Schizophrenia
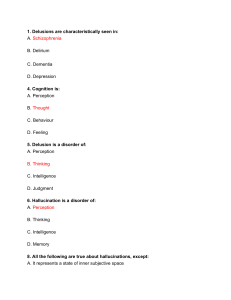
advertisement

Psychopathology Schizophrenia Signs & symptoms Possible Causes Nursing Diagnoses Treatment & care Plans Teaching plans 1 Psychopathology • Prevalence - 20% (12 months period) Anxiety disorder - most prevalent Mood disorder (collectively) Alcohol disorders Major depression • Comorbidity - 17% • Help seeking - 60-80% 2 Understanding Psychopathology • • • • • Organized knowledge - understand Operational definition - communicate Criteria for diagnosis - DSM IV Behavior - subjective/ objective Etiology - nature/nurture 3 Schizophrenia • the most debilitating mental illnesses • Greek terms - "splitting of the mind” • do not have more than one distinct personality • distortions in their perceptions, feelings, and relationships with the world around them. • 1% of the population suffer (in 12 m period) 4 Mild Anxiety Moderate Severe Psychosis Anxiety disorder Somatoform disorders Dissociative disorders Anxiety Cause Physical conditions Grief Personality disorders Major depression The mental health continuum for schizophrenia 5 Epidemiology • 95% of sufferers – lasts a lifetime • 1/3 of homeless suffer from Schizo • 15% no respond to med; 75% partial effective • 20-50% attempt suicide 10% kill themselves • 20% shorter life expectancy • 25% experience secondary depression 6 Causes of Schizophrenia • Genetic factors • Chemical imbalance & physical abnormalities – neurotransmitters, brain structures • Biological factors – age, virus, … • Environmental factors – chr. Life stressors, changes, … 7 Causes - genetic influences • • • • • • Identical twin affected Fraternal twin affected Both parent affected One parent affected Brother or sister affected No affected relative 50% 15% 35% 15% 10% 1% 8 Signs & symptoms • • • • • • • Alterations in personal relationships Alternations of activity Altered perception Alterations of thought Distorted thinking Altered consciousness Alterations of affect 9 Bleular's 4 A's Autism - preoccupation with the self with little concern for external reality Associative looseness - the stringing together of unrelated topics Ambivalence - simultaneous opposite feelings Affective disturbance - inappropriate, blunted, or flattened affect 10 Positive Symptoms - recognizable • Positive (type I) symptoms; delusion (fixed false beliefs), hallucination (false perception) • Excess dopamine in the limbic system -> embellishments of normal cognition and perception • Responsive to antipsychotics 11 Negative Symptoms - what is missing • Lack of affect or energy • Attribute to cortical dysfunction ie atrophy, decreased cerebral blood flow, increased ventricular brain ratios, and a hypodopaminergic state. • Overactive glutamate in the prefrontal cortex stimulates dopamine receptors in the limbic area • Secondary to medications, hospitalization, loss of social support, and economic decline… 12 Diagnostic criteria • S & S - At least 2 of the following: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, negative symptoms • Social/occupational dysfunction • Duration - continuous signs of the disturbance for at least 6 months • Not caused by substance abuse or a general medical disorder 13 Prodromal symptoms • A month or a year before the onset • Deterioration in previous functioning, withdrawn from others, lonely, depressed • Vague plan for the future • Neurotic symptoms ie. Ac /chr anxiety, phobia, difficulty in concentration, misinterpretation, • Feelings of rejection, lack of self-respect, 14 Subjective Signs • Reported by the client • Altered perceptions, thought processes & content, consciousness, and affect • May induce the pt to seek psychiatric help 15 Alterations in thinking • • • • • • • Thought broadcasting Thought insertion Thought withdrawal Delusions of being controlled Delusion of persecution, grandeur, Ideas of reference, somatic delusions, Associative looseness; neologisms; concrete thinking; echolalia; clang association; word salad 16 Alternations in Perception, behavior • Hallucinations – auditory, visual, olfactory, gustatory, tactile • Bizarre behavior – extreme motor agitation, stereotyped behavior, automatic obedience, waxy flexibility, stupor, negativism • Agitated behavior – poor impulse control 17 Objective Signs • Observed directly by nurse • Altered relationships, hygiene, social skills, communication, and psychomotor activity • Frighten others may lead to involuntary psychiatric intervention 18 Subtypes of schizophrenia • Paranoid - preoccupied with one or more delusion • Disorganized - disorganized speech, behavior; poor attention; inappropriate affect • Catatonic - waxy flexibility or purposeless excessive motor activity, mutism, stupor • Undifferentiated • Residual - negative symptoms. 19 Other psychotic disorders • Schizoaffective disorder – Scho symptoms are dominant + major manic or depressive symptoms • Delusional disorder – delusions have basis in reality, but no schizo • Brief psychotic disorder – psychosis lasts less than 1 M • Schizophreniform disorder – 6M < - > 1M 20 Nursing diagnoses • Altered nutrition: less than body requirements • Risk for violence directed at self or others • Self-care deficit: feeding, bathing, dressing/ grooming, toileting • Noncompliance with medications • Ineffective individual/ family coping • Self-esteem disturbance • Altered thought processes 21 Psychotherapeutic management • • • • • • • Provide supportive care Strengthen patient’s self-esteem Treat patients as adults Prevent failure/ embarrassment Respect individuality - unique Reinforce reality Handle hostility calmly & matter-of-factly 22 Issues related to Schizophrenia • Family ⇔ the patient communication, overprotection, blaming • Non-compliance with medical regimen • Caregiver’s needs - cope with strange and frightening behaviors ie. apathy, poor personal hygiene, violence 23 Issues related to Schizophrenia (II) • Depression - part of the symptoms, be masked during acute stage • Relapse - stressors, noncompliance • Stress & coping • Substance abuse -30% have dual Dx., cause (-) effect on the treatment & poor outcomes • Work - no work, inability, no motivation 24 Depression and Suicide in Schizo • Depression is a natural part of schizo • Depression can be masked especially during the acute phase • Depression is a reaction to schizo 25 Delusion & Nursing Intervention • presenting reality, orient pts to time, person & place • avoid argument, touch, competitive activities, • reinforce positive behaviors • encourage verbalization 26 Disruptive Behavior • • • • • Set limit decrease environmental stimuli intervention before acting out close observation safety environment - minimize potential weapons • making contract with the client • using restraints 27 Withdrawn Patients • arrange nonthreatening activities • encourage participation - seating • provide remotivation and resocialization group experience • reinforce appropriate grooming and hygiene • provide psychosocial rehabilitation - social skill training, ... 28 Suspicious Patients • • • • • • Be matter-of-fact; (ie DST for depression) avoid close physical contact - no touch be consistent in activities offer special food avoid whisper Maintain eye contact 29 Hyperactivity Patients • Allow pt to stand for a few min in group • Provide a safe environment • Provide activities that do not require fine motor skills 30 Immobility Patients • Minimize circulatory problem • Provide adequate diet, exercise, and rest • Prevent victimization 31 Nursing interventions • • • • • • • • Medication compliance- 40-60% noncompliance Avoid reinforcing hallucinations & delusion Maintain orientation Use touch minimally and judiciously Avoid easily misinterpreted behavior Reinforce positive behaviors Avoid competitive activities, Allow & encourage expression of feelings 32 Nursing interventionsMilieu management • • • • • • • • clear & realistic limits; consistency; Supportive environment – structured, predictable reduced stimulation early intervention for escalating behavior safety for the pt and others opportunity for nonthreatening social interaction remotivating and resocializing group Communication skills 33 Nursing interventions – Family therapy • Involve the family – use appropriate community resources • Educate the family – chr. dis, S/S of relapse, med compliance, • Provide an outlet for the family – discuss feelings, explore alternative effective coping skills. 34 Psychotherapy • Individual Th – supportive therapy • Group Th – interpersonal skills, family problems, community support • Family Th – expand social network, problem-solving capacity, lower the emotional overinvolvement of families 35 Case Management • Limited hospital stay, 3rd party payment • Discharge planning – transitional care • Partial hospitalization, halfway houses, day treatment programs • Community resources – NAMI, Schizophrenics Anonymous, … 36 Schizophrenia & violence • Myth - tends to be violent – perhaps perpetuated by the media • Fact- more likely to be victims than perpetrators of violence • Violence in this population may be r/t homicidal delusion 37 Schizophrenia and comorbidities • Hypertension, obesity, and diabetes -> death from cardiac disease is higher than in the • Atypical medications create weight gain, worsening cholesterol and triglycerides levels and diabetes • Tobacco use, smoking -> heart disease 38 The Negative Impact of Severe Mental Illness • Impairment – hallucination, depression • Dysfunction – lack of work adjustment skills, social skills, or ADL skills • Disability – unemployment, homelessness • Disadvantage – discrimination, poverty 39 Nurse’s feelings & self-assessment • Pt’s anxiety, loneliness, dependence, distrust -> N’s uncomfort • Feelings of helplessness -> anxiety -> defensive behaviors ie denial, withdrawal, avoidance -> burnout • Peer group supervision can be helpful • Periodic reassessment of Tx goals, 40 Family/care taker education • Teaching about the disease –S/S • Medication teaching and side-effect management • Cognitive & social skills enhancement • Identifying signs of relapse • Attention to deficit in self-care, social and work functioning • Exploration of community resources 41 Signs of Potential Relapse • • • • • Feeling of tension Difficulty concentrating Trouble sleeping Increased withdrawal Increased bizarre/ magic thinking 42 Schizophrenia - overview • • • • Diagnosis - criteria Prevalence - age and gender Course of illness - phases, warning signs Medication management - side effect, coping • Psychosocial rehabilitation - ind, gr, fam… • Community resources • Stress management 43 Review of antipsychotics • • • • • • • Typical & atypical med/ type I & II S/S Clozaril – arrhythmia, agranurocytosis Anticholinergic drugs -> memory impaired High-potency -> EPSEs, NMS Low-potency drugs -> anticholinergic symptoms Half-life of the medication – safety, elderly Reduced rate of relapse (about 2.5 times less) 44 Care of Hallucinations & Delusions • Hallucinations – Content of hallucination – commanding H -> suicidal or homicidal – N’s attitude – nonjudgmental, nonthreatening – Eye contact, louder voice, call the person by name • Delusion – Be empathic - Clarify the reality of the pt’s intent – Clarify misinterpretations of the environment – No argument 45 Great wall, China 46