PHLEBOTOMY AND SPECIMEN CONSIDERATIONS
advertisement

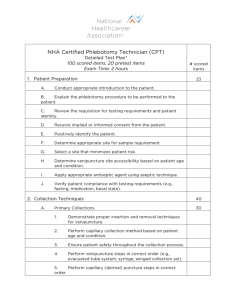
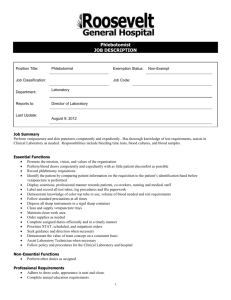
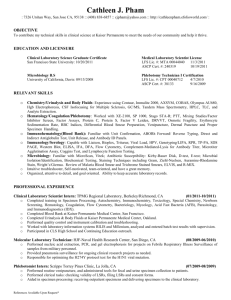
•many errors can occur during these steps, such errors are considered preanalytical errors and are known to contribute to delayed and suboptimal patient care. PHLEBOTOMY AND SPECIMEN CONSIDERATIONS Two classifications of preanalytical variables: 1. Controllable variables relate to standardization of collection, transport, and processing of specimens. 2. Uncontrollable variables are those associated with the physiology of the particular patient (age, sex, underlying disease, etc.) PHLEBOTOMY AND SPECIMEN CONSIDERATIONS PHLEBOTOMY •The process of collecting blood •literally translated means “to cut a vein” PHLEBOTOMY AND SPECIMEN CONSIDERATIONS 2 main phlebotomy procedures: 1. Venipuncture- blood is collected through a needle inserted in the vein 2. Capillary puncture –blood is collected from a skin puncture made with a lancet or similar device •individuals trained in blood collection techniques BLOOD COLLECTION PERSONNEL •Plays an important role in public relations in the laboratory •An assured professional can put the patient at ease and facilitate a positive interaction BLOOD COLLECTION PERSONNEL PROFESSIONALISM 1.Appearance 2.Attitude 3.Communication Skills 4.Bedside Manner INFECTION CONTROL •PPE -lab coats, gloves are required for phlebotomy procedures and during specimen handling -New gloves for each patient -Masks •Hand hygiene -most important means of preventing the spread of infection -Hands must be decontaminated frequently , including after glove removal -Alcohol based antiseptic can be used if hands are not visibly soiled •Isolation - separates certain patients from others and limit their contact with personnel and visitors -Required precaution is posted on patient’s door THE VASCULAR SYSTEM VEINS •have thinner walls because blood in them is under less pressure •Collapse more easily •Dark bluish red (oxygen poor) ARTERIES •Have thick walls to withstand the pressure of ventricular contraction, that creates a pulse •Normal systemic arterial blood is bright red. Capillary • only one cell •Can easily be punctured to provide blood specimen VASCULAR ANATOMY (phlebotomy related) 2 basic patterns of the veins VASCULAR ANATOMY (phlebotomy related) VASCULAR ANATOMY (phlebotomy related) OTHER VEINS: •Veins on the back of the hand or at the ankle may be used, although these are less desirable and should be avoided in diabetics and other individuals with poor circulation. •Leg, ankle and foot veins are sometimes used but not without permission of the patient’s physician due to potential medical complications SOURCE AND COMPOSITION OF BLOOD SPECIMENS ARTERIAL BLOOD Primarily reserved for blood gas evaluation and certain emergency situations VENOUS BLOOD •affected by metabolic activity of the tissue it drains and varies by collection site chloride, glucose, pH, CO2, lactic acid and ammonia levels differ may from arterial blood CAPILLARY BLOOD •Contains arterial and venous blood plus tissue fluid •Capillary glucose is normally higher •Calcium, potassium and total protein are normally lower TYPES OF BLOOD SPECIMENS SERUM PLASMA WHOLE BLOOD VENIPUNCTURE EQUIPMENT Venipuncture can be performed by 3 basic methods I Evacuated tube system (ETS) – most preferred because blood is collected directly from the vein in the tube, minimizing the risk of specimen contamination and exposure to the blood II Needle and syringe – used on small, fragile and damaged veins III Winged infusion set (butterfly) – can be used with the ETS and syringe •Used to draw blood from infants and children, hand veins and other difficult to draw situations VENIPUNCTURE EQUIPMENT 1. Tourniquet •Applied to a patient’s arm during venipuncture •Distends the veins, making them larger and easier to find, stretches the wall so they are thinner and easier to find •Must not be left on longer than 1 minute because specimen quality may be affected VENIPUNCTURE EQUIPMENT 2. Needles •Sterile, disposable and sized by length and gauge Gauge = number that relates to needle diameter or bore • Gauge 21-23 •Gauge 21 – considered standard for routine venipuncture VENIPUNCTURE EQUIPMENT 3. Evacuated Tube System 3 basic components A. Multisample needle – allows collection of multiple tubes during venipuncture VENIPUNCTURE EQUIPMENT •The Vacuum collection needle is pointed at both ends, with one end shorter than the other. •The long end of the needle is used for insertion into the vein, the shorter end is used to pierce the rubber stopper of the vacuum tube and usually is covered by a rubber sheath VENIPUNCTURE EQUIPMENT •The bevel is the slanted opening at the end of the needle. •bevel of the needle must face upward when the needle is inserted into the vein. VENIPUNCTURE EQUIPMENT B. Tube holder •Plastic cylinder with a small opening for a needle at one end and a large opening for tubes at the other end •The tube end has flanges to help place and remove tubes VENIPUNCTURE EQUIPMENT C. Evacuated tubes •Have a premeasured vacuum that automatically draws the volume of blood indicated on the label •Vacuum loss can occur if tubes are stored improperly, opened, dropped or advanced too far onto the needle before draw, or if the needle bevel backs out of the skin during draw •Are color coded to identify a type of additive, absence of additive or special tube property VENIPUNCTURE EQUIPMENT 4. SYRINGE SYSTEM •Syringes are customarily used for patients with veins from which it is difficult to collect blood and for blood gas analysis. VENIPUNCTURE EQUIPMENT 5. BUTTERFLY SYSTEM •A short needle with butterfly wings and a length of tubing with a Luer fitting for syringe use or a Luer adapter for ETS use •Gauge 23 most commonly used •During use , the plastic wings are held with the thumb and index finger, allowing the user to achieve the shallow needle angle needed to access small veins VENIPUNCTURE EQUIPMENT 6. Tube Additives A. Anticoagulants •Prevent blood from clotting and include EDTA, citrates, heparin and oxalates B. Antiglycolitic agents •Prevent glycolysis which can decrease glucose concentration by upto 10 mg/dl per hour •Sodium fluoride : most common antiglycolitic agent Preserves glucose for upto 3 days, and inhibits bacterial growth C. Clot activators •Are coagulation factors like thrombin •Glass particles (silica) •Inert clays ex. Diatomite (celite) Enhance clotting by providing more surface for platelet activation VENIPUNCTURE EQUIPMENT D. Thoxotropic gel separators -inert substances contained near the bottom of certain tubes -during centrifugation the gel lodges between cells and fluid, forming a physical barrier that prevents the cells from metabolizing substances in the serum or plasma VENIPUNCTURE EQUIPMENT 7. Trace element free tubes •Contamination free •Used to collect specimens for trace elements, toxicology, nutrient ORDER OF DRAW AND ADDITIVE CARRY OVER •is a special sequence of tube collection that reduces the risk of specimen contamination by microorganisms Additive carry over •Affects chemistry test •Occurs when blood in an additive tube touches the needle during venipuncture or during transfer from a syringe ORDER OF DRAW AND ADDITIVE CARRY OVER COMMON TESTS AFFECTED BY ADDITIVE CONTAMINATION Citrate – ALP, Ca,Phosporus EDTA - ALP, Ca, CK,PTT,K,PT,Serum Iron, Na Heparin – Activated CT, ACP, Ca, PT, PTT Na, Li Oxalates- ACP, ALP, Amylase,Ca, LDH, PT, PTT, K, Red cell Silica (clot activator) – PTT, PT Sodium fluoride – Na, BUN STOP, LIGHT RED, STAY PUT, GREEN LIGHT, GO S (Sterile) L (Light Blue) R (Red) S (Serum Separator Tube) P (Plasma Separator tube) G (green) L (lavender) G (gray) VENIPUNCTURE PROCEDURES 1. Review and accession of test requests 2. Approach, identify and prepare the patient 3. Verify diet restrictions and latex sensitivity test 4. Sanitize hands 5. Position patient, apply tourniquet and ask patient to make a fist 6. Select vein,release tourniquet and ask patient to open fist 7. Clean and air dry site 8. Prepare equipment and put on gloves 9 .Reapply tourniquet, uncap and inspect needle 10. Ask patient to remake a fist ,anchor vein and insert needle 11. Establish blood flow, release tourniquet and ask patient to open fist 12. Fill, remove and mix tubes in order of draw 13. Place gauze, withdraw needle, activate safety feature and apply pressure 14. Discard needle and holder unit 15. Label tubes 16. Observe Handling Instructions 17. Check patient’s arm, apply bandage 18. Dispose of used materials 19. Thank Patient, Remove Gloves and Sanitize hands. 20. Transport Specimens to the lab. Trouble shooting Failed Venipuncture Tube position Vacuum Bevel against the vein wall Needle too deep Needle beside the vein Collapsed vein Blood cannot be replaced as quickly as it is drawn Use a smaller tube or pull the plunger more slowly If blood does not return, discontinue the draw Undetermined needle position Multiple venipuncture attempts: •Try again below the first site, on the other arm or on a hand or wrist vein. •If the second attempt is unsuccessful, ask someone to take over. Pediatric Venipuncture •Interaction with a child •Immobilizing a child Geriatric Venipuncture • meaningful communication is important •Alzheimer’s disease, arthritis, coagulation problems, clouding of lens or catarcts, hearing loss, skin are less elastic, parkinson’s disease and stroke Preanalytic Considerations Problem sites: •Burn, Scars and Tattoos •Damaged Veins •Edema •Hematoma •Mastectomy Vascular Access Devices: •Arterial line •Arteriovenous shunt or fistula •Heparin or saline lock •Intravenous line •Central Vascular access device (CVAD) or indwelling line PROCEDURAL ERROS RISKS 1. Hematoma formation - rapid swelling near the venipuncture site due to blood leaking into the tissues Situations that can trigger hematoma formation? 2. Iatrogenic anemia 3. Inadvertent arterial puncture 4. Infection of the site 5. Nerve injury 6. Reflux 7. Vein damage Patient Conditions and Complications 1.Allergies to supplies or equipments 2.Excessive bleeding 3.Fainting (syncope) 4.Nausea or vomiting 5.Obese Patients 6.Pain 7.Petechiae 8.Seizures/Convulsions Capillary Specimen Collection -Useful in pediatrics where removal of larger quantities of blood can have serious consequences Collection sites 1. Fingers – adults and children over the age of 2 2. Heels - infants Materials: 1. Alcohol- 70 % alcohol 2. Gauze- to wipe the first drop of blood and excess tissue fluid - hold the pressure after specimen collection 3. Bandage – to cover the site after collection 4. Lancets - sterile, disposable, sharp instruments used for capillary puncture 5. Warming devices – increases blood flow when performing heel sticks ex. Towel or diaper dampend with warm water (<42C) 6. Microcollection Tubes – special small plastic tubes “bullets” 7. Microhematocrit tubes – used for manual hematocrit 8. Sealants – used to seal one end of microhematocrit tubes Capillary Order of Draw 1. EDTA specimens – first because most affected by clumping 2. Other additive specimes 3. Serum specimens Indications for capillary puncture: Adults and Older Children: •There are no accesible veins •Available veins are fragile and must be saved for other procedure •Patient has clot-forming tendencies •Blood is to be obtained for POCT procedures Infants and Very Young Children: •Infants have a small blood volume •Venipuncture is difficult and can damage vein and surrounding tissues •Preferred specimen for newborn screening test Capillary Specimen Collection Steps 1-4 same as venipuncture 5. Position patient 6. Select puncture/ incision site 7. Warm the site if applicable 8. Clean and air dry site 9. Prepare equipment 10. Puncture the site and Discard the lancet\ 11. Wipe away first drop of blood 12.Fill and mix tubes in the order of draw 13. Place gauze and apply pressure 14. Label specimen and observe special handling procedures 15. Check the site and apply bandage 16. Dispose of used materials 17. Thank patient, Remove Gloves and sanitize hands 18. Transport specimen to the lab Heel Stick procedure •Select a site on the medial or lateral plantar surface of the heel that is warm, normal color, free of cuts, bruises, infection, rashes, swelling or previous punctures •Encircle the heel with the index finger around the arch, thumb around the bottom and other fingers around the top of the foot •Place the lancet against the skin on the medial or lateral plantar surface of the heel using enough pressure to keep it in place without deeply compressing the skin •Neonatal Bilirubin Collection – must be protected from light •Neonatal Screening •screens for phenylketonuria, a disorder which could be managed by dietary adjustment if diagnosed early. Specimen Handling and Processing • Mixing tubes – gentle inversion •Transporting Specimens •Delivery time limits - must be centrifuged within 1 hour if serum or plasma is needed Why is prompt separation important? •Cellular glycolysis lowers glucose levels in a specimen at a rate of up to mg/L per hour until the serum or plasma is physically separated from the cells