Documentation guidelines - Southside Community Services Board
advertisement

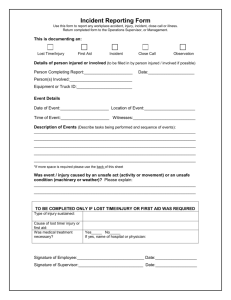
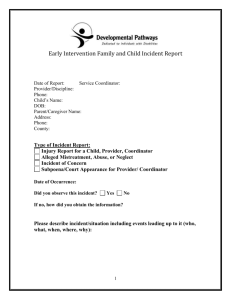
DOCUMENTATION GUIDELINES FOR SCSB QUALITY REPORTING STANDARDS DEFINITIONS • Incident – any event that affects an individual’s safety. • Medical Incident – an incident that occurs involving an individual which requires the implementation of first aid training by staff, the immediate care of a medical professional, or has the potential to cause medical care in the near future and requires monitoring by staff. • Behavioral Incident – an incident in which an individual becomes physically aggressive toward staff or other individuals or threatens another individual while having the ability to carry out the threat. BLAME-FREE ENVIRONMENT Southside Community Services supports a “Blame-Free” Environment: • Employees are mandated to report all incidents, accidents or occurrences. • By getting to the root cause of an error, we can correct the underlying issue that allowed the event to occur; this is the process of learning. INCIDENT/ACCIDENT REPORTS • An incident/accident report should be completed in Credible whenever an event occurs. Examples: Accident (vehicular/nonvehicular) Allegation of Abuse/Neglect Arrested/Detained Assault of or by an individual Choking Fall (including the result of seizure) Fire Injury (minor) Medical Emergency Medication Errors Missing Individual Property Damage/Destruction Self-Injury (without suicidal intent) Seizure Suicidal (thoughts, gestures, attempts) Sexual Incident (allegations, suspicion, observation of harassment, rape, or inappropriate contact/behavior) Theft (agency property) Theft (individual’s property) Threatening Behavior (verbal threats, intimidation, threatening gesture, inappropriate contact) Violent Behavior Other WHEN SHOULD INCIDENTS BE REPORTED? • Anytime an incident occurs in which an individual could have been injured OR whenever there is a deviation from established policy and procedures. • Once the immediate medical needs of the individual are met and the situation is under control. • Employees are required to report the incident as soon as possible. • As soon as possible after the incident has occurred. • People forget 50-80% of what they’ve witnessed after one day and 97% after one month (1). WHY FILE AN INCIDENT REPORT? • Southside Community Services is mandated by DBHDS to file incident reports in a timely manner. • It’s a way for Administration/QA to track emerging trends and to prevent a recurrence of an incident. • Some incidents can result in lawsuits. • If a claim were filed and the case proceeded to court, which could be years after the event, you or anyone else involved might be hardpressed to recreate the scene. ENTERING INCIDENT REPORTS INTO CREDIBLE Examples of Location: Bedroom Classroom Bathroom Dining Room Parking Lot List the people involved in, or who observed, the incident/accident. Ensure that you include the following: Name | Title | Role (e.g. client, staff, visitor, witness…etc.) | Contact Information (e.g. address, worksite, phone #, email..etc.) Betty Rose – Quality Control Specialist – Staff 143 Industrial Parkway Clarksville, VA 23927 1-434-579-6916 brose@sscsb.org Teresa Park – QA Trainer – Staff/Witness 143 Industrial Parkway Clarksville, VA 23927 1-434-579-6916 tpark@sscsb.org Elvis Presley – Client 100 My Home Avenue South Boston, VA 24592 1-434-000-0000 Describe the incident/accident in detail, including circumstances prior to the incident/accident as well as the conditions at the time of the incident/accident. Be sure to include a thorough description of any injuries and/or property damage.* ABC + Spell check Box Adjust (1) WHO was involved in the incident? (4) WHERE did the incident occur? (2) WHAT happened? (5) WHY did the incident occur? (3) WHEN did the incident occur? (6) HOW was the incident handled? Describe immediate actions taken. Include the names of individuals to whom the incident/accident was reported as well as the name of the individual who made the report. Include applicable dates and times.* ABC + Please include the following: What actions did you take? Was First Aid admistered? Did you check vital signs? At what time did you notify: Your Immediate Supervisor Your Program Director The Individual’s Primary Care Physician 911 A/R or Guardian Arrival & Departure time of EMS What facility was individual taken to? Arrival time of A/R or Guardian: To the E.R., Physician’s Office, or to the program. Performed by SCS Staff The Date of Report should be the day that you enter the incident into CREDIBLE. WHO TO NOTIFY FOR AN EMERGENCY INCIDENT? Staff may notify the A/R or Guardian during: After hours Weekends If directed by Supervisor * Never leave an individual alone during an emergency! WHO TO NOTIFY FOR A NONEMERGENCY INCIDENT? Staff may notify the A/R or Guardian during: After hours Weekends If directed by Supervisor GUIDELINES FOR QUALITY REPORTING Regardless of the charting method used, documentation must be: •Objective- Perform assessments using your senses of touch, sight, hearing, and smell, and document facts. •Avoid general statements. •Free of grammatical/spelling errors •Must be completed in a timely manner. •Should include names of all individuals notified/involved, and steps taken. •ACCURATE Chronological order (DATE &TIME) •Abbreviations are to be avoided. •With Dignity and Respect utilized at all times. EXAMPLES OF QUALITY REPORTING Be Precise: Accurately reporting sequences of events will protect you from scrutiny. Poor Example: “Individual fell in the smoking area. Cut his knee, it was cleaned and covered with a piece of gauze. Reported to Jane.” Quality Example: "Individual fell on deck of HDTC smoking area at 0900. He received a 1/2” laceration to his left knee, no other injuries noted, no complaints of pain. BP- 128/74, Pulse -92 , Resp.-22. Individual was able to stand and walk into building without assistance and without difficulty. Area on left knee was cleaned with soap and water using Universal Precautions and Covered with a sterile gauze pad, and held in place with paper tape. Jane Smith, Supervisor was notified of injury to left knee and of treatment provided at 0915. J. Smith, Supervisor advised she will notify the individual’s guardian of injury as well as individual’s physician for further directions. EXAMPLES OF QUALITY REPORTING • Be Objective • Always try to remove personal emotions and opinions from the writing you do. Do not document your feelings, hunches, or viewpoints. • Example: “Patient acting crazy.” This statement relies on staff’s subjective opinion of the individual’s mental state. A better version would be: “Individual pacing back and forth, breathing fast, clenching fists, yelling ‘Don’t touch me!’ repeatedly.” • This provides a clear picture of what actually happened during the incident, allowing the reader to see a clear picture of the individuals actions. EXAMPLES OF QUALITY REPORTING • Record all communication with others. • Your communications with the individual’s , Therapists, Case Manager, Nurse, Physician, Psychiatrist, and/or their AR/Guardian regarding any changes in their physical or behavioral health should be documented, especially if it is in reference to the care of the individual. Recording of this communication allows a reader to track changes and establish clear lines of cause and effect. Be sure to indicate the time contact was made and information that was given. EXAMPLES OF QUALITY REPORTING When providing care to individuals, remember that it is important to: • Follow SCS Board Policy and Procedures. • Standards as trained in; AHA Firstaid/CPR/AED. • The Mandt System • Medication Training ENTERING PEER-TO-PEER INCIDENT REPORTS INTO CREDIBLE WHO was involved in the incident? WHAT happened? WHEN did the incident occur? WHERE did the incident occur? WHY did the incident occur? HOW was the incident handled? PEER-TO-PEER INCIDENTS • When a Peer-to-Peer Incident occurs, staff must report the following in CREDIBLE: 1) Incident/Accident Report 2) Peer-to-Peer Incident Report • If the incident involved (2) or more individuals, staff shall complete an Incident/Accident/P2P report for EACH of the individual’s involved. • Document the MANDT techniques that were used to alleviate the incident. • Removal of stimulus, offer options, least amount of interaction necessary for safety, structured cooling off, active listening. Give description of techniques used. ENTERING SERIOUS INJURY INCIDENT REPORTS INTO CREDIBLE SERIOUS INJURY REPORTS • Serious Injury - any injury that requires medical attention by a licensed professional. • When a Serious Injury Incident occurs, staff must report the following in CREDIBLE: 1) 2) 3) 4) Incident/Accident Report Complete for All Incident Report Serious Injury Report Peer-to-Peer Incident Report IF APPLICABLE • Examples: • Serious physical injury • Loss of consciousness • Attempted suicides • Medication overdoses • Reactions from medications administered or prescribed * Complete these (2) forms whenever an individual requires medical attention from a licensed professional. ENTERING DEATH REPORTS INTO CREDIBLE * Complete these (2) forms whenever a death occurs to an individual that is or has received services in an SCS program. Be sure to include: Date of Death Time of Death Date of Discovery Location How you were informed? Was the individual death referred to a medical examiner? ENTERING MEDICAL ERRORS INTO CREDIBLE WHEN TO REPORT A MEDICATION ERROR? Document in Credible when the following occurs: • Medication Error • Medication Discrepancy • Medication Count Discrepancy • Medication Reaction • Pharmacy Discrepancy • Failure of staff to document on the MAR at the actual time the medication/treatment was actually dispensed or omission of medication. DOCUMENTATION REQUIRED (1) Staff Completes (2) Staff Completes (3) Supervisor Completes * All three options must be completed. DOCUMENTATION TIPS • Be Exact. Describe exactly what your involvement was. How were you involved? Example: If you didn’t see the individual fall, document that you found the individual lying on the floor. • Be Clear. Someone should be able to read your documentation and know exactly what happened, regardless of their background. • Write Objectively. Describe what you heard, what you saw, smelled, touched. Paint a clear picture. • Add Direct Quotes. State the individual’s comments as direct quotes. For example: The individual stated, “I do not feel good and I’m feeling dizzy”. • Be grammatically correct. You are not the only person that sees these reports; be as professional as you can. Remember, these reports are legal documents and can be used in legal proceedings or investigations. QUESTIONS?