What's an incomplete? Issues of incomplete abortion diagnosis and
advertisement

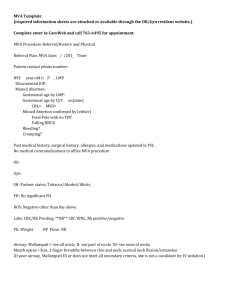
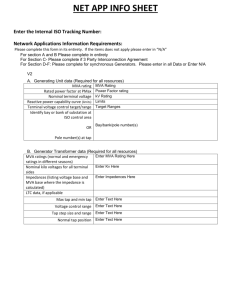
Manual Vacuum Aspiration (MVA) for Early Pregnancy Loss Sarah Prager, MD Department of Obstetrics and Gynecology University of Washington Adapted from the Association of Reproductive Health Professionals, Washington, DC, USA Incidence of Early Pregnancy Loss ≤ 20 weeks’ gestation 12%–24% of pregnancies 600,000 to 800,000 annually Griebel CP, et al. Am Fam Physician. 2005.; Everett C. BMJ. 1997. Smith NC. Contemp Rev Obstet Gynecol. 1988.; Stirrat GM. Lancet. 1990. What Is a Manual Vacuum Aspirator? •Has locking valve •Is portable and reusable •Vacuum is equivalent to electric pump •Efficacy is same as electric vacuum (98%–99%) •Has semi-flexible plastic cannula Creinin MD, et al. Obstet Gynecol Surv. 2001.; Goldberg AB, et al. Obstet Gynecol. 2004.’ Hemlin J, et al. Acta Obstet Gynecol Scand. 2001. Comparison of EVA to MVA EVA MVA Vacuum Electric pump Manual aspirator Noise Variable Quiet Portable Not easily Yes Cannula 4–16 mm 4–12 mm Capacity 350–1,200 cc 60 cc Suction Constant Decreases to 80% (50 mL) as aspirator fills Dean G, et al. Contraception. 2003. Clinical Indications for MVA Uterine evacuation in the first trimester: • Induced abortion • Spontaneous abortion Incomplete medication abortion Uterine sampling Post-abortal hematometra Hemorrhage Creinin MD, et al. Obstet Gynecol Surv. 2001.; Edwards J, Creinin MD. Curr Probl Obstet Gynecol Fertil.1997.; Castleman LD et al. Contraception. 2006; MVA Label. Ipas. 2007. Using MVA for treatment/completion of spontaneous abortion Treatment for spontaneous abortion Ensures POC are fully evacuated Comfortable for woman due to low noise level Portable for use in physician office familiar to the woman Women very satisfied with method • Very few studies on MVA in spontaneous abortion MVA Label. Ipas. 2007. MVA Instruments Steps for Performing MVA A step-by-step, onepage poster is available from the manufacturer to guide clinicians through the procedure Products of Conception (POC) Procedure is complete when POC are identified Electric Suction Machine Edwards J, et al. Am J Obstet Gynecol. 1997. MacIsaac L, et al. Am J Obstet Gynecol. 2000. MVA Aspirator Moving Out of the Operating Room Miscarriage Management: Why the OR? Current practices developed when • • • • Abortion was illegal Uterine evacuation was an emergency Antibiotics were not available Access to blood transfusion was very limited “Puerperal (childbed) fever was the scourge of nineteenth-century obstetrics and abortion.” - Joffe 1999 Advantages of Moving Treatment from OR to Outpatient Setting • Avoid the repeated exams that often occur in the hospital • Simplify scheduling and reduce wait time Average OR waiting time in U.K.-based study: 14 hours, with 42% of women not satisfied • Save resources • Avoid cumbersome OR protocols Prolonged NPO requirements & discharge criteria Demetroulis 2001; Lee and Slade 1996 Advantages of Moving Treatment from OR to Outpatient Setting (continued) • Office affords more treatment options • • • • Vacuum aspiration or misoprostol Pain management choices Improved patient autonomy and privacy Convenience Personalized care Patient education Lee and Slade 1996 Moving Incomplete Abortion to an Outpatient Setting: Johns Hopkins Methods • N = 35, incomplete first-trimester abortion • Compared treatment with MVA in labor and delivery vs. conventional care (suction curettage in OR) Blumenthal and Remsburg 1994 Moving Incomplete Abortion to Outpatient Setting: Johns Hopkins Results • Decreased anesthesia requirements • Decreased overall hospital stay, from 19 to 6 hours • Decreased patient waiting time by 52% • Decreased procedure time, from 33 to 19 minutes • Decreased costs per case: $1,404 in OR $827 in L&D $200 or less in ER Blumenthal 1994 Moving Incomplete Abortion to Outpatient Setting: Johns Hopkins Cost Comparisons Charges Admission Supplies Anesthesiology ___________________ Total Hospital Charges Outpatient MVA OR Procedure Mean ($) Mean ($) 10 58 6 137 125 85 _______ ________ $ 827 $1404 $577 saved per procedure with MVA Blumenthal 1994 Use Caution in Women with… • • • • • Uterine anomalies Coagulation problems Active pelvic infection Extreme anxiety Any condition causing the patient to be medically unstable Complications with MVA Very rare Same as EVA May include: • • • • • MVA Label. Ipas. 2004. Incomplete evacuation Uterine or cervical injury Infection Hemorrhage Vagal reaction MVA vs. EVA Complication Rates Methods Vacuum aspiration for abortion up to 10 wks LMP Retrospective cohort analysis Choice of method (MVA vs. EVA) up to physician n = 1,002 for MVA; n = 724 for EVA Charts reviewed for complications more… Goldberg AB, et al. Obstet Gynecol. 2004. MVA vs. EVA Complication Rates (continued) Complications • 2.5% for MVA • 2.1% for EVA (p = 0.56) • No significant difference *Elective not spontaneous studies Goldberg AB, et al. Obstet Gynecol. 2004. more… MVA vs. EVA Complication Rates (continued) Choice of MVA vs EVA in procedures • Attendings: 52% MVA • Gyn residents: 59% MVA • Other residents: 76% MVA (p<0.001) Goldberg AB, et al. Obstet Gynecol. 2004. Early Abortion with MVA: Study • Methods • 2,399 MVA procedures, < 6 weeks LMP • Meticulous inspection of POC immediately after MVA • Results • 99.2% effective in terminating pregnancy • 6 repeat aspirations (0.25%) • 14 ectopic pregnancies (0.6%) diagnosed and treated Edwards J, Creinin MD. Curr Probl OIbstet Gynecol Fertil. 1997. MVA and POC: Study • In group overall • n = 1,726, up to 10 weeks LMP • Complication rates between MVA and EVA • 37 patients at < 6 weeks’ gestation • In 35 of 37, provider chose MVA • No re-aspirations needed in patients < 6 weeks more… Goldberg AB, et al. Obstet Gynecol. 2004. MVA and POC: Study (continued) “…Significantly more re-aspirations for inability to accurately identify the pregnancy occurred in electric group.” Goldberg AB et al. Obstet Gynecol, 2004 Goldberg AB, et al. Obstet Gynecol. 2004. Patient Satisfaction • Both EVA and MVA groups were highly satisfied • No differences in: • • • • • Pain Anxiety Bleeding Acceptability Satisfaction • More EVA patients were bothered by noise Bird ST, et al. Contraception. 2003.; Dean G, et al. Contraception. 2003.; Edelman A, et al. Am J Obstet Gynecol. 2001. MVA Safety and Efficacy: Summary • MVA is simple • Easily incorporated into office setting • Training/Practice Issues • • • • • Expanding pain management options Ultrasound as needed No sharp curettage Patient-provider interaction Instrument processing for multiple use (new guidelines) MVA and Pain Pain is made worse by: Fearfulness Anxiety Depression Belanger E, et al. Pain. 1989.; Smith GM, et al. Am J Obstet Gynecol. 1979. Hansen GR, Streltzer J. Emerg Med Clin N Am. 2005. Effective Pain Management Respectful, informed, and supportive staff Warm, friendly environment Gentle operative technique Women’s involvement Effective pain medications Pain Management Techniques With addition of: • Focused breathing: 76% • Visualization: 31% • Localized massage: 14% General or nitrous 10% 32% Local + IV 58% Local Lichtengerg ES, et al. Contraception. 2001. Good M, et al. Pain Manag Nurs. 2002. Paracervical Block Regular Injection Castleman L, Mann C. 2002. Maltzer DS, et al. 1999. Deep Injection Efficacy of Ancillary Anesthesia • Importance of psychological preparation and support • Music as analgesia for abortion patients receiving paracervical block • 85% who wore headphones rated pain as “0,” compared with 52% of controls • Verbicaine (“Vocal Local”)/Distraction Therapy Shapiro AG, Cohen H. Contraception. 1975. Stubblefield PG.Suppl Int J Gynecol Obstet. 1989. Sharp Curettage and Pain Often requires increased dilatation Often painful More difficult to reduce anesthesia Forna F, Gulmezoglu AM. Cochrane Library. 2002. Sharp Curettage and MVA Generally not indicated Not routinely recommended after MVA more… WHO. 2003 Ultrasound and MVA Not required for MVA Used by some providers routinely Use contingent on provider preference and experience Word Health Organization. 2003. Counseling for MVA Effective counseling occurs before, during, and after the procedure •Woman-centered •Structured completely around the women’s needs and concerns more… Breitbart V, Repass DC. J Am Med Womens Assoc. 2000.; Hogue CJ, et al. Epidemiol Rev. 1982; Steward FH, et al. 2004. Hyman AG, Castleman L. 2005 Counseling for MVA (continued) • Prepare women for procedure-related effects • Address women’s concerns about future desired pregnancies more… Breitbart V, Repass DC. J Am Med Womens Assoc. 2000.; Hogue CJ, et al. Epidemiol Rev. 1982; Steward FH, et al. 2004. Hyman AG, Castleman L. 2005 Counseling for MVA (continued) Quality of counseling Picker Institute. 1999. Patient satisfaction with care Post-Procedure Care • Observe for complications • Bleeding • Pain • Monitor pain and treat accordingly Monitor vital signs Check bleeding and pain more… Post-Procedure Care (continued) Give instructions for aftercare/follow-up Discuss contraception, if appropriate Discharge patient • Tolerates oral intake (general anesthesia only) • Vital signs are normal • Bleeding is minimal Lichtenberg ES, Shott S. Obstet Gynecol. 2003. Instructions for Aftercare Warning signs to call a clinician Pain management options Prophylactic antibiotics • Many regimens effective When to return to normal activities Lichtenberg ES, Shott S. Obstet Gynecol. 2003. When Women Should Contact Clinician Heavy bleeding with dizziness, lightheadedness Worsening pain not relieved with medication Flu-like symptoms lasting >24 hours Fever or chills Syncope Any questions For more information on EPL • Association of Reproductive Health Professionals (ARHP) archived webinar: Options for Early Pregnancy Loss: MVA and Medication Management www.arhp.org/healthcareproviders/cme/webc me/index.cfm • Ipas WomanCare Kit for Miscarriage Management www.ipaswomancare.com Questions? Papaya Model Demonstration and Practice to Follow