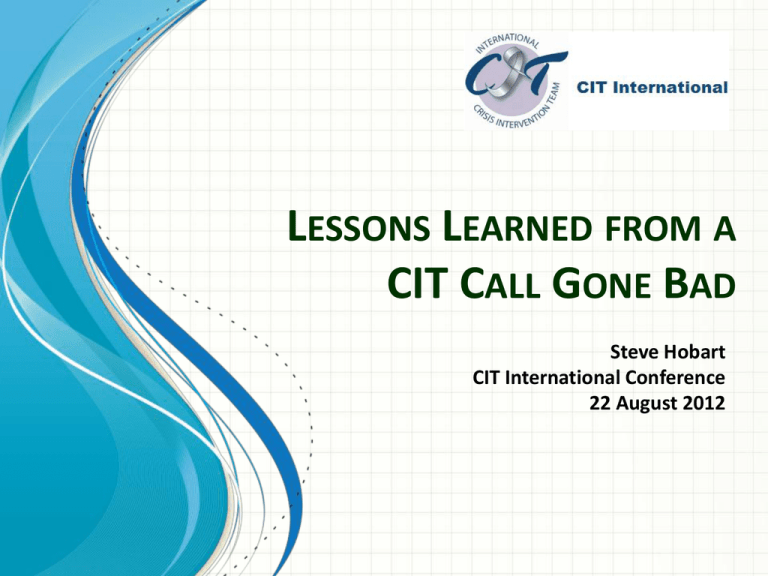
LESSONS LEARNED FROM A CIT CALL GONE BAD Steve Hobart CIT International Conference 22 August 2012 Outline/Agenda Introduction The CIT Call Lessons Learned For patients, caregivers and advocates For the mental health professional community For those who respond to calls for CIT service Workshop: Refining of Lessons Learned Introduction Talk is dedicated to the memory of my son, Aaron Hobart. While in the throes of a mental health crisis, Aaron was killed by a confused police officer who claims to have feared for his life in his encounter with Aaron. Talk is motivated by a desire to prevent similar tragedies. For the purposes of this workshop, the “CIT call” is a request for crisis intervention team assistance from a caregiver on behalf of a loved one having a mental health crisis. Brief Bio of Aaron (1) Born in 1989. Died at age 19. Minor birth complications. Tended to over-focus on things. Label of Aspberger Syndrome. IQ = 129 Legomaniac: aspired to be an architect Sensitized to poverty and injustice on mission trip to Mexico Brief Bio of Aaron (2) Held jobs at Whataburger, YMCA Lifeguard at church retreats Poet, Musician and “Metaphysician” The CIT Call The Call for a CIT Officer (1) Slightly edited transcript Dispatcher: … 911. What’s your emergency? Pam Hobart: I have a son that needs to be taken … he’s becoming very violent … I need a CIT officer. D: Where’s this at? What’s your address? PH: 12127 Aspen Lane D: What’s he doing? PH: … um … Well he’s been … um … he’s deteriorating … he’s becoming delusional … um … he’s not hurting anyone but … he needs to be in a hospital. He needs medication. (…) D: Where’s he at now? Is he at the house? PH: He’s in our home. Yes. … My husband’s here. D: OK. I’m going to send an officer out there. The Call for a CIT Officer (2) Slightly edited transcript PH: And he’ll be able to help us to transport him? D: Yes. PH: OK. Thank you. … How long will that be? D: Depends on traffic PH: Oh, OK. Thank you very much. [End call #1] (Call #2, about 2 minutes later) D: Ms. Hobart. … This is J__ with the Police department. How old is your son? PH: 19 D: OK. We have officers on the way. They just wanted to know that. The Call for a CIT Officer (3) Slightly edited transcript PH: OK. What’s the procedure? D: They’ll have to explain that to you when they get there. Um … they were just asking me a couple of questions while they were still on their way out there. PH: Sure. Sure. OK. D: Alright? No problem. Is he still in his room? PH: Yes. My husband’s in there with him, but he’s becoming more and more belligerent and … um … D: OK. Your husband’s in the room with him now? PH: Yes. D: OK. I’ll let them know about this information. PH: OK. Thank you. [End call #2] The Call for a CIT Officer (4) Slightly edited transcript (Call #3, about 1 minute later) D: Ms. Hobart? … This is J__ again. Are there any weapons in his room or anything? Does he have any? PH: No, no. He’s got a drum set in his room. D: OK. He’s not under the influence, is he? PH: No. D: OK. These are just … a couple of questions the officers were asking. PH: We just want to transport him as soon as possible. D: Has he done this before? PH: He was hospitalized a year and a half ago, but that was something where he was driving at night. He took one of our cars and was stopped for reckless driving. D: OK. Well, they’re almost there. PH: Well, Thank you. [End call #3] Record from Officer’s Dash-Cam Audio 15:07:40-43 Officer: “Tell RP to step outside” 15:08:00-03 (sound of door opening) PH: “Come in?” 15:08:09-12 PH: “You’re with the police?” Officer: “Yes.” 15:08:12-15 (More talk, words not distinct on radio recording. Recollection was PH: “I’m glad you’re here.”) 15:08:15 Start of “Stop … Stop” (both PH and Officer, according to statements) 5 seconds of scuffle 15:08:20-22 Six shots fired. 15:08:23-24 Officer: <Cursing> 15:08:25 Officer: “224 shots fired” Nobody wanted the call to end this way. What went wrong? The Call for a CIT Officer (Hindsight 1) Slightly edited transcript Dispatcher: … 911. What’s your emergency? Pam Hobart: I have a son that needs to be taken … he’s becoming very violent … I need a CIT officer. D: Where’s this at? What’s your address? PH: 12127 Aspen Lane D: What’s he doing? PH: … um … Well he’s been … um … he’s deteriorating … he’s becoming delusional … um … he’s not hurting anyone but … he needs to be in a hospital. He needs medication. (…) D: Where’s he at now? Is he at the house? PH: He’s in our home. Yes. … My husband’s here. D: OK. I’m going to send an officer out there. The Call for a CIT Officer (Hindsight 2) Slightly edited transcript PH: And he’ll be able to help us to transport him? D: Yes. PH: OK. Thank you. … How long will that be? D: Depends on traffic PH: Oh, OK. Thank you very much. [End call #1] (Call #2, about 2 minutes later) D: Ms. Hobart. … This is J__ with the Police department. How old is your son? PH: 19 D: OK. We have officers on the way. They just wanted to know that. The Call for a CIT Officer (Hindsight 3) Slightly edited transcript PH: OK. What’s the procedure? D: They’ll have to explain that to you when they get there. Um … they were just asking me a couple of questions while they were still on their way out there. PH: Sure. Sure. OK. D: Alright? No problem. Is he still in his room? PH: Yes. My husband’s in there with him, but he’s becoming more and more belligerent and … um … D: OK. Your husband’s in the room with him now? PH: Yes. D: OK. I’ll let them know about this information. PH: OK. Thank you. [End call #2] The Call for a CIT Officer (Hindsight 4) Slightly edited transcript (Call #3, about 1 minute later) D: Ms. Hobart? … This is J__ again. Are there any weapons in his room or anything? Does he have any? PH: No, no. He’s got a drum set in his room. D: OK. He’s not under the influence, is he? PH: No. D: OK. These are just … a couple of questions the officers were asking. PH: We just want to transport him as soon as possible. D: Has he done this before? PH: He was hospitalized a year and a half ago, but that was something where he was driving at night. He took one of our cars and was stopped for reckless driving. D: OK. Well, they’re almost there. PH: Well, Thank you. [End call #3] Record from Officer’s Dash-Cam Audio (Hindsight) 15:07:40-43 Officer: “Tell RP to step outside” 15:08:00-03 (sound of door opening) PH: “Come in?” 15:08:09-12 PH: “You’re with the police?” Officer: “Yes.” 15:08:12-15 (More talk, words not distinct on radio recording. Recollection was PH: “I’m glad you’re here.”) 15:08:15 Start of “Stop … Stop” (both PH and Officer, according to statements) 5 seconds of scuffle 15:08:20-22 Six shots fired. 15:08:23-24 Officer: <Cursing> 15:08:25 Officer: “224 shots fired” So … What went wrong? Why Did This CIT Call Go Bad? In one word: Preparation 1. We were not prepared to deal with the police. 2. The police were not prepared to properly handle a CIT call. Lessons Learned Lessons for persons at risk of a brain disorder crisis (1) Bad News – Good News Bad news: You are at risk if you have had an “episode” in the past. Good News: You are not alone in this. Lessons for persons at risk of a brain disorder crisis (2) Your disorder is not your fault. You didn’t cause it. You didn’t ask for it. You didn’t do anything to deserve it. It is your body, your disorder, your life, your responsibility. You are accountable for what you do with it. You have to learn to manage it. You need to plan for a possible “episode”. Failure to plan is planning to fail. Failure can cost you your life. Lessons for persons at risk of a brain disorder crisis (3) To manage your disorder, you need to learn about it. Diagnoses are often based primarily on interpretation of observed symptoms, rather than identification of specific causative factors. Ritsner, M., “Is a Neuroprotective Therapy Suitable for Schizophrenia Patients?”, in M. Ritsner ed. “Brain Protection in Schizophrenia, Mood and Cognitive Disorders”. Vulnerability – Stress Model for Mental Illness Current paradigm for psychiatric brain disorders is that a combination of vulnerability and stress leads to the manifestation of symptoms and additional damage to the brain. Vulnerabilities and stressors can include: genetics, glandular problems, nutrition, trauma, toxins, infections, psychosocial stressors, birth complications and more. from Ritsner Some “Non-Psychiatric” Conditions Associated With Psychosis Some causes are more treatable than others. Anti-psychotics are not always the answer. White et al., American Journal of Psychiatry, 163:3, March 2006 See also: http://en.wikipedia.org/wiki/Psychotic_disorders#Psychiatric_disorders Managing Your Brain Disorder • How has it manifested itself? What changed during a crisis? • Perception of reality: Examples: Paranoia? Voices? Hallucinations? Delusions of Grandeur? Alternate personality? • Attitude about yourself: Examples: Mania? Depression? Suicidal thoughts? Omnipotence? • Attitude toward others: Examples: Fear? Belligerence? Withdrawal? Shame? Suspicion? • Behavior: Examples: Pacing? Skipping meals? Skipping regular personal hygiene? Hoarding? “Bizarre” activities? • What may have indicated that a crisis could be imminent? • Sleeplessness? Frenetic activity? Reclusiveness? Recurrent or obsessive thoughts? Change in daily habits? • What can you do about it? • • • • Consult with a psychiatrist Prescribed medications (self-medication is a prescription for problems) Therapy Investigate possible vulnerabilities, causes or “triggers” Lessons for persons at risk of a brain disorder crisis (4) You need to plan for an eventual crisis, even though it may be scary to even consider the possibility: • Anti-psychotics generally do not cure brain disorders. • Anti-psychotics can reduce the frequency of crises, but likely will not eliminate them altogether. • Various forms of psychotherapy can help in self-awareness and coping with the illness, but they do not address the underlying biological disorder. If you do not pre-plan for a crisis, others will have to make decisions for you when it occurs. The urgency of the situation will likely lead to suboptimal decisions, despite the best intentions. Elements of a Sample Crisis Plan Credit NAMI Minnesota: http://www.namihelps.org/Crisis-Booklet-Adults.pdf Further Elements of a Mental Health Crisis Plan (1) Must keep in mind the goal: Get to the “other side” of the crisis with no harm to yourself or others. Know who is going to be involved in responding to your crisis. • Caregiver(s) • Doctor(s): primary care, psychiatrist, admitting doctor • Transport personnel: police department or specialty transport services • How will the call for help be routed and dispatched? • Who will be dispatched? What will be their training? Are they equipped to do the job? Will they seek to preserve your comfort and dignity? • Justice of the Peace: How can Mental Health Warrant process be expedited? Flowchart for Deployment of Mobile Crisis Outreach Team Further Elements of a Mental Health Crisis Plan (2) Must keep in mind the goal: Get to the “other side” of the crisis with no harm to yourself or others. Discuss, preferably in person with each potential team member, what you can expect each member of your team to do in responding to your crisis. • Get feedback: Is your plan realistic? • Will they honor your plan? • Contingencies: e.g. What if there are no beds? What if a part of your “team” is unavailable at the time of crisis? Further Elements of a Mental Health Crisis Plan (3) Crisis kit (for patient and caregiver): Physical: • Toiletries, • Comfortable change of clothes • Reading material and/or music with earphones • Other medications, snacks (consider shelf life) Documentation: • Medical and psychiatric records • Prescription history • Insurance documents • Medical (or full) power of attorney or guardianship papers • HIPAA (and state) release forms • Crisis plan notes and documents • Copies of previous mental health warrants or other legal matters • Certificate of Medical Examination • Partially filled-out mental health warrant Caregivers (1) 1. Help loved one take responsibility for life decisions. • Matter of maturity and necessity • Encourage development of appropriate treatment or management strategy in line with loved one’s life goals. • Encourage investigation of possible causes or triggers for mental health crises. 2. Encourage socialization, education and employment 3. More autonomy for your loved one • Autonomy is a consequence of taking responsibility • Reduces interpersonal stress • Shows respect (dignity) • Can enrich life experiences • May even lead to healthy independent living (hope) Caregivers (2) Do not assume that there will not be another episode. Plan for another episode. Odds are that it will happen. Do not assume adhering to medication regime will prevent a recurrence. In general, medication may reduce, but not eliminate, risk of another episode. Work with loved one on his/her plan. Suggestions for augmenting your loved one’s plan: • Have back-up medication (consider shelf life) • Get to know the CIT officers in your jurisdiction • Know what resources are available • Know where you want to take your loved one • Have information ready for dispatcher and CIT officer • Have insurance information available Caregivers (3) A mental health crisis can entail complex legal issues. These need to be included in crisis planning. Consider finding an appropriate lawyer ahead of time. Laws and procedures may vary from one jurisdiction to the next. The laws are written to protect the rights of patients. Oftentimes, they presume that a conscious patient is competent. • Guardianship, Medical power of attorney and/or Durable Power of Attorney (These only permit you to consent on behalf of your loved one for medical treatment and psychiatric exams, not for commitment.) • HIPAA release • Learn the local laws and procedures: o Emergency detention o Mental health warrants o Voluntary admission for mental health services o Court-ordered mental health services Caregivers (4) Your loved one may enter a crisis in a public situation. Obliviousness to the social setting may result in an arrest for “disorderly conduct”, disturbing the peace, trespassing or some other charge. There is a potential for escalation, especially if they resist arrest or otherwise fail to give sufficient deference to an officer’s authority. If your loved one is not diverted from the criminal justice system into appropriate care: o Protecting your loved one’s legal rights, e.g. to remain silent or have an attorney present during questioning, may become problematic. o Access to psychiatric care and all medications may be delayed for several days, even if all the protocols are understood and observed. o What to do about possible criminal arrest record? Impact on career prospects, etc. Some Potential “Gotcha’s” for Consumers and Caregivers (1) Some entities calling themselves “crisis intervention” responders are actually providers of psychological counseling services for people having life crises (e.g. home loss due to a hurricane). They are not prepared to be primary responders to people having psychiatric emergencies. Know your crisis support team! (2) There are some situations under which a “Mobile Crisis” unit will not respond. • Situation insufficiently severe to warrant assistance • Situation sufficiently dangerous to warrant use of a trained peace officer Psychiatrists Work with patient and caregiver to determine cause of illness Do not assume the cause Eliminate as many causes as possible. • Toxins • Tumors • Trauma • Endocrinology, etc. Respect patient’s right to choose, but be as informative and persuasive as possible regarding the most appropriate course of action. Work with caregiver and patient to plan for another possible episode Community and crisis response resources Treatment facility options Emergency medication plan Obtain admitting privileges Certificate of medical examination (TX) Hospitals that Receive Mental Health Patients Strive to keep at least one bed available for psychiatric patients. Be liberal in granting admitting privileges to psychiatrists who treat patients with serious brain disorders. Have a mental health professional on call at all times. Note: psychiatric emergencies do not observe 9-5 working hours or holidays. Local Governments Actively ensure all departments are complying with the letter and spirit of ADA, especially in areas where it can make a difference between life and death. Take advantage of assistance and information available from the US Department of Justice and other organizations. Consider the liability risk of not having CIT. Police Chief / Police Department (1) Implement a plan for “Crisis Intervention” calls. • Numerous resources available. • Many examples of CIT programs already implemented. o There is no need to “re-invent the wheel”. o Examples: Memphis model, co-responder model o The program specifics will have to be tailored to local needs and resources. • Best plans have the support of local governments, the mental health community and consumer / caregiver buyin. Police Chief / Police Department (2) CIT call response requires a coordinated team effort. Make up of team depends on local resources • Mental health specialist (if available) • CIT Officer – leader of the team if no mental health professional • Back-up officers (no solo CIT call responses) • Call taker / Dispatcher • Caregiver at the scene (!) Police Chief / Police Department (3) The public needs to know what to expect from your CIT program o Especially consumers, caregivers, counselors and psychiatrists o Encourage CIT officers to assist consumers in development of their crisis plans o Website a source of information and good public relations (e.g. Houston, Memphis and others) Police Chief referring to state-mandated 16hour “CIT training” at the police academy. Police Chief / Police Department (4) Establish General Orders for CIT Officers, support officers (no solo CIT calls), call takers and dispatchers in how to handle calls requiring CIT service. Ensure that the General Orders are up-to-date with respect to the all laws, including case law, as well as best practices. Require all officers and dispatchers to become familiar with the General Orders. - Call Taker / Dispatcher Police Chief / Police Department (5) Ensure that your personnel are adequately trained o No gaps in the academy training and Field Training. o Field training should include supporting role in mental health call scenarios. o Call takers / dispatchers should be trained to field calls from the mentally ill or their caregivers as well as from persons with a complaint about the behavior of a possibly mentally ill person. - Responding Officer - Call Taker / Dispatcher Police Chief / Police Department (6) Suggested Competencies for CIT Call Response (Not intended to be an exhaustive list) “CIT Officer”: Trained, empathetic, motivated, experienced leaders CIT is a specialty, just like SWAT is a specialty Primary concern is safety of all people at the scene Can comfortably and respectfully work with all personnel involved: the team, mental health personnel, caregivers, consumers, judges At least 40 hours specialist training Need to know how to direct a team (always have back-up) Needs to retain authority even if more senior, but less qualified, officers arrive (e.g. Nagle/Casey case, another call gone bad) as long as the mission is a crisis intervention. Has pre-arrival briefing with team Consults with caregiver at the scene Conducts drills and post-mission reviews with team Equipped with full range of less than lethal options Police Chief / Police Department (7) Suggested Competencies for CIT Call Response (Not intended to be an exhaustive list) CIT Officer back-up: A CIT call should not be a solo operation Back-up team members need to know their roles Back-up can be over-zealous to protect one another (e.g. Meadours case, another call gone bad) Understand elements of CIT Officer briefing o What is known and interpreted about the situation o Safety guidelines o Verbal signals • When to have force at the ready • When to deploy a particular form of force or restraint Trained and equipped for multiple non-lethal custody-taking techniques Police Chief / Police Department (8) Suggested Competencies for CIT Call Response (Not intended to be an exhaustive list) Call-taker / Dispatcher: Knows how to determine if a call requires a Crisis Intervention Team Knows how to handle calls requiring CIT services o Proper dispatching o Obtaining the right information from the caller o Instructing the caller on what to expect o Coaches caller in keeping situation stable o Participates in drills Police Chief / Police Department (9) Foster a mentoring / learning atmosphere: • • • • Post-action reviews Compile and disseminate lessons learned Continually update documented best practices Supplementary training - Responding Officer - Call Taker / Dispatcher Post-Action Review: CIT International Example Incident Tracking Form http://www.citinternational.org/images/stories/CIT/SectionImplementation/Outcomes/TrackFormCITINT.htm For Everybody Involved Common Goal: to compassionately secure assistance to people in a brain disorder crisis in order to prevent harm to themselves and to others. Components of a compassionate community • Without participation of consumers and caregivers, there is no need to bother with CIT. • Without mental healthcare resources, there is no need to bother with CIT. • There is no CIT without trained responders. Communication • Lay people, police, trained medical personnel don’t always speak the same language. • Trigger words: “violent”, “afraid”, “danger”, “risk” Compassion • People suffering from brain disorders need help, not hardship. Cooperation • A call for assistance from a caregiver or a person in crisis is generally not a request to put someone in jail or to inflict pain or injury on anyone. • Caregivers and CIT responders need to cooperate when possible in safely securing appropriate care for the person with a brain disorder crisis. A Caregiver’s Perspective Primary concerns for their loved one: 1. Safety 2. Health 3. Comfort 4. Dignity Apart from the consumer, the caregiver has the most “skin-in-the-game” and is extremely anxious to ensure that everything goes well for their loved one. In the absence of a breach of the law, the mentally ill person is not a “suspect” or a “perp”. When CIT call responses involve uniformed officers arriving in police cars with flashing lights, taking a family member away in handcuffs (or on a stretcher), this creates a disincentive to requesting CIT “services”. Failure to irreproachably execute a CIT mission can severely damage trust in the system by the consumer/caregiver community. “Killing is unnecessary” Workshop • Constructive criticism – brief to allow more participation • Your most important item • Will edify everyone present – THANK YOU !!! • Will improve future presentations – THANK YOU !!!