Informed consent: The Process
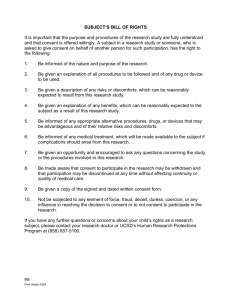
advertisement

Wendy Lloyd BA, LPN, CIP,CCRP Regulatory Affairs and Compliance Specialist Identify consent process requirements Distinguish between IRB, PI/Designee consent process responsibilities Identify with what went wrong? Audit results, FDA Warning Letters and OHRP Determination Letters Summarize tips to avoid deficiencies "A word is not a crystal, transparent and unchanged; it is the skin of a living thought and may vary greatly in color and content according to the circumstances and the time in which it is used" — Oliver Wendell Holmes Jr. DHHS – 45 CFR Part 46 FDA 21 CFR Part 50 (Informed Consent) Part 56 (IRB) No investigator may involve a human being as a subject in research covered by these regulations unless the investigator has obtained the legally effective informed consent of the subject or the subject's legally authorized representative The information that is given to the subject or the representative shall be in language understandable to the subject or the representative and include the elements of consent An IRB shall require that information given to subjects as part of informed consent is in accordance with 50.25. The IRB may require that information, in addition to that specifically mentioned in 50.25, be given to the subjects when in the IRB's judgment the information would meaningfully add to the protection of the rights and welfare of subjects. Detailed description of the method for obtaining informed consent All informed consent documents submitted for IRB approval Changes in ICD’s are submitted as amendments Consent must contain all required elements Consent is documented in writing through the use of a current IRB-approved ICD, unless waived PI assures the informed consent process in research is an ongoing exchange of information throughout the course of the research and it is documented Fetuses, Pregnant Women, and Human In Vitro Fertilization Prisoners Children Elderly Cognitively Impaired Minorities Etc. FDA Mandates ICH/GCP 4.8 suggests FDA has no regulations concerning delegation of consenting although it is discussed in the FDA Information Sheets FDA only requires that a copy of consent be provided to subject consent is obtained the same day that the subject's involvement in the study begins, the subject's medical records/case report form should document that consent was obtained prior to participation in the ICH allows the delegation of the informed consent process to a designee ICH recommends the person conducting the informed consent process sign and date the consent form ICH recommends that the subject receive a signed and dated copy of the consent form If research“FDA Consent information sheet” FDA and ICH BOTH require the IRB to review The informed consent, process, protocol, advertisements, and the Investigator's Brochure ICH/GCP 3.1 also recommends IRB submission of: Subject recruitment procedures Written information provided to subjects Information about subject compensation Investigator's current CV and/or other documents evidencing qualifications DHHS OHRP FDA Other Federal Agencies (NIH, CDC and CMS State Law Institution IRB Policy Policy IRB Policy Department Policy Research Team SOP’s Study Protocol/ Contract Depending on funding ICH/GCP A document that provides a summary of the research and explains the subjects rights as a participant It is designed to outline and be a reference regarding what is expected of the participant Disclosure of relevant information to prospective subjects about the research; their comprehension of the information, and their voluntary agreement, free of coercion and undue influence, to research participation. http://ohsr.od.nih.gov/info/sheet6.html Simplicity Summary QOL How many adverse events? How many visits? Know how many subjects are on study? This dose Different dose Cognition/capacity Level of education Social/cultural values Language Age Environment Anxiety/fear Pain Influence of medications Quality of disclosed information Readability of informed consent “the belief that the purpose of a clinical trial is to benefit the individual patient rather than to gather data for the purpose of contributing to scientific knowledge” The subject believes that his medical needs will determine his assignment to a treatment group or the PI will modify the protocol to serve his own medical need. The subject has unreasonable expectations about the likelihood of benefit from study participation. In this example the subject believes the PI will not administer treatment that might harm them, but rather, will provide interventions that only help them. Harris Interactive Online Studies of 2031 and 2261 adults Only a minority of the public is confident that clinical trials subjects are not treated like guinea pigs do not suffer more pain or side effects than with standard of care treatment receive high quality care receive honest accurate information 2002 24% 2005 54% 13% 32% 25% 53% 48% However 83 % believe it is essential and very important all new pharmaceutical products be tested on humans before they are approved for general use www.harrisinteractive.com/news/allnewbydate.asp?NewsID=213 www.harrisinteractive.com/news/allnewbydate.asp?NewsID=941 2,261 US adults over 18 surveyed online April 2005 I understood that participation was voluntary. I understood that I was agreeing to participate in a clinical research study. I fully understood what was required of me (number of visits, how long the study lasted, etc.). I knew I could stop participating in the study at any time. I felt comfortable asking additional questions regarding the study. I was assured confidentiality of all personal information that I provided, with the exception of those allowed by federal law. I felt secure that my confidentiality was protected throughout the study. I was made aware of the benefits involved in participating in the clinical research study. I was made aware of the risks involved in participating in the clinical research study. I understood that I could choose other treatment options, including no treatment at all. The informed consent document was easy to read and understand. 2004 % 90 2005 % 84 89 83 81 78 79 75 79 75 73 73 71 69 74 68 74 65 66 63 60 61 www.harrisinteractive.com/news/allnewsbydate.asp?NewsID=941 2,261 US adults over 18 surveyed online April 2005 % Said purpose of the study was "clear" after reading the informed consent 85 Agreed their questions were answered by the study team regarding the informed consent process 80 Said the study coordinator conducted the informed consent process. 54 Read the informed consent by themselves 48 www.harrisinteractive.com/news/allnewsbydate.asp?NewsID=941 Non compliance Complaints to the IRB, the institution, the OHRP or the FDA ME NIH Research Team Compliance Officer Institutional Official Government Public Members COG Family Advocates FDA YOU Sponsor Investigator Educators Auditors IRB Chair and Translator Press / Media Pharmacist DOD OHRP The person must be trained regarding informed consent process and be knowledgeable about study FDA Requirements: IRB must know who will conduct consent process FDA does not require the that the PI personally conduct the consent process. ECOG Requirements: “Legally, it is the physician’s responsibility to discuss the study with the patient and obtain the written consent.” “After an initial discussion it may be the physician, nurse, or CRA who provides further details to the patient.” 7.2.6 “Presenting the Consent Form to the Patient,” ECOG Protocol Management Ongoing Interactive process Different for every subject Different for every study Essential for study success IRB approved Providing clear definition between where standard of care leaves off and research begins Allows re-education Requires re assessment of subject understanding with each visit Emergency, life threatening situation that requires intervention Minimal risk study with IRB approval Although the regulations place the burden of responsibility on the PI, the protection of human research subjects is a shared responsibility among all research professionals involved in the conduct of the study Members of a research team have a moral obligation to uphold the ethical and regulatory standards by which human subjects research is conducted Ultimate protector of the subject’s rights and safety Be personally certain that each subject is adequately informed and freely consents to participate in the investigator’s research Assure that every reasonable precaution is taken to reduce risk to a minimum for the subject The investigator is responsible for whom he delegates authority to Follow the protocol Obtain consent before initiating ANY studyspecific procedures Provide a quiet, comfortable, and private setting Explain the consent procedures and process to the subject Ensure sufficient time to consider all options Access the subject's reading abilities, cognitive status now and throughout study Requires accessing subjects understanding Ensure the subject is the one who wants to participate, free from coercion or other undue influence Consistent with IRB approved process Provide additional safeguards as required Provide new information promptly Provide a copy of the consent document and each revised consent document to the subject Document process and response from patient Establish a relationship with the subject Provide privacy Assess views on research vs. standard of care Keep the subject in the center of the process Be an active listener Ask open-ended questions Be aware of non-verbal messages Empathize with the subject’s concerns Be a teacher by educating the subject and verifying his understanding of the research study Assure withdrawal is possible at ANY time Inform other options are available Be available anytime for any question Do not rush the process or the subject Know the protocol Introduce yourself and state who referred you Do not depend on subject enrolling You are not a salesman Provided consent document for review Methods of conveying information differs Check list Read consent to subject Read highlights /review calendar Video Electronic Web-based resources Informed Consent Worksheet Date of Consent:__________________ Name of Study:_____________________________ IRB Study Number:__________________________ Patient Name:_____________________ Patient MRN:_________________ _Study ID#:__________ The following has been explained to the potential study subject, and the subject has been offered the opportunity to ask questions regarding the study: TOPIC COMMENTS Purpose of the study _________________________________ Qualifications to participate _________________________________ Location and participants _________________________________ What will happen during the study _________________________________ Risk and benefits _________________________________ Study related injury or illness _________________________________ Alternative treatments _________________________________ Confidentiality _________________________________ Study costs _________________________________ Compensation _________________________________ Who to contact with questions _________________________________ Voluntary participation _________________________________ Termination of participation _________________________________ Questions or comments: __________________________________________________________________ __________________________________________________________________ Does the patient state an understanding of the study and procedures and agree to participate? ___yes ___no _____________________________________ Person administering consent Signed copy given to patient? ___yes ___no __________________________ Date / Time Copy in patients chart? ___yes ___no INFORMED CONSENT & RECONSENT Clinical Research Trial: ________________________________ PRESENTATION CHECKLIST Version Date:________________ Physician discussed diagnosis and treatment options (standard of care, no treatment) Physician discussed clinical research trial including the following: • Description of the clinical research trial, its goals, and medications involved • Voluntary participation • Anticipated duration of participation • All known risks: reported side effects and management of known side effects and… • Possibility of unknown side effects • Potential and reasonable expected benefits • Treatment groups and randomization (if applicable) • Required study procedures • Follow-up after completion of study treatment • Rights and responsibilities of research participants (including contraception if applicable) • Confidentiality • Compensation / Additional Costs Consent presented to patient / legal representative / legal guardian Time allowed for patient / legal representative / legal guardian to read consent and ask questions prior to signing consent Patient / legal representative / legal guardian acknowledged understanding of the clinical trial and indicated questions were answered to their satisfaction Patient / legal representative / legal guardian signed informed consent Patient / legal representative / legal guardian received a copy of each signed research consent form Study specific procedures were not done prior to consent being signed Contact information provided to patient / legal representative / legal guardian for study related concerns Performance Status today (per protocol): Karnofsky / __________ Lansky ECOG / Zubrod / WHO ___________ Consent document(s) signed on: / / Amount of time explaining the consent:________________ Time consent signed:_______ AM/PM **Translation Services: Translated document(s) and / or interpreter provided as needed: q NO (translation services not needed) _____ YES List language provided:______________________ Any additional comments regarding translation:____________________________________________ Physician’s Signature (print name):____________________________________Physician (sign): Date:________________________ Ask if problems arose since last visit (A/E’s) Provide new information if applicable Encourage questions each visit Talk about what comes next Re-assess subjects desire to continue each visit Assess compliance (diary, meds etc) If subject regains cognitive ability New information becomes available Significant protocol changes New surrogate is identified IRB instructs you to re-consent Investigator has the option to re-consent for longitudinal data collection time points Method of presentation Voluntary participation Environment Complete explanations Length of time devoted to the process Simple explanations Adequate time offered to ask questions How subject demonstrates understand of the study and desire to participate Promptness of reporting new information You know you want to: Volunteer to have your consenting process observed Contact Wendy Lloyd by phone (936-7106) or by email (wendy.lloyd@vanderbilt.edu) in advance or just prior to consenting If SOP’s exist are they followed? Confirm consent process documentation Implementation of changes only after IRB approval Correct version non expired consent used All options completed by subject Consent signed and dated by all parties Consent signed prior to ANY procedures Consented by trained individuals Signatures of subject and consenting person on different dates Consent and study procedures on same date Consent was performed by an untrained or unqualified care provider Person consenting is not listed as KSP Check boxes within the consent incomplete Crossed out sections or white out used in the IRB approved consent Unable to locate consent for subject on study Subjects not re-consented with revised consent as instructed Ineligible subjects enrolled Multiple consent documents for same patient with no explanation why Person consenting did not state the purpose or procedures of the study Consent document left on clip board for subjects to complete and return to nurse if interested Person consenting the subject did not sign the form Confirm all personnel consenting subjects are KSP Document training and qualifications of all KSP Establish one place to retrieve ONLY the latest IRB approved consent Conduct random audits of the consent documentation Review the FDA Warning Letters and FDA IRB Information Sheets –“A Guide to Informed Consent” Become familiar with the Regulations, state law, institutional and IRB Policies Know the protocol Only do what you are trained to do Volunteer for consent observation Ask subjects if they felt fully informed Seek education Stay organized If you find something don’t hide it Network Become certified If you don’t know ask January 19 – PI failed to obtain ICD for subjects (? Number), During response PI gave ICD to FDA not IRB approved January 28 – PI failed to obtain consent with complete study info, conducted lab tests for two subjects without consent February 18- PI failed to consent 1 subject (hand writing not subjects), enrolled 4 ineligible subjects February 24 – PI failed to obtain legally authorized ICD: child was enrolled with 1 parent signature, child was in DHS custody February 25 – PI failed to obtain legally authorized consent; implemented changes in the investigational plan without approval March 2 – 7 of 25 subjects met EXCLUSION criteria, failed to properly consent 3 subjects, 1 was told would receive investigational device but received control device March 18 – PI failed proper monitoring of the investigational study March 10 – PI failed to notify subjects following study participation regarding safety events March 21- PI failed to consent 2 subjects, 4 ineligible subjects enrolled March 24- IRB approved protocol allowing consent following study procedures instead of before April 1- PI failed to consent 1 subject, response letter found consent but it was visibly altered and the PI did not alter it. June 28 – PI failed to consent with updated consent for 7 subjects, enrolled 7 subjects who were ineligible. January 28 – IRB did not document specific criteria when approving waiver or alteration of consent January 29 – IRB did not waive consent for subjects, PHI was obtained from family members and the approved consent did not contain the appropriate risk language April 8 – PI retain PHI on subject for a study without approval or consent. PI also implemented study changes (a 3rd intervention) without IRB approval June 3 – PI decided not to inform subjects of new drug information since they had completed the study and PI did not conduct all follow-up visits (although subject was in the office) per protocol requirements Nov 24 – IRB approved research involving pregnant woman/fetus that held the prospect of direct benefit to the fetus. Only one signature line was on the consent instead of the required two. IRB also approved telephone and electronic consents for studies however did not properly waive documentation or alteration of consent. May 10- subject complained he was encouraged to continue a study he did not wish to continue in Each interaction is different because every subjects, circumstance, question, communication style is different. It is up to each one of us to take the consent process serious and fully inform each subject By possibly increasing subject recruitment and retention on a wide scale Playing a substantial role in shaping public perceptions of the value of clinical research For federal guidance on obtaining informed consent of human research subjects, see the following websites: General requirements for informed consent http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=50.20 http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=50.23 http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=50.24 http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=50.25 Documentation of informed consent http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=50.27 Research involving pregnant women, fetuses or neonates http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.204 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.205 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.206 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.207 Research involving children (also found in 21 CFR 50.50-56) http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.404 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.405 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.406 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.407 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.408 http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.409 Pediatric research “assent”decision matrix http://www.hhs.gov/ohrp/panels/407-01pnl/riskcat.htm Office for Human Research Protections (OHRP) informed consent tips http://www.hhs.gov/ohrp/policy/index.html OHRP informed consent FAQ http://answers.hhs.gov/ohrp/categories/1566 Vanderbilt IRB Policy http://mcapps01.mc.vanderbilt.edu/IRB/policy&procedures.nsf/(WebTa bleOfContents)/8AF759048966C29D86257731005ECD1F?OpenDocument If you have additional comments or questions feel free to contact me Wendy Lloyd Wendy.lloyd@vanderbilt.edu 615-936-7106