The Unified - ascls-ga
advertisement

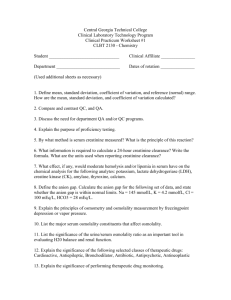
Signs, Symptoms, Complications Selling Sickness Carbohydrates Pancreas Type I vs Type II Diabetes Water/Osmolality/Electrolytes Acid-Base Disorders Lipids Heart Disease Renal Disease http://memekid.com/funny-chemistry-cat-memes.htm http://www.md-reasons.info/2014/07/diabetes-complications-of-diabetes.html Ill Defined Diseases Affect numerous people High Cholesterol and Diabetes Drug Companies Profits Expand boundaries of illness New customers Diabetes Before 1997 Diabetes diagnosis fasting blood glucose > 140 mg/dL After 1997 Diabetes diagnosis fasting blood glucose > 126 mg/dL Cholesterol Before 1998 High Cholesterol > 240 mg/dL After 1998 High Cholesterol > 200 mg/dL Increased new customers by 86% Lifestyle changes Diet and Exercise Types of Energy the body can use Carbohydrates Proteins Lipids Carbs are Good Carbohydrates Glycemic index Insulin Response Definitions Glycolysis Glycogenesis Glycogenolysis Gluconeogenesis – ATP and Pyruvate http://www.rogerspeakperformers.com/2012/the-glycemic-index/ Anatomy of a Pancreas Exocrine – digestive enzymes amylase and lipase Increased in pancreatitis (lipase more specific) Endocrine - Islets of Langerhans Beta Cells – Insulin Alpha Cells – Glucagon Delta Cells – Somatostatin Insulin Allows glucose to enter cells Only hormone than can decrease glucose levels Glucagon Primary hormone responsible for elevating glucose levels http://www.medicinenet.com/image-collection/pancreas_picture_1/picture.htm When the body has an excess of glucose it will go through the process of: A) Decreasing cell membrane permeability B) Gluconeogenesis C) Glycogenesis D) Glycogenolysis Glucagon acts by: A) Increasing glycogenolysis B) Increasing glycogenesis C) Increasing glycolysis D) Inhibiting glycogenolysis PANCREAS REVIEW Type I AKA insulin dependent diabetes (IDDM) Mostly young and thin Little to no insulin produced – autoimmune destruction Diabetic ketoacidosis - common Lab findings • Blood glucose levels 300-500 mg/dL • Ketonuria • Ketonemia • Decreased Na and Cl • Increased K • Slightly increased osmolality Type II non insulin dependent diabetes (NIDDM) Most common form found in mostly older and obese adults Combination of Insulin resistance and Insulin production issues Diabetic ketoacidosis – rare Hyperosmolar coma Lab findings Blood glucose levels >1000 mg/dL Greatly increased osmolality http://www.psychiatrictimes.com/metabolic-disorders/metabolic-monitoring-patients-antipsychotic-medications/page/0/4 Glucose – serum, plasma, whole blood Preferred diagnosis test is fasting plasma glucose (fasting 10 hours prior) • Reference range 70 -110 mg/dL Glycosylated hemoglobin or HbA1C – average glucose over 3 months Whole blood EDTA tube Ketone levels – serum or urine – acetest sodium nitroprusside (detects acetoacetic acid) Microalbuminuria – minute concentrations of albumin in urine (early signs of nephropathy) http://blog.diabetesms.com/?cat=3 Jane Doe is a 55 year-old-female. Her lab results were: Fasting glucose 122 mg/dL Fasting triglycerides 144mg/dL All other lab tests were normal. The doctor ordered a 2 hour OGTT. The 2 hour glucose tolerance test result was 228 mg/dL. These results indicate: A) Results are normal B) Diabetes mellitus C) Hypoglycemia D) Ketoacidosis CARBOHYDRATES REVIEW Monitoring long-term glucose control in patients with adult onset diabetes mellitus can best be accomplished by: A) Urine microalbumin B) Glucose tolerance testing C) 2-hour postprandial serum glucose D) Glycosylated hemoglobin CARBOHYDRATES REVIEW Average Water Content of the Human Body is 40% to 75% of total body weight. Intracellular fluid – two-thirds of total body water Extracellular fluid – one-third of total body water (Intravascular and extravascular fluid) Intravascular fluid plasma (93% water) Carries proteins, electrolytes, nutrients, hormones, wastes What must be kept in a constant concentration in the body is: Electrolytes (ions) pH (acid-base balance) Water http://www.apswater.com/article.asp?id=129&title=What+are+the+chemical+properties+of+water? Is a physical property of solution that is based on the concentration of solutes (particles) per kilogram of solvent Calculated osmolality (mOsmol / kg H20) = 2 [Na+ ] + [glucose] /20+ [BUN]/3 Measured Osmolality is done using freezing point depression Reference Range Serum 275-295 mOsm/kg General indicator of water volume Plasma osmolality directly effects the hypothalamus Increase osmolality increases thirst Increase osmolality increases ADH secretion from the posterior pituitary Decreased osmolality decreases ADH secretion Deficiency of vasopressin (ADH) Diabetes Insipidus Results in large volume of dilute urine Renin-angiotensin-aldosterone Stimulates sodium reabsorption and potassium excretion http://pixgood.com/adh-kidney.html Water deficit Osmolality increases (electrolytes concentrated) Increased thirst ADH is secreted • Increases water reabsorption Aldosterone is inhibited • Less sodium reabsorbed = decrease in electrolytes Water overload Osmolality decreases (electrolytes diluted) Thirst suppressed Aldosterone secreted • Sodium is reabsorbed = increase in electrolytes Remember two basic types of dehydration Dying of thirst in the desert – losing more water relative to electrolytes • Lab findings – all electrolytes elevated o Hypernatremia o Hyperosmolality Vomiting and Diarrhea – losing more electrolytes relative to water • Lab findings – all electrolytes decreased o Hyponatremia o Hyposmololality https://www.cartoonstock.com/directory/t/thirsty.asp Anions have a negative charge Cations have a positive charge Extracellular fluid has a high concentration of Na+, Cl-, HCO3- Intracellular fluid has a high concentration of K+, Ca+, Mg+, PO4- Hemolysis is unacceptable for these tests Sodium – osmolality = blood volume Major extracellular cation 135-145 mEq/L Hyponatremia • With low serum osmolality – diarrhea, vomiting, diuretics • With normal serum osmolality – in vitro hemolysis • With high serum osmolality – hyperglycemia Hypernatremia • Dehydration, diabetes insipidus (dilute urine), hyperaldosteronism Potassium – myocardial contraction Major intracellular cation 3.4 – 5.0 mmol/L (20X greater inside cell than outside) • HEMOLYSIS IS UNACCEPTABLE Both high and low levels will stop the heart Hypokalemia • Vomiting, diarrhea, hyperaldosteronism Hyperkalemia • Hyperglycemia, hypoaldosteronism (Addison’s disease) Chloride – maintain electrical neutrality (chloride shift) Major extracellular anion 98-106 mmol/L Passively follows sodium increased and decreased in the same conditions Sweat chloride test for cystic fibrosis – iontophoresis/pilocarpine http://www.cdha.nshealth.ca/pathology-laboratory-medicine/clinical-chemistry/hemolysis Bicarbonate (HCO3-) – buffering system maintain pH Second most abundant anion in extracellular fluid 22-29 mmol/L Measured as total CO2 • 90% of total CO2 is bicarbonate Acid base imbalance • Decreased metabolic acidosis • Increased metabolic alkalosis Exposure to air will decrease CO2 Electrolytes analysis Ion selective electrode – potentiometry using Nernst equation Susceptible to protein build up Sodium analysis selective membrane Glass ion-exchange Potassium analysis selective membrane Valinomycin Chloride analysis selective membrane Ion exchange Carbon dioxide (bicarbonate) PCO2 electrode http://chemwiki.ucdavis.edu/Analytical_Chemistry/Analytical_Chemistry_2.0/11_Electrochemical_Methods/11B%3A_Potentiometric_Methods Anion Gap Difference between unmeasured anions and unmeasured cations The anion gap is calculated as follows: [Na+] – ([Cl- ] + [HCO3- ]) or ([Na+] + [K+ ] ) – ([Cl- ] + [HCO3- ]) Reference range: 10-20 mmol/L Used as a form of QC High anion gap common in ketoacidosis Hyponatremia with a high osmolality is most commonly seen in A) Diarrhea B) Renal Failure C) In Vitro Hemolysis D) Hyperglycemia In dehydration which of the following hormones is responsible for increasing water reabsorption in the tubules: A) Antiduretic Hormone B) Aldosterone C) Rennin D) Thyroxin WATER ELECTROLYTE OSMOLALITY REVIEW Bicarbonate-carbonic acid buffer system Normal pH reference range is 7.35-7.45 pCO2 (35-45 mmHg) HCO3 (22-26 mmol/L) CO2 ≈ acid As CO2 increases = pH decreases As CO2 decreases = pH increases HCO3- ≈ base As HCO3- increases = pH increases As HCO3- decreases = pH decreases http://groups.csail.mit.edu/medg/people/psz/PatilThesis81/Patil81_ch1.html Acidosis or Alkalosis Determine what is causing the problem Respiratory or Metabolic (renal) Respiratory problem If pH and PCO2 are opposite each other • pH PCO2 • pH PCO2 Metabolic problem If pH and HCO3- go up together or down together • pH HCO3- • pH HCO3- Other normal system can then compensate (compensatory system) If Respiratory system • Hypoventilate • Hyperventilate If Metabolic system • Excrete or reabsorb H+ • Excrete or reabsorb HCO3- Look at compensatory system reference range for either HCO3- or CO2 Uncompensated (value within normal range) Partially compensated (value outside of normal range) Compensated (value outside of normal range and pH within normal range) Collection Heparinized syringe radial artery No Bubbles or exposure to air http://www.rtmagazine.com/products/blood-gas-analysis/ Break it down Acidosis or alkalosis? Problem organ system? Is the other system compensating? ABG problem Review pH 7.26 pCO2 16 mmHg HCO3- 7.1 mmol/L ABG problem Review pH 7.60 pCO2 25 mmHg HCO3- 24 mmol/L Unsaturated Fat 3 Saturated Fat Hydrogenation form of preservation Trans Fat Solid at room temperature https://www.flickr.com/photos/ fotoosvanrobin/11026441715/ http://www.med-health.net/OliveOil-Ear-Wax.html http://www.indiana.edu/~oso/Fat/trans.html Lipids Organic compounds insoluble in water Fatty acids Triglycerides Cholesterol Fatty Acids Body makes most Essential fatty acids -not made by the body • Omega 3 and Omega 6 Triglycerides Majority of what we eat Lots of calories Cholesterol Present in all cell membranes Building block of bile and steroid hormones Liver makes most of what we need Fat stored as Triglycerides in adipose tissue Lipolysis – break down of fat for energy Ketone bodies Lipoproteins from largest (least dense) to smallest (most dense) Chylomicrons • Largest lipoprotein least dense • Transport dietary lipids from the small intestine to the liver • Causes turbidity in serum VLDL • Contains mostly triglycerides • Transports triglycerides from the liver to peripheral tissue LDL • Delivers cholesterol to cells • Contains mostly cholesterol • BAD cholesterol associated with Apoliprotein B • High levels of LDL and Apo B risk of heart disease HDL • Removes cholesterol out of cells • GOOD cholesterol associate with Apoliprotein A • High levels of HDL and Apo A risk of heart disease http://dolinabiotechnologiczna.pl/diagnostyka-laboratoryjna-2/ratunku-lipemia/ Which of the following lipoproteins is the major carrier of cholesterol to peripheral tissues? LIPID REVIEW A) VLDL B) LDL C) HDL D) Chylomicrons True or False: Increased levels of apolipoprotein A-I are associated with increased risk of coronary artery disease. http://investorplace.com/2014/03/bacon-smell-oscar-mayer-aapl-stock-krft-stock/#.VT01CWN8MXk Lipid panel includes (fasting 10-12 hours) Total cholesterol - measured LDL – calculated using Friedewald calculation • LDL = total cholesterol – (HDL + VLDL) • Invalid Trig > 400 mg/dL HDL - measured Triglycerides – measured • High levels increase risk of pancreatitis Arteriosclerosis – hardening of the arteries If it affects the heart called Coronary Artery Disease http://healthinformatics.wikispaces.com/Balloon+Angioplasty Initial Cardiac Panel includes: Troponin - Most specific cardiac marker • Troponin I (TnI) increases 4 hours normal after 6 days • Troponin T (TnT) increases 4 hours normal after 7 days Total CK – nonspecific marker • Found in all muscle increased in rhabdo, MD CK-MB (isoenzyme)– second most specific cardiac marker • Peaks in 1 day returns to normal in 2 days Myoglobin – least specific marker • Sensitive rises within 1 hour returns to normal in 1 day • Early indicator • Not included on subsequent cardiac panels only initial http://dietchoices.com/diet-plans/heart-attack-grill-diet/ Which of the following tests monitors inflammation levels that may contribute to acute coronary syndromes? A) hs-CRP B) Troponin I C) BNP D) Total CK HEART DISEASE REVIEW hsCRP – high sensitivity C-reactive protein Measures inflammation related to stress (cortisol) • Increased hsCRP = increased plaque formation BNP – B natriuretic peptide Increased in CHF Elimination of waste Urea • Protein degradation = ammonia =urea Creatinine Waste product of creatine • Jaffe reaction o Ketones positive interference Falsely elevate creatinine levels • Uric Acid Final product of purine metabolism • Monosodium urate crystals synovial fluid = gout o Polarized microscope • Glomerular Filtration Rate 24 hour urine Creatinine Clearance Creatinine Clearance = U S x V 24V x 1.73 SA Normal Kidneys Serum • Normal levels of BUN and Creatinine Urine • Concentrated • High in BUN and Creatinine • Little to no protein Abnormal Kidneys - Renal Failure Serum • High levels of BUN and Creatinine Urine • Dilute low specific gravity • Low in BUN and Creatinine • High in protein o Microalbuminuria – early indicator diabetic nephropathy o Renal failure will result if diabetes is not well managed http://www.rayur.com/acute-renal-failure.html Bishop, M.L., Fody, E.P., & Schoeff, L. E. (Edward P Fody MD). Clinical Chemistry: Principles, Tehcniques, and Correlations. Philadelphia: Lippincott Williams & Wilkins. Moynihan, R., & Cassels, A. (2006). Selling Sickness: How the World’s Biggest Pharmaceutical Companies Are Turning Us All Into Patients. New York: Nation Books.