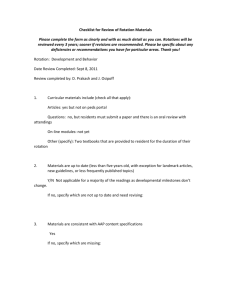
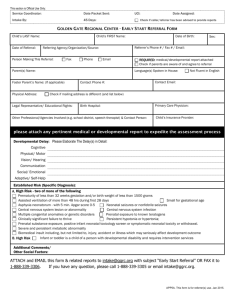
Electronic PEDS:DM and PEDS
advertisement

Why Screen with Validated, Accurate Tools Frances Page Glascoe Professor of Pediatrics Vanderbilt University Outline 1. 2. 3. 4. 5. Who are we detecting Outcomes of Early Intervention Prevalence and detection/referral rates AAP Policy for primary care Challenges from informal approaches/Why quality screens improve detection rates 6. Why trans-disciplinary efforts are needed to improve early detection in primary care 7. How/what quality measures work well in busy clinics 1. Who are we detecting? Those with significant delays and disabilities (16% – 18% of the population). Of this group, common problems are: 1. language impairment (~45%) 2. learning disabilities (~30%) 3. intellectual disabilities (~20%) 4. autism, motor disorders, brain injury, etc. (~5%) Those at-risk due to psychosocial disadvantage, are an additional (10% - 12%) TOTAL = ~ 30% 2. Early Intervention Benefits* Family interest in participation Better outcomes for participants: Higher graduation rates, reduced teen pregnancy, higher employment rates, decreased criminality and violent crime $30,000 to >$100,000 benefit to society (1992 $$s) For every 1$ spent on EI, society saves 17$ * Includes IDEA and Head Start programs 3. Prevalence/Detection Issues 16% - 18% of children have developmentalbehavioral difficulties and need special services Recent research (Pediatrics, July 2008) suggests 13% by age 2! Only 2% - 3% are enrolled in early intervention Only 12% enrolled in special education Enrollment rates in EI should be closer to 8% in the 0 - 4 age range (CDC, www.cdc.gov) 3. Detection/Referral Issues!! Only about 30% of children with substantial delays and disabilities are detected by their health care provider Many of those detected, are not referred Thus most children do not receive the benefits of early intervention that can prevent school failure, high school drop out, etc. 4. Components of the AAP 2006 Policy Statement Eliciting and addressing parents’ concerns Ongoing monitoring of: Health and family history developmental milestones mental health (parent/child) parent-child interactions/psychosocial risk and resilience factors Developmental promotion/parent education Periodic use of screening tests including autism screens at 9, 18 and 24-30 months and well-visits thereafter Holy Smokes! • What? Even more stuff to do at busy wellvisits? 5. Challenges in the 2006 Statement Aren’t we already doing “surveillance”? I’ve got good milestones and questions to parents, aren’t those good enough? So you’re saying I have to screen AND perform surveillance? NO!! With Evidence…. • Surveillance and screening can be accomplished with the same tools Without Evidence….. • Many many problems with early detection 5 (A) Why don’t informal approaches work 1. How do you know your milestones checklists (even if drawn from measures like the Denver) are good predictors of school success? 2. Are your scoring criteria accurate? 5 (A) Sample Checklist—age 4 Uses hungry, tired, thirsty Climbs stairs without holding on Stacks 10 blocks Knows colors Dresses self completely Plays games with rules 5 (A) Quality Measures Have Criteria For example, “Knows Colors” – what exactly does this mean? Match? Points to when named? Names when pointed to? How many colors? 5 (A) Quality measures select items that best predict actual developmental status— and have clear criteria for judging success 5 (B) Why don’t informal approaches work Are you screening the asymptomatic? 5 (C) Why don’t informal approaches work Are you screening repeatedly—at all well-visits? Development develops! Developmental problems do too! Developmental Status by parent's verbal behavior and positive perceptions* Quotients (Glascoe & Leew, Pediatrics, 2010) 110 105 100 95 90 85 80 75 Age in Months 0-5 06 - 11 12 - 17 18 - 24 * Talks at meals, helps child learn new things, reads aloud, able to soothe, enjoys child, perceives child as interested in conversing 5 (D) Why don’t informal approaches work Are you identifying enough kids? What’s your referral rate? 1 out of 400 1 out of 200 1 out of 100 1 out of 25 1 out of 10 1 out of 6 PREVALENCE BY AGE 4 % of 0 - 2 year olds 8% of 0 - 3 year olds 12% of 0 - 4 year olds 16%+ of 0 - 8 year olds 5 (E) Why don’t informal approaches work Are you asking parents quality questions? “Your teacher wishes me to delineate those watershed occasions in your life that have led you to become, slowly and inexorably, a loose cannon.” Sample questions to parents that don’t work well Do you think he has any problems…..? Do you have any worries about her development? 5 (D) If you don’t ask… and ask well…. they don’t always tell! 34% of parents don’t raise developmentalbehavioral concerns without being asked Parents with limited education are less likely to raise concerns spontaneously When developmental-behavioral concerns are raised, children with problems are 11 times more likely to be enrolled in intervention Quality questions about parents’ concerns equalizes ‘the playing field’ for the ‘haves’ and ‘have-nots’ But wait a minute! “Refer without a diagnosis? NNNNNNN” “There’s nothing out there to refer to.” “So many of my kids don’t qualify.” “Many parents don’t follow through.” “I never know what happens after I refer” 5 (E) REFERRAL CHALLENGES • > 80% of referrals from primary care providers made only to familiar services (Glade, Forrest et al Amb Peds, 2002) • Nonmedical providers often fail to respond like the ideal subspecialist (Forrest et al APAM, 1999) • Clinicians often unfamiliar with service options (and with good tools) 6 When Non-Medical Providers Detail Primary Care Enrollment in EI increased from 2% to 12% --commensurate with prevalence ABCD Project, Commonwealth Fund (2007) 70% increase in ASD dx in ages 0 - 3 Minnesota Dept of Education, Pediatrics, 2004 244% increase in referrals to EI Hix-Small et al, Pediatrics,- 2007 How Non-Medical Providers Improved Detection and Referral Rates Arranged a series of short lunch visits Provided laminated lists of local resources for each exam room Called clinics back when referrals were made and after testing Collaborated on finding alternative services Established two-way- consent forms How Non-Medical Providers Improved Detection and Referral Rates Showed options among time-saving tools relying on information from parents Explained billing/coding for optimal reimbursement Described State mandates (and essential record keeping for Medicaid audits) Helped with implementation and work flow issues - 7 What Kinds of Tools are Most Effective for Primary Care and Why? 7 “Oh, by the way…..” Using quality tools with good questions to parents: •Saves providers’ time •Restrains visit length to predicted levels •Ensures reimbursement •Improves detection rates •Increases parent and provider satisfaction and visit attendance • Focuses developmental promotion 7 What Tools are Workable for Primary Care? • PEDS (10 questions eliciting concerns) • PEDS:Developmental Milestones (6 – 8 questions about milestones) • Ages and Stages Questionnaire-3 (30 questions about milestones) • Ages and Stages: Social-Emotional (30 questions about temperament, mental health, etc.) • The M-CHAT at 18 – 24 months What PEDS adds to results of skills-focused screens SKILL FOCUSED: Does your child use three words at a time? YES CONCERNS FOCUSED: Do you have concerns about how your child talks and makes speech sounds? “Yes…. only says the same three words, Wheel of Fortune” over and over.” 7 What Else Do Clinicians Need in Their Armamentarium? • The Family Psychosocial Screen --A good intake form with questions about parental depression (4 items) and psychosocial risk (repeated in the 2nd year of life) • A resilience measure indicating the need for parent-training, such as the Brigance ParentChild Interactions Scale (6 items) administered in the 1st and 2nd year of life. Online Screening Helps! PEDS Online (www.pedstest.com/online) Provides automated scoring Writes referral letters, parent summary reports in Spanish and English Generates billing codes Parents can complete at home or in waiting rooms prior to the encounter. Offers PEDS, PEDS:Developmental Milestones, and the M-CHAT. Summary Good tools for primary care are available Health care providers should avoid ad hoc approaches (and inaccurate measures) Non-medical providers need to collaborate and communicate about early detection and referrals How do we get reimbursed? • First, you must use validated, accurate screens • Add the – 25 modifier to your code for preventive services • Add 96110 (times the number of screens administered) • For private payers, different modifiers may be needed • Have your clinic coordinator find out about private payers • Appeal all denied claims • If a second denial, contact the AAP’s coding hotline