Method for Induced Abortion
advertisement

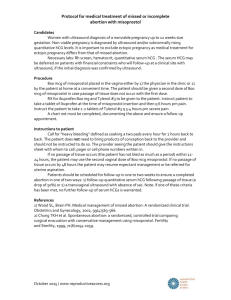
Method for Induced Abortion OBSTETRICS & GYNECOLOGY Volume 104, Number 1, July 2004 R3 박영미 First trimester abortion Vacuum curettage Complications of vacuum curettage abortion Medical abortion in the first trimester Complications of early medical abortion Second trimester abortion Dilation and evacuation Complications of dilation and evacuation Labor induction methods Fetal death in utero Selective fetal reduction Methods for abortion in the first trimester Vacuum curettage The most common method of abortion in the United States Before 13 weeks : suction or vacuum curettage After 13 weeks : dilation and evacuation (D&E) Antibiotics Marked reduction in postabortal infection Tetracycline, doxycycline, minocycline : broad spectrum of antimicrobial effect : oral absorption Vacuum curettage Pain relief Paracervical block Nonsteroidal anti-inflammatory drugs 10-20mL of 1% lidocaine Deep injection into the cervical stroma at multiple site Addition of 2-4 units of vasopressin to the anesthetic solution -> reduces blood loss -> prevent postabortal uterine atony Preoperative administration -> modest reduction in pain Conscious sedation Intravenous midazolam 1-3mg and fentanyl 50-100ug Vacuum curettage The necessary dilatation of the cervix Mechanical cervical dilation with tapered cervical dilators Hygroscopic dilators – laminaria Reduces risk for perforation or cervical laceration Prostaglandins – misoprostol 400ug vaginal dose, 3-4 hours before procedure Minimal side effects, little expense Vacuum curettage For complete abortion and early diagnosis of ectopic pregnancy Preoperative ultrasonography Careful inspection of the aborted tissue Follow up with serial hCG titer Manual vacuum aspiration 6mm flexible cannula and modifed 60ml syringe Effective in pregnancies as early as 3 weeks As safe and effective as electric vacuum through 10weeks of pregnancy Used to treat Incomplete spontaneous abortion in office or emergency room Complications of vacuum curettage - Immediate complications Excessive bleeding Cause Incomplete abortion Pregnancy of more advanced gestational age than expected Uterine atony Low-lying implantation Uterine injury Management Misoprostol 1000ug, rectally or buccally 30ml balloon Foley catheter : inserted into the uterine cavity, inflated with 50-60ml of sterile saline Complications of vacuum curettage Persistent postabortal bleeding Cause Retained tissue or clot (hematometra) Trauma Management Prompt surgical intervention : laparoscopy : repeat vacuum curettage Selective uterine artery embolization Rarely, hysterectomy Complications of vacuum curettage Uterine perforation Risk 1 in 1000 first trimester abortion Increases with gestational age, parous women Perforations at the junction of the cervix and lower uterine segment lacerate the ascending branch of the uterine artery within the broad ligament severe pain, broad ligament hematoma, intra-abdominal bleeding laparotomy to ligate the severed vessels and repair the uterine injury Complications of vacuum curettage Low cervical perforation Injure the descending branch of the uterine artery within the cardinal ligaments The bleeding is external, through the cervical canal -> subside temporarily as the artery goes into spasm -> no intra-abdominal bleeding Management Hysterectomy Arteriography and selective uterine artery embolization Complications of vacuum curettage Hematometra Symptom & sign Lower abdominal pain : increasing intensity in the hour after an abortion Large, globular, tense uterus Management Immediate re-evacuation Pretreatment with ergot 0.1mg IM, the use of oxytocin Addition of vasopressin to the paracervical anesthetic Complications of vacuum curettage Early detection of ectopic pregnancy, incomplete abortion Immediate fresh examination of the specimen If no chorionic tissue The gestational sac, chorionic villi are easily visualized Frozen section : to rule out ectopic pregnancy A few villi but no gestational sac Retained pregnancy tissue in the uterus Complications of vacuum curettage - Later complication Retained tissue or clot & early endometritis Symptom & sign ① No response to simple analgesics ② Excessive and prolonged bleeding ③ Severe pain or fever Management ① Broad spectrum oral antibiotics ② Vacuum evacuation in the clinic Complications of vacuum curettage Advanced sepsis Symptom & sign ① generalized abdominal tenderness & guarding ② tachycardia ③ significant fever ④ prostration Management ① immediate hospital care ② prompt uterine evacuation ③ high dose combinations of antibiotics ④ intensive care for cardiovascular support with fluid resuscitation, monitoring with central lines Medical abortion in the first trimester Three highly effective regimens Mifeprostone (RU-486) + misoprostol Methortexate + misoprostol Misoprostol alone Medical abortion in the first trimester Mifepristone + prostaglandin analogue The first highly effective means Mifeprostone : analogue of norethindrone : high affinity for progesterone receptors -> act as a false transmitter and blocks natural progesterone Effectiveness : increased to approximately 95% by the addition of lowdose prostaglandin Medical abortion in the first trimester The U.S FDA : Mifepristone 600mg orally, followed by misoprostol 400ug orally 2days later : Use is limited to the first 49days of amenorrhea Evidence-based protocol : Mifeprostone 200mg orally, followed by selfadministered vaginal misoprostol 800ug at home : Vaginal misoprostol -> lower peak serum level, more sustained blood level -> administered at 24,48,72 hours after the mifeprisotne (no difference in efficacy) : The effective gestational age can be safely extended from 49 to 63 days of amenorrhea Medical abortion in the first trimester Methotrexate + misoprostol Regimen : Methotrexate 50mg/m2 single intramuscular dose, followed vaginal imsoprostol 800ug at 3-7days : Expulsion of the gestational sac has not occurred -> Misoprostol is repeated in 24hours Effectiveness : 53% aborted after the first dose of misoprostol, additional 15% after the second dose, total of 92% by 35 days Medical abortion in the first trimester Misoprostol alone Regimen : Vaginal misoprostol 800ug initially, followed by 800ug at 24 hours, if needed Effectiveness : Complete abortion rate : 92% : As effective as mifepristone/misoprostol and much less expensive Medical abortion in the first trimester Vaginal ultrasonography after start of medical abortion Performed to ensure that the uterine cavity is empty Intact gestation with cardiac echoes 2weeks after start of medication -> failed abortion Gestational sac is present but no fetal cardiac activity -> wait for expulsion, take more misoprostol -> have surgical evacuation If medical abortion fails, surgical termination is advisable : possible risk for fetal malformation from misoprostol and methotrexate Complications of early medical abortion Persistent bleeding The duration of bleeding or spotting : 9-16 days after mifeprisotne/ misoprostol : up to 8% as long as 30 days Need for curettage is related to gestational age ( 200mg mifepristone + 800ug vaginal misoprostol ) : 2.1 % at 49 days or less : 3.1% at 50-56 days : 5.1% at 57-63 days Complications of early medical abortion Hausknecht : the complications report ( November 2000 to May 2002, 80,000 women who received mifepristone ) Vacuum curettage for bleeding or for persistent non-viable pregnancy A death of a woman with a ruptured ectopic pregnancy Infection (0.013%) Sepsis with adult respiratory distress syndrome Coronary artery thrombosis Second-trimester abortion Dilation and Evacuation Dilation of the cervix Laminaria method : Prevailed because of ① concerns about cervical injury for mechanical dilation ② the greater technical ease of second-trimester procedures : More laminaria are used as gestational age ① After 20 weeks -> 10 more laminaria ② 10-13 laminaria at 20-23 weeks -> greater than 14mm by the next day Dilation and Evacuation : Method ① Initial set of 2-3 medium laminaria ② 4 or more new laminaria to the first set 6 hours later ③ Dilatations of 18 mm or more by the next day in 92% Misoprostol treatment : Replace laminaria in the early second trimester : method ① ② ③ ④ 600ug administered buccally 2-4 hours before procedure At 14-16 weeks of gestation Sufficient dilation to allow insertion of a 14mm vacuum curette Dilation and Evacuation Instrument technique At 13-15 weeks : Readily evacuation with vacuum cannula of 12-14mm -> Ovum forceps (as an adjunct) : The surgeon may prefer to use forceps as the primary and use the vacuum only the end of the procedure Through 16 weeks : The 16mm cannula system, vacuum curette alone At 17 weeks and beyond : Even large diameter aspiration system is not adequate by itself : Forceps evacuation ,the primary method and vacuum, the secondary method Dilation and Evacuation Decrease of blood loss Intravenous oxytocin : 40 or more units per 1000mL : During the procedure or begun after uterine evacuation is completed Vasopressin : Two to four units mixed with the local anesthetic solution : Diluted with 10-20mL sterile saline : Injected into the cervix Dilation and Evacuation The patients The obese patient : Increased procedure difficulty, procedure time, blood loss with increasing body mass index : BMI greater than 30 -> 20% longer time for procedure -> 40% more difficult by the operator Placenta previa : Not a contraindication to laminaria with D&E Previous cesarean delivery : Not increase perioperative risk of D&E Dilation and Evacuation Intact D&E procedure ① 2 or more days of laminaria treatment to obtain wide dilation of the cervix ② Assisted breech delivery of the trunk of the fetus, under ultrasound guidance ③ The calvarium is decompressed ④ Delivered with the fetus otherwise intact Dilation and Evacuation Combination D&E technique ① After multistage laminaria treatment over 2 or more days ② 1.5-2.0mg of digoxin are injected into the fetus under ultrasound guidance ③ The membranes are ruptured ④ Intravenous oxytocin is started (167mU/min) ⑤ Assisted delivery is performed after a few hours Complications of dilation and evacuation The same as first-trimester surgical abortion : no more frequent when laminaria are used Perforation 0.32% for D&E at 13-20 weeks : but, 0.05% with first-trimester vacuum curettage Lead to bowel injury and require laparotomy : but, safely managed with laparoscopy with first trimester Complications of dilation and evacuation Hemorrhage Caused by incomplete procedure, uterine atony, trauma (as in the first trimester) At the later gestational ages, risk for DIC increases : 8 / 100,000 first trimester : 191 / 100,000 second trimester Amniotic fluid embolism Rare and less frequent with vacuum curettage and D&E than with labor induction technique Must be considered when a patient exhibits respiratory difficulty while undergoing an abortion Labor induction methods Hypertonic solution Intra-amniotic hypertonic saline : The first effective labor induction method for second trimester abortion : Hypertonic urea : Potentially safer agent –> intravascular injection would not be harmful : Intra-amniotic dose of 80-90g is effective : injection-to-abortion intervals are prolonged Labor induction methods Intra-amniotic prostaglandin F²α Effective, but often required a second injection Associate with : Transient fetal survival in some cases : Significant gastrointestinal side effects : Failure of the primary technique : Risk for cervical rupture, in the primigravida Overnight treatment with laminaria tents reduced : The mean time from instillation to abortion from 29 hours to 14 hours : The need for second injections Labor induction methods Systemic prostaglandins Three different prostaglandis ① Dinoprostone (prostaglandin E2) ② Carboprost tromethamine (Hemabate) ③ Misoprostol Labor induction methods Dinoprostone 20mg vaginal suppository every 3 hours The mean time to abortion : 13.4 hours 90% aborting by 24 hours Reducing the dinoprostone to 10mg at 6 hour intervals combined with high-dose oxytocin -> the same efficacy but fewer gastrointestinal side effects Carboprost tromethamine 250ug every 2 hours intramuscular injection The mean time to abortion : 15-17 hours About 80% aborting by 24 hours Labor induction methods Misoprostol The ideal dose and interval is still under investigation 200ug vaginally every 12 hours : Equally effective with dinoprostone 20mg every 3 hours : Fewer side effects (vomiting, diarrhea, fever) 200ug, 400ug, 600ug at 12 hour intervals : Abortion by 48 hours to be 70.6%, 82%, 96% : Vomiting, diarrhea, fever increased with the dose High doses and short intervals : increase risk for uterine rupture : 3 case of uterine rupture with previous cesarean delivery Labor induction methods Mifepristone and prostaglandins Method ① Mifepristone is administered ② 3 days later the patient is hospitalized for prostaglandin treatment (gemeprost, misoprostol) Typical intervals from start of the prostaglandin to abortion : 7-9 hours Recent studies use misoprostol more often : low cost and high efficacy Labor induction methods High dose oxytocin Method ① 50 units in 500mL of 5% dextrose and normal saline given over 3 hour period ② After 1 hour rest ③ Oxytocin infusion is repeated, adding 50 additional units to the next 500mL infusuon, continuing with 3 hour ④ And 1 hour of rest ⑤ Repeat until the patient aborts or a final solution of 300 units of oxytocin in 500mL is reached Labor induction methods Use of feticidal agents Feticidal agents : reduces the induction to abortion interval and improve efficacy Method ① 60mL of 23% saline solution ② Intra-amniotic urea ③ Ultrasound guided fetal intra-cardiac injection of potassium chloride ④ 1.0-1.5mg of digoxin given : ultrasound-directed intrafetal injection : into the amniotic sac Labor induction methods Hysterotomy and hysterectomy Little indication as the primary method for abortion : because the risk of major complications and death is greater than for any other technique The only need for hysterotomy in failed abortion : uterine anomaly Fetal death in utero Vaginal Prostaglandine E2 Highly effective after fetal death Producing fetal abortion in about 10 hours Side effect : vomiting, diarrhea, fever Beyond 24 weeks, the full dose of 20mg should not be used -> uterine rupture Misoprostol Increasingly used to manage fetal death Vaginal 200ug at 12 hour intervals Safe and effective in the second trimester The dose should be reduced in the third trimester Initial dose of 25ug at 6 hour intervals Increasing to a maximum of 50ug at 6 hour intervals Fetal death in utero Hemorrhage begun after abortion -> DIC should be suspected If the uterus appears intact on manual exploration ① intramuscular carboprost, immediately : stop the bleeding, even in the presence of DIC : reduce the need for blood products ② misoprostol 1000ug rectally : used successfully for postpartum hemorrhage Selective fetal reduction Method Indication US guided intra-cardiac injection of potassium Multiple pregnancy, to avoid the risk of extreme prematurity for the surviving pregnancies One anomalous fetus of multifetal gestation Contraindication Monoamniotic twins Twin-twin transfusion syndrome -> embolic phenomena -> infarction in the surviving twin Selective fetal reduction Fetal loss Higher with higher starting numbers of gestations ① Starting number > 6 -> 15.4% ② Starting numbers =2 -> 6.2% Higher if more fetuses were left intact ① Finishing number = 3 -> 18.4% ② Finishing number = 1 -> 6.7%