Introduction to Evidence-based Practice Resources for HINARI Users
advertisement

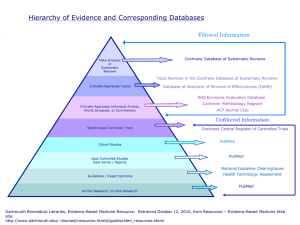
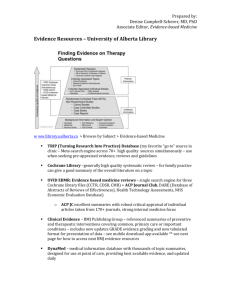
Evidence-based Practice Resources for HINARI Users (Module 7.2) Evidence-based Practice Resources for HINARI Users Instructions - This part of the: course is a PowerPoint demonstration intended to introduce you to Evidence-based Practice and related HINARI resources. module is off-line and is intended as an information resource for reference use. Table of Contents • Evidence-based Medicine (EBM) definition, background and resources • Clinical Evidence • Cochrane Library • EBM Guidelines • BMJ Practice • HINARI EBM Journals • Searching for EBM articles in HINARI/PubMed’s Clinical Queries and Limits • Other Resources • Summary Evidence-based Practice (EBP) Definition "Evidence-Based Practice requires that decisions about health care are based on the best available, current, valid and relevant evidence. These decisions should be made by those receiving care, informed by the tacit and explicit knowledge of those providing care, within the context of available resources." Sicily statement on evidence-based practice. BMC Medical Education, 2005 Jan 5;5(1):1 What is EBP? • The integration of best evidence* from current research, patient preferences and values, and clinical expertise to clinical questions (Sackett, 2000) in a timely fashion. Best Evidence EBP Patient Values/Local Conditions Clinical Expertise *Best available evidence is: consistent research evidence with high quality and quantity Why EBP? • To improve care – To bridge the gap between research & practice – “Kill as few patients as possible” (O. London) – A new treatment might have fewer side effects. – A new treatment could be cheaper or less invasive – A new treatment may be necessary in case people develop resistance to existing therapies, etc. • To keep knowledge and skills current (continuing education) • To save time to find the best information How does EBP help? A patient comes to a clinic with a fresh dog bite. It looks clean and the nurse and patient wonder if prophylactic antibiotics are necessary. The nurse searches PubMed and found a meta analysis indicating that the average infection rate for dog bites was 14% and that antibiotics halved this risk to 7%. • For every 100 people with dog bites, treatment with antibiotics will save 7 from infection • Treating 14 (NNT) people with dog bites will prevent 1 infection • You explain these numbers to the patient along with possible consequences and patient decides not to take antibiotics. On a follow up visit you find out that he did not get infected. Glasziou P, Del Mar C, Salisbury J. EBP Workbook, 2nd. ed. BMJ Books, 2007. What are some Barriers for EBP? • • • • • • Overuse, underuse, misuse of evidence Time, effort, & skill needed Access to evidence Intimidation by senior clinicians Environment not supportive of EBP Poor decision making The 5 Step EBP Process 1. ASK: Formulate an answerable clinical question 2. ACCESS: Track down the best Evidence 3. APPRAISE: Appraise the evidence for its validity and usefulness 4. APPLY: Integrate the results with your clinical expertise and your patient values/local conditions 5. ASSESS: Evaluate the effectiveness of the process Ask Assess Access Apply Appraise Step 1: ASK a focused (answerable) clinical question Ask • Background questions (What do I know about this?) • Foreground (Clinical) Questions P = Patient, population or problem (Who are the patients or populations? What is the disease?) I = Intervention (What do you want to do with this patient (e.g. treat, diagnose, observe)? C = Comparison intervention (What is the alternative to the intervention (e.g. placebo, different drug, nothing?) O = Outcome (What are the relevant outcomes (e.g. morbidity, mortality, death, complications)? Why should I use PICO? • • • To help define problem in clarify it in your own mind To prepare for searching To ask patient centered questions. Treatment of Pneumococcal Pneumonia SHOULD be different for – Terminal Cancer Patient – Elderly, Severely Demented Patient – Young, mother of 2 children • Developing the question requires: – Some background knowledge of the condition – Understanding of the patient and what are the outcomes and beliefs that matter to this patient • Death? Disability? Quality of life? Cost? Improvement of symptoms? Example: Intervention Questions • Identify background questions, create a PICO and a focused clinical question for this case: 54 year old male patient was diagnosed with intermediate grade prostate cancer and wants to know whether to get a radical prostatectomy or radiation treatment. He is concerned about death from prostate cancer and also risks of impotence and incontinence. Formulate the Clinical Question • PICO P - 54 year old male with intermediate grade prostate cancer I - radical prostatectomy C- radiation treatment O- reduce risk of mortality, impotence, and incontinence • Focused clinical question In 54 year old male patients with intermediate grade prostate cancer is radical prostatectomy more effective compared to radiation treatment in reducing the risk of mortality, impotence, and incontinence? EBP Step 1a: Classify the type of the question • What is the treatment? Question of INTERVENTION/PREVENTION • What causes the problem? Question of ETIOLOGY, RISK • Does this person have the problem? Question of DIAGNOSIS • Who (and how likely) will get the problem? Question of PROGNOSIS Etiology and Risk Questions What causes a disease or health condition? • The reverse of intervention questions-they deal with harmful outcomes of an activity or exposure (public health issues) • Develop a clinical question for the case: S. is a smoker and just found out that she is 3 months pregnant. She quit smoking immediately. But she is worried if her developing baby was harmed and if the baby is at risk for having developmental problems. She is asking you if smoking during the first trimester can harm her baby? Etiology or Risk Questions • P-babies of mothers who smoke I-smoking in first trimester C-nothing O-increase risk of developmental problems • Question: Are babies of mothers who smoke during their first trimester at an increased risk of developmental disabilities? Diagnosis Questions • These questions are concerned with how accurate a diagnostic test is in various groups and in comparison to other tests or usually to a “gold standard test”. As part of your clinic assessment of elderly patients, there is a hearing check. You think that a simple whispered voice test is very accurate compared to other methods. You want to do a literature search. What is your question? (1) Glasziou P, Del Mar C, Salisbury J. EBP Workbook, 2nd. ed. BMJ Books, 2007. Example • P-elderly people I-whispered voice test C-no test (or other tests) O-accurate diagnosis of hearing problems • Question: In elderly people, does the whispered voice compared to other tests give an accurate diagnosis of hearing problems? Glasziou P, Del Mar C, Salisbury J. EBP Workbook, 2nd. ed. BMJ Books, 2007. Templates for EBP Questions • For a therapy: In _______(P), what is the effect of _______(I) on ______(O) compared with _______(C)? • For etiology: Are ____ (P) who have _______ (I) at ___ (Increased/decreased) risk for/of_______ (O) compared with ______ (P) with/without ______ (C)? • Diagnosis or diagnostic test: Are (is) _________ (I) more accurate in diagnosing ________ (P) compared with ______ (C) for _______ (O)? • Prevention: For ________ (P) does the use of ______ (I) reduce the future risk of ________ (O) compared with _________ (C)? • Prognosis: Does __________ (I) influence ________ (O) in patients who have _______ (P)? Melnyk B. & Fineout-Overholt E. (2005). Evidence-based practice in nursing & healthcare. New York: Lippincott Williams & Wilkins. EBP Step1b: Decide on the best type of study for question For each type of question there is a hierarchy of evidence Therapy/Prevention RCT>cohort > case control > case series What should I do about this problem? Diagnosis Does this person have the problem? Etiology/Harm cross-sectional study with blind comparison to a gold standard RCT > cohort > case control > case series What causes the problem? Prognosis/Prediction Who will get the problem? RCT >cohort study > case control > case series Frequency and Rate cohort study > cross-sectional study How common is the problem? NOTE: A well designed systematic review of RCTS (randomized controlled trials) is best as it is least biased therefore more valid. Hierarchy of Study Designs for Intervention Least • Randomized Controlled Trial Experimental • Cohort Studies Observational • Case-Controlled Studies Observational • Case reports/Clinical Observations Observational Bias Most Bias To recognize the type of study ask the questions: 1. Is intervention randomly assigned? Yes-RCT; No-Observational study 2. When were the outcomes determined? • After the exposure-cohort study (prospective study) • During the exposure-cross-sectional study • Before the exposure-case-control study (retrospective study based on recall) EBP Step 2: ACCESS Track Down the Best Evidence Access 1. Start “hunting” from the best resource: Match your question to the best medical information resource for this question. • Well designed Systematic Reviews¹ can be a great place to start they contain commentary about validity ¹A systematic review involves the application of scientific strategies, in ways that limit bias, to the assembly, critical appraisal, and synthesis of all relevant studies that address a specific clinical question. Cook DJ, Mulrow CD, Haynes RB. Annals of Internal Medicine March 1, 1997; 126 (5) 376. Track Down Hierarchy of Evidence- Access evidence at the level that will give you the best evidence Filtered & Critically Appraised Expert Opinion and Not Filtered Background info. Most clinically relevant (at the top) Least clinically relevant (at the bottom) Why not get info only from textbooks and review articles? • Texts and review articles? – Dated – perhaps by several years – Often biased • Author chooses article that he/she agrees with (or has written) • Author chooses articles of his/her friends • Author does not identify all the relevant literature • Review’s methods are not explained • These resources help with background knowledge (learn about disease) not foreground (answer the specific clinical question for this patient) Why not get info only from guidelines? • They can assure standards of care but: – Can be biased – May not always be developed by experienced experts – Are not always evidence-based – Can work for most patients but not for all – Can work in some circumstances but not in all – Can be dated – There may not be guidelines for everything Filtered and Critically Appraised Evidence-Based Resources • The Cochrane Library by The Cochrane Collaboration via Wiley – Independent non-for-profit international collaboration – Reviews are among the studies of highest scientific evidence – Minimum Bias: Evidence is included/excluded on the basis of explicit quality criteria – Reviews involve exhaustive searches for all RCT, both published and unpublished, on a particular topic – Abstracts searchable for free on the Internet; complete database is available via HINARI for most countries – 1995- Benefits for using not-evaluated databases for EBM research (PubMed, Cinahl) • • • • Create comprehensive search strategies Conduct systematic reviews of the literature Conduct synonym searching utilizing thesauri Set up and distribute alerts relating to evidencebased medicine • Limit to specific populations & publication types • Utilize EBM built-in filters (search strategies) EBP Step 3: Appraise: Appraise Determine if the results are valid and useful • Appraisal principles (primary and secondary research) – What is the PICO of the study? Does it match my question? – How well was the study done? Is it biased? – What do the results mean? Are they real and relevant? • More: University of Oxford’s Center of EBM: http://www.cebm.net/index.aspx?o=1157 • Tools for evaluating studies can be found in the Evaluating the Evidence section in the EBM tutorial at: http://www.hsl.unc.edu/Services/Tutorials/ebm/welcome.htm EBP Step 4: APPLY: Integrate the results with your clinical expertise and your patient values Apply • Question to ask: – Is the intervention feasible in my settings? – What alternatives are available? – Is my patient so different then those in the study that the results cannot apply ? – Will the potential benefits outweigh the potential harms of treatment ? – What does my patient think? What are his cultural beliefs? – Individual decision making/group decision making/choice – Explaining risks and benefits to patients: https://docs.google.com/View?id=d7k3gkg_679hnvn54c8 • Visual Rx: http://www.nntonline.net/visualrx/ EBP Step 5: ASSESS Assess Evaluate the effectiveness of the process. How am I doing? • • • • Am I asking questions? Am I writing down my information needs? What is my success rate in the EBM steps? How is my searching going? Am I becoming more efficient? • Am I periodically syncing (checking) my skills and knowledge with new developments? • Teach others EBP skills • Keep a record of your questions Limitations of EBP • Limited scope of evidence-it will never be complete • The quality of research available • Keeping it patient centered, cost effective • Evidence from Randomized Controlled Trials for real life patients • Communicating uncertainties • Decision making If you are interested in learning more about EBM, go to the online tutorial Introduction to Evidence-Based Medicine from the Health Sciences Library, University of North Carolina (USA): http://www.hsl.unc.edu/Services/Tutorials/ebm/welcome.htm Logging on to HINARI 1 To access the HINARI Evidence-based Medicine resources, we must Login to the HINARI website using the URL http://www.who.int/hinari/ Logging into HINARI We will need to enter our HINARI User Name2and Password in the appropriate boxes, then click on the Login button. Note: If you do not properly sign on, you will not have access to Evidence-based Medicine resources that are located in the Reference Sources drop down menu. From the HINARI Reference Sources drop down menu, we also can find tutorials for learning more about EBM. In this example, we will link to BMJ Learning. From the BMJ Learning’s Browse our modules listing, we have clicked on Clinical Epidemiology and located four EBM-related tutorials. From the Reference Sources drop down menu, there are four valuable EBMrelated sites. First, we will click on the Clinical Evidence link, a resource for informing treatment decisions and improving patient care. It is published by the BMJ Publishing group. In the Clinical Evidence site, you can search by Sections, Full review list or (keyword) Search this site. Also note that there is a Clinical Evidence Userguide in multiple languages and links to the Latest updated reviews. Using the Search this site option, we have completed a keyword search for tuberculosis and identified 73 documents. The links include clinical evidence Guidelines, Keypoints, Interventions and Updates about this topic. We have further limited this search by combining tuberculosis and HIV. This has resulted in 56 documents. We will click on the link to Tuberculosis in people with HIV. The initial page of HIV: treating tuberculosis initially displays Interventions based on clinical questions. Note that also you have access to Key points, About this condition, Updates, Guidelines and References. We will click on the Guidelines hyperlink. The Guidelines page contains the title, name of organization and hyperlink to 10 documents from key health agencies. The guidelines have been sourced from the National Guidelines Clearinghouse (USA). We have clicked on the Full review list option and displayed the topics under the A alphabetical list. This A-Z subject access contains an extensive list of topics and clinical evidence material. From the Reference Sources drop down menu, we now will click on the Cochrane Library link. The Cochrane Library contains high-quality, independent evidence including reliable evidence from Cochrane and other systematic reviews and clinical trials. It is published by John Wiley. Note the full-text reviews are available to Band 1 only while Abstracts can be accessed by all users. The Cochrane Library COCHRANE LIBRARY : The Cochrane Collaboration. Oxford: Update Software; 1996-. Updated quarterly. • Cochrane Database of Systematic Reviews (CDSR) – High-quality pre-evaluated systematic reviews from all over the world – International, not-for-profit organization – Complete reviews and protocols (reviews that are still in progress) – CDSR abstracts are in Medline but there is no link to full-text of the review – Specific topics, explicit evaluation criteria to minimize bias The initial page of this site has a title, abstract or keyword option Search engine. You also can Browse Cochrane Database by broad subject heading . The initial page also highlights New and Updated Cochrane Reviews. We will go to the Advanced Search. Also from the initial page, there is a link to the Cochrane Journal Club. We have opened the Advanced Search option where you can specify search fields and have the ability to combine terms using AND/OR/NOT operators. In this text Advanced Search, we have combined diarrhea child* using the Search All Text option with the wildcard (*) used to locate the terms child and children. Note that you also can complete a MeSH Search, look at your Search History or Saved Searches. The Advanced Search results for diarrhea child* has retrieved 451 records from the Cochrane Database of Systematic Reviews. You have the option to Export All Results (save). Note: if the results of your search are too many, you can narrow it by limiting the keyword search to Title instead of Search All Text. The screen displays the Abstract of the first systematic review listed in the search - Oral zinc for treating diarrhoea in children. To access the full-text review, click on the Full PDF hypertext link in the left column. Other options are Summary and Standard. Also note the hypertext links to specific sections of the systematic review. We have displayed the Abstract of the systematic review that includes the Background, Objectives, Search strategy, Selection criteria, Data collection and analysis and Main Results. The final section of the Abstract is titled Plain language summary. This section is useful for disseminating the results to groups of health workers and patients. Also note the Main results and author’s conclusions (the ‘bottom line’) as these sections discuss the review’s results and how they should be used. We have displayed the PDF Full version of the Oral zinc for treating diarrhoea in children systematic review. Other options include Summary and Standard files. Note: The url that contains http://hinarigw.who.int/whalecom... shows that we have logged in to HINARI properly and will have access to the full-text version of this review. From the Advanced Search page of the Cochrane Library, we have clicked on the Cochrane Reviews: By Topic hyperlink. This has displayed the Topics for Cochrane Reviews. From this extensive list, you have another option for locating subject- specific material. Note that there are other search lists including an A-Z list, Updated Reviews and New Reviews. For more training material, you can click on The Cochrane Library Help hyperlink. We have opened the Search Manual. Another option is a listing of Web Updates. If your institution does not have access to Cochrane…. Access to the Abstracts is free from a link at: http://www.cochrane.org/ After accessing the Cochrane Collaboration (http://www.cochrane.org/), click on the Cochrane Library link. This will give you access to the Library’s search options and the abstracts but not the full-text articles. Click here We now access the third Reference Sources option for evidence-based health information - EBM Guidelines. This is the initial page of EBM Guidelines Evidence-Based Medicine. Also published by John Wiley, this resource is a collection of clinical guidelines for primary care combined with evidence-based research. You can Search by keyword or Browse database contents by EBM Guidelines, Evidence summaries, Pictures, Audio samples, Videos and Programs. We have completed a keyword search for Influenza. The results page includes summaries of the key issues including Related resources and References and links to important websites. Also included are links to the Evidence summaries. We have displayed the first Evidence summary. Each link contains a brief review of the study and notes the reference(s). We now access the fourth Reference Sources option for evidence-based health information – BMJ’s BestPractice – a combination of research evidence, guidelines and expert opinion. We have completed a keyword search for diabetes. Note the drop down menu with the broad category results of the search. The results for the diabetes search are displayed in broad subject categories. Note that each category contains full-text documents on the Highlights, Basics, Prevention, Diagnosis, Treatment, Followup and Resources. HINARI Evidence-Based Journals (other journals may have EBM articles) We have browsed the ‘E’ in the HINARI Find journals by title list and it notes several journals for evidence-based practice. We now search for evidence-based articles using PubMed. From the main HINARI webpage, go to PubMed by clicking on Search HINARI journal articles through PubMed (Medline). Remember you must login to HINARI to have access to the full-text articles. Open the Clinical Queries box. This search tool assigns filters to keyword searches - to locate articles on Clinical Studies, Systematic Reviews and Medical Genetics. In June 2010, these features were revised so that you can complete a search for Clinical Studies, Systematic Reviews and Medical Genetics at the same time. To use the Search by Clinical Study Categories, you would type a disease or procedure in the Search box and select one Category and Scope per search. We have displayed the options for Category and clicked on Therapy from the drop down menu. Note the definition of the Filters on the bottom of the page. Note: you can go directly to PubMed Clinical Queries The direct link to PubMed Clinical Queries is http://www.ncbi.nlm.nih.gov/pubmed/clinical For the Scope option, we will enter Narrow and also enter type 2 diabetes AND developing countries in the search box. The Therapy (Category) and Narrow (Scope) type 2 diabetes AND developing countries search has resulted in 8 citations. We now will click on the See all option. Note that the results for Systematic Reviews and Medical Genetics also are displayed. We have displayed all 8 articles for this search including 7 HINARI and 3 Free Full Text articles. Remember - you can access the full-text articles by clicking on these Filters or changing the display from Summary to Abstract. Note that the specific search is listed in the Search box including the AND (Therapy/Narrow[filter]) for systematic reviews. We have clicked on the See all option for the systematic reviews results. The type 2 diabetes AND developing countries AND systematic [sb] search resulted in 13 articles. If you have a MY NCBI account, you can add Meta-analysis and Systematic Reviews to your Filters. Go to Manage Filters, click on Properties option and put each term in the Search with terms box. When you save a PubMed search, you will be sent an email listing new articles on the specific topic. Remember that you will need to go to HINARI to get the full-text articles. In this example, Free Full Text, HINARI, Meta-analysis and Systematic Reviews are listed in Filters. Additional Evidence-based Health Resources • National Guidelines Clearinghouse http://www.guideline.gov/ • DARE: Database of Abstracts of Reviews of Effects http://www.crd.york.ac.uk/crdweb/ • health-evidence.ca http://health-evidence.ca • The Campbell Library http://www.campbellcollaboration.org/library.php • McMaster PLUS collection http://hiru.mcmaster.ca/hiru/HIRU_McMaster_PL US_projects.aspx • Duke University Medical Center Library: EBM http://www.mclibrary.duke.edu/subject/ebm?tab=co ntents • EBM Librarian • https://sites.google.com/site/ebmlibrarian/ EvidenceUPDATES contain a searchable database, an email alerting system and links to selected evidence-based resources. Registration is required but free. Trip Database is a clinical search tool for health professionals to identify quality clinical evidence for clinical practice. Registration is required but free and gives the users additional resources. The Essential Health Links gateway contains annotated links to numerous Evidence-Based Medicine resources available on the Internet. The Canadian Institutes of Health Research web site contains four Knowledge Translation Learning Modules. Several of these online courses are relevant for evidence based practice and use of knowledge to make informed health decisions. Review/Summary • Evidence-based practice depends on knowing the most recent, valid scientific knowledge. • This involves finding the ‘best’ studies. • Sometimes others have evaluated the quality of the studies, including methodology; many new evidence-based tools mentioned in this tutorial provide evaluation. • When there is no evaluation available, it is essential to evaluate the validity of the study. • Tools for evaluating studies can be found in the Evaluating the Evidence section in the EBM tutorial mentioned earlier and found at: http://www.hsl.unc.edu/Services/Tutorials/ebm/welcome.htm • It is always important to consider studies in terms of applicability to and values of the local patient/situation. • Evidence-based practice is a developing field and new, useful resources are continuously being developed. Appendix 1 Appendix 1 – Contains four case studies for developing Evidence-Based Practice curriculum: experimental cancer research, EBP curriculum for pharmacy students, health literacy for pharmacy students and outreach activity for early intervention providers Developed by: Irena Bond, Library Manager Associate Professor of Library and Learning Resources Massachusetts College of Pharmacy and Health Sciences Research Evidence Practitioner’s Experience Local Conditions Patient/Community Preferences & Values This is the end of the Evidence-based Medicine for HINARI Users module. The material initially was developed by: Gale G. Hannigan, PhD, MLS, MPH; Professor & Medical Informatics Education Librarian, Texas A&M University. Material revised and enhanced by Irena Bond, Library Manager, Associate Professor of Library and Learning Resources, Massachusetts College of Pharmacy and Health Sciences. There is a workbook that accompanies this module. The workbook will take you through a live session covering the topics included in this demonstration with working examples. Updated 2011 08