Evidence-based Resources for HINARI Users
advertisement

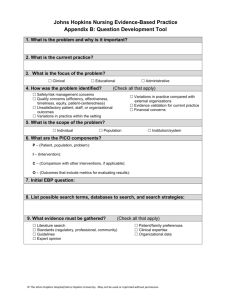
Evidence-based Practice Resources for HINARI Users (Module 7.2) Evidence-based Practice Resources for HINARI Users Instructions - This part of the: course is a PowerPoint demonstration intended to introduce you to Evidence-based Practice and related HINARI resources. module is off-line and is intended as an information resource for reference use. Table of Contents – Part A • Evidence-based Medicine (EBM) – Definition – What, why and how of EBM – 5 step EBM process – ask, access, appraise, apply and access – Limitations of EBM Table of Contents – Part B • HINARI Resources – Clinical Evidence – Cochrane Library – EBM Guidelines – BMJ Practice – Essential Evidence Plus – HINARI EBM Journals Table of Contents – Part C • Other (Internet) Resources: – PubMed’s Clinical Queries and ‘Type of Article’ Limits – Clinical Practice Guidelines – definition & examples – Cochrane Library ‘Abstracts’ – PubMed Health – clinical effective research – Trip Database – Evidence Updates - BMJ and McMaster University – Knowledge Translation Learning Modules – Canadian Institutes of Health Research – Essential Health Links gateway – annotated links – Other useful websites Evidence-based Practice (EBP) Definition "Evidence-Based Practice requires that decisions about health care are based on the best available, current, valid and relevant evidence. These decisions should be made by those receiving care, informed by the tacit and explicit knowledge of those providing care, within the context of available resources." Sicily statement on evidence-based practice. BMC Medical Education, 2005 Jan 5;5(1):1 What is EBP? • The integration of best evidence* from current research, patient preferences and values, and clinical expertise to clinical questions (Sackett, 2000) in a timely fashion. Best Evidence EBP Patient Values/Local Conditions Clinical Expertise *Best available evidence is: consistent research evidence with high quality and quantity Why EBP? • To improve care – To bridge the gap between research & practice – “Kill as few patients as possible” (O. London) – A new treatment might have fewer side effects. – A new treatment could be cheaper or less invasive – A new treatment may be necessary in case people develop resistance to existing therapies, etc. • To keep knowledge and skills current (continuing education) • To save time to find the best information How does EBP help? A patient comes to a clinic with a fresh dog bite. It looks clean and the nurse and patient wonder if prophylactic antibiotics are necessary. The nurse searches PubMed and found a meta analysis indicating that the average infection rate for dog bites was 14% and that antibiotics halved this risk to 7%. • For every 100 people with dog bites, treatment with antibiotics will save 7 from infection • Treating 14 (NNT) people with dog bites will prevent 1 infection • You explain these numbers to the patient along with possible consequences and patient decides not to take antibiotics. On a follow up visit you find out that he did not get infected. Glasziou P, Del Mar C, Salisbury J. EBP Workbook, 2nd. ed. BMJ Books, 2007. What are some Barriers for EBP? • • • • • • Overuse, underuse, misuse of evidence Time, effort, & skill needed Access to evidence Intimidation by senior clinicians Environment not supportive of EBP Poor decision making The 5 Step EBP Process 1. ASK: Formulate an answerable clinical question 2. ACCESS: Track down the best Evidence 3. APPRAISE: Appraise the evidence for its validity and usefulness 4. APPLY: Integrate the results with your clinical expertise and your patient values/local conditions 5. ASSESS: Evaluate the effectiveness of the process Ask Assess Access Apply Appraise Step 1: ASK a focused (answerable) clinical question Ask • Background questions (What do I know about this?) • Foreground (Clinical) Questions P = Patient, population or problem (Who are the patients or populations? What is the disease?) I = Intervention (What do you want to do with this patient (e.g. treat, diagnose, observe)? C = Comparison intervention (What is the alternative to the intervention (e.g. placebo, different drug, nothing?) O = Outcome (What are the relevant outcomes (e.g. morbidity, mortality, death, complications)? Why should I use PICO? • • • To help define problem in clarify it in your own mind To prepare for searching To ask patient centered questions. Treatment of Pneumococcal Pneumonia SHOULD be different for – Terminal Cancer Patient – Elderly, Severely Demented Patient – Young, mother of 2 children • Developing the question requires: – Some background knowledge of the condition – Understanding of the patient and what are the outcomes and beliefs that matter to this patient • Death? Disability? Quality of life? Cost? Improvement of symptoms? Example: Intervention Questions • Identify background questions, create a PICO and a focused clinical question for this case: 54 year old male patient was diagnosed with intermediate grade prostate cancer and wants to know whether to get a radical prostatectomy or radiation treatment. He is concerned about death from prostate cancer and also risks of impotence and incontinence. Formulate the Clinical Question • PICO P - 54 year old male with intermediate grade prostate cancer I - radical prostatectomy C- radiation treatment O- reduce risk of mortality, impotence, and incontinence • Focused clinical question In 54 year old male patients with intermediate grade prostate cancer is radical prostatectomy more effective compared to radiation treatment in reducing the risk of mortality, impotence, and incontinence? EBP Step 1a: Classify the type of the question • What is the treatment? Question of INTERVENTION/PREVENTION • What causes the problem? Question of ETIOLOGY, RISK • Does this person have the problem? Question of DIAGNOSIS • Who (and how likely) will get the problem? Question of PROGNOSIS Etiology and Risk Questions What causes a disease or health condition? • The reverse of intervention questions-they deal with harmful outcomes of an activity or exposure (public health issues) • Develop a clinical question for the case: S. is a smoker and just found out that she is 3 months pregnant. She quit smoking immediately. But she is worried if her developing baby was harmed and if the baby is at risk for having developmental problems. She is asking you if smoking during the first trimester can harm her baby? Etiology or Risk Questions • P-babies of mothers who smoke I-smoking in first trimester C-nothing O-increase risk of developmental problems • Question: Are babies of mothers who smoke during their first trimester at an increased risk of developmental disabilities? Diagnosis Questions • These questions are concerned with how accurate a diagnostic test is in various groups and in comparison to other tests or usually to a “gold standard test”. As part of your clinic assessment of elderly patients, there is a hearing check. You think that a simple whispered voice test is very accurate compared to other methods. You want to do a literature search. What is your question? (1) Glasziou P, Del Mar C, Salisbury J. EBP Workbook, 2nd. ed. BMJ Books, 2007. Example • P-elderly people I-whispered voice test C-no test (or other tests) O-accurate diagnosis of hearing problems • Question: In elderly people, does the whispered voice compared to other tests give an accurate diagnosis of hearing problems? Glasziou P, Del Mar C, Salisbury J. EBP Workbook, 2nd. ed. BMJ Books, 2007. Templates for EBP Questions • For a therapy: In _______(P), what is the effect of _______(I) on ______(O) compared with _______(C)? • For etiology: Are ____ (P) who have _______ (I) at ___ (Increased/decreased) risk for/of_______ (O) compared with ______ (P) with/without ______ (C)? • Diagnosis or diagnostic test: Are (is) _________ (I) more accurate in diagnosing ________ (P) compared with ______ (C) for _______ (O)? • Prevention: For ________ (P) does the use of ______ (I) reduce the future risk of ________ (O) compared with _________ (C)? • Prognosis: Does __________ (I) influence ________ (O) in patients who have _______ (P)? Melnyk B. & Fineout-Overholt E. (2005). Evidence-based practice in nursing & healthcare. New York: Lippincott Williams & Wilkins. EBP Step1b: Decide on the best type of study for question For each type of question there is a hierarchy of evidence Therapy/Prevention RCT>cohort > case control > case series What should I do about this problem? Diagnosis Does this person have the problem? Etiology/Harm cross-sectional study with blind comparison to a gold standard RCT > cohort > case control > case series What causes the problem? Prognosis/Prediction Who will get the problem? RCT >cohort study > case control > case series Frequency and Rate cohort study > cross-sectional study How common is the problem? NOTE: A well designed systematic review of RCTS (randomized controlled trials) is best as it is least biased therefore more valid. Hierarchy of Study Designs for Intervention Least • Randomized Controlled Trial Experimental • Cohort Studies Observational • Case-Controlled Studies Observational • Case reports/Clinical Observations Observational Bias Most Bias To recognize the type of study ask the questions: 1. Is intervention randomly assigned? Yes-RCT; No-Observational study 2. When were the outcomes determined? • After the exposure-cohort study (prospective study) • During the exposure-cross-sectional study • Before the exposure-case-control study (retrospective study based on recall) EBP Step 2: ACCESS Track Down the Best Evidence Access 1. Start “hunting” from the best resource: Match your question to the best medical information resource for this question. • Well designed Systematic Reviews¹ can be a great place to start they contain commentary about validity ¹A systematic review involves the application of scientific strategies, in ways that limit bias, to the assembly, critical appraisal, and synthesis of all relevant studies that address a specific clinical question. Cook DJ, Mulrow CD, Haynes RB. Annals of Internal Medicine March 1, 1997; 126 (5) 376. Track Down Hierarchy of Evidence- Access evidence at the level that will give you the best evidence Filtered & Critically Appraised Expert Opinion and Not Filtered Background info. Most clinically relevant (at the top) Least clinically relevant (at the bottom) Why not get info only from textbooks and review articles? • Texts and review articles? – Dated – perhaps by several years – Often biased • Author chooses article that he/she agrees with (or has written) • Author chooses articles of his/her friends • Author does not identify all the relevant literature • Review’s methods are not explained • These resources help with background knowledge (learn about disease) not foreground (answer the specific clinical question for this patient) Why not get info only from guidelines? • They can assure standards of care but: – Can be biased – May not always be developed by experienced experts – Are not always evidence-based – Can work for most patients but not for all – Can work in some circumstances but not in all – Can be dated – There may not be guidelines for everything Filtered and Critically Appraised Evidence-Based Resources • The Cochrane Library by The Cochrane Collaboration via Wiley – Independent non-for-profit international collaboration – Reviews are among the studies of highest scientific evidence – Minimum Bias: Evidence is included/excluded on the basis of explicit quality criteria – Reviews involve exhaustive searches for all RCT, both published and unpublished, on a particular topic – Abstracts searchable for free on the Internet; complete database is available via HINARI for most countries – 1995- Benefits for using not-evaluated databases for EBM research (PubMed, Cinahl) • • • • Create comprehensive search strategies Conduct systematic reviews of the literature Conduct synonym searching utilizing thesauri Set up and distribute alerts relating to evidencebased medicine • Limit to specific populations & publication types • Utilize EBM built-in filters (search strategies) EBP Step 3: Appraise: Appraise Determine if the results are valid and useful • Appraisal principles (primary and secondary research) – What is the PICO of the study? Does it match my question? – How well was the study done? Is it biased? – What do the results mean? Are they real and relevant? • More: University of Oxford’s Center of EBM: http://www.cebm.net/index.aspx?o=1157 • Tools for evaluating studies can be found in the Evaluating the Evidence section in the EBM tutorial at: http://www.hsl.unc.edu/Services/Tutorials/ebm/welcome.htm EBP Step 4: APPLY: Integrate the results with your clinical expertise and your patient values Apply • Question to ask: – Is the intervention feasible in my settings? – What alternatives are available? – Is my patient so different then those in the study that the results cannot apply ? – Will the potential benefits outweigh the potential harms of treatment ? – What does my patient think? What are his cultural beliefs? – Individual decision making/group decision making/choice – Explaining risks and benefits to patients: https://docs.google.com/View?id=d7k3gkg_679hnvn54c8 • Visual Rx: http://www.nntonline.net/visualrx/ EBP Step 5: ASSESS Assess Evaluate the effectiveness of the process. How am I doing? • • • • Am I asking questions? Am I writing down my information needs? What is my success rate in the EBM steps? How is my searching going? Am I becoming more efficient? • Am I periodically syncing (checking) my skills and knowledge with new developments? • Teach others EBP skills • Keep a record of your questions Limitations of EBP • Limited scope of evidence-it will never be complete • The quality of research available • Keeping it patient centered, cost effective • Evidence from Randomized Controlled Trials for real life patients • Communicating uncertainties • Decision making