Chapter 18 - Dr. Gerry Cronin
advertisement

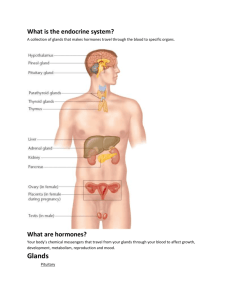
Chapter 18 The Endocrine System Introduction • The nervous and endocrine systems coordinate all of the body systems The nervous system does so through the action of neurons, and the neurotransmitters they secrete The endocrine system uses hormones produced by endocrine structures to produce their effects Types of Hormones • Hormones are simply mediator molecules that have effects on cells in the local environment, or in a distant part of the body Some hormones, called autocrine hormones are local hormones that are secreted, and bind to the same cell. We will see examples of autocrine stimulation when we study the immune system in chapter 22 Types of Hormones • Hormones as mediator molecules … Paracrine hormones are local hormones that are secreted into interstitial fluid and act on nearby cells Types of Hormones • Hormones as mediator molecules … Endocrine hormones are secreted into interstitial fluid and then absorbed into the bloodstream to be carried systemically to any cell that displays the appropriate type of receptor Solubility of Hormones Hormones can be divided into two broad chemical classes. This chemical classification is useful because the two classes exert their effects differently – Lipid soluble hormones bind to receptors in the cytoplasm or nucleus of the cell – Water soluble hormones bind to receptors on the surface of the cell Solubility of Hormones Lipid soluble hormones consist of steroid hormones, thyroid hormones, and the gas nitric oxide – Steroid hormones are derived from cholesterol – Thyroid hormones (T3 and T4) are synthesized by attaching iodine to the amino acid tyrosine – The gas nitric oxide (NO) is both a hormone and a neurotransmitter. Its synthesis is catalyzed by the enzyme nitric oxide synthase Solubility of Hormones • Lipid soluble hormones require a carrier protein for transport in the watery environment of the blood Once they arrive at their destination, however, they are able to freely pass through the plasma membrane to bind to receptors located in the cytoplasm or the nucleus of the target cell Lipid-Soluble Hormone Action Free hormone Blood capillary 1 Lipid-soluble Transport protein hormone diffuses into cell 2 Activated Nucleus Receptor receptor-hormone complex alters gene expression DNA Cytosol mRNA 3 Newly formed mRNA directs synthesis of specific proteins on ribosomes Ribosome New protein 4 New proteins alter cell's activity Target cell Solubility of Hormones Water soluble hormones include peptide and protein hormones (and others with an amine group), and a group of local hormones derived from the arachidonic acid on our cell membranes called eicosanoids – Peptide hormones and protein hormones are amino acid polymers – The two major types of eicosanoids are prostaglandins and leukotrienes – both play a role in mediating the inflammatory response Solubility of Hormones • Water soluble hormones are easy to transport in the watery blood. The plasma membrane of target cells, however, is impermeable to them Water soluble hormones exert their effects by binding to receptors exposed to the interstitial fluid on the surface of target cells • the hormone binding to its receptor acts as the first messenger in a cascade of signal transduction Solubility of Hormones The first messenger (the hormone) then causes production of a second messenger inside the cell, where specific hormone-stimulated responses take place – One common second messenger is cyclic AMP (cAMP). Neurotransmitters, neuropeptides, and several sensory transduction mechanisms (vision) also act via second-messenger systems Water-Soluble Hormone Action Blood capillary 1 Binding of hormone (first messenger) to its receptor activates G protein, which activates adenylate cyclase Water-soluble hormone Adenylate cyclase Receptor Second messenger G protein ATP cAMP 2 Activated adenylate cyclase converts ATP to cAMP Protein kinases 6 Phosphodiesterase inactivates cAMP 3 cAMP serves as a second messenger to activate protein kinases Activated protein kinases 4 Activated protein Protein kinases phosphorylate cellular proteins ATP ADP Protein— P 5 Millions of phosphorylated proteins cause reactions that produce physiological responses Target cell Effects of Hormones • Prostaglandins (PGs) and leukotrienes are eicosanoid hormones with local control. They are synthesized from membrane lipids and have widespread effects PG’s mediate pain, platelet aggregation, fever, and inflammation. They regulate smooth muscle contraction, gastric acid secretion, and airway size • aspirin is a drug that works by inhibiting an enzyme necessary for synthesis of certain PGs: the ones that facilitate pain and the inflammatory response Effects of Hormones Endocrine hormones control a variety of physiological processes. Among other things, they: – Balance the composition and volume of body fluids – Regulate metabolism and energy production – Direct the rate and timing of growth and development – Exert emergency control during physical and mental stress (trauma, starvation, hemorrhage) – Oversee reproductive mechanisms EFFECTS OF HORMONES (Interactions Animation) o Introduction to endocrine hormones: Regulation, secretion and concentration You must be connected to the internet to run this animation Endocrine System Glands Glands that secrete endocrine hormones into the bloodstream are called endocrine glands – They are one of two major types of glands in the body, the other being exocrine glands (which secrete their products into ducts ) In this chapter we will focus our study on the endocrine glands and the widespread effects of endocrine hormones Control of Hormones When stimulated, an endocrine gland will release its hormone in frequent bursts, increasing the concentration of the hormone in the blood – Hormone secretion is regulated by signals from the nervous system, chemical changes in the blood, and other hormones • Most hormonal regulatory systems work via negative feedback, but a few operate via positive feedback Control of Hormones • In a negative feedback system the hormone output reverses a particular stimulus. For example: Blood Ca2+ level is controlled by the parathyroid hormone (PTH). If blood Ca2+ is low, there is a stimulus for the parathyroid glands to release more PTH. PTH then exerts its effects in the body until the Ca2+ level returns to normal. If the level gets too high the body will cease PTH production and secrete calcitonin lower the Ca2+ levels. Control of Hormones • This example shows how PTH and calcitonin have negative feedback influence on one another Control of Hormones In a positive feedback system the hormone output reinforces and encourages the stimulus. For example, during childbirth, the hormone oxytocin stimulates contractions of the uterus, and uterine contractions in turn stimulate more oxytocin release, a positive feedback effect CONTROL OF HORMONES (Interactions Animation) o Hormones Summary You must be connected to the internet to run this animation The Endocrine System The endocrine system consists of the pituitary, thyroid, parathyroid, adrenal and pineal glands – Some of the most important glands of the endocrine system are not exclusively endocrine glands: The hypothalamus, thymus, pancreas, ovaries, and testes are paramount; the kidneys, stomach, liver, small intestine, skin, heart, and placenta also contribute The Endocrine System The Hypothalamus The hypothalamus is the major link between the nervous and endocrine systems – It receives input from several regions in the brain including the thalamus, the RAS, and the limbic system The Pituitary Gland The hypothalamus mainly controls the pituitary gland, which is also called the hypophysis – The pituitary hangs down from the hypothalamus on a stalk called the infundibulum – The gland is divided into an anterior adenohypophysis and a posterior neurohypophysis - the anterior pituitary accounts for about 75% of the total weight of the gland The Adenohypophysis The anterior pituitary (adenohypophysis) is anatomically and functionally connected to the hypothalamus by blood vessels that form a portal system called the hypophyseal portal system – In a portal system, blood flows from one capillary network into a portal vein, and then into a second capillary network before returning to the heart • The name of the portal system indicates the location of the second capillary network The Adenohypophysis Specialized neurosecretory cells in the hypothalamus secrete releasing hormones into the hypophyseal portal system that supplies blood to the anterior pituitary gland The Adenohypophysis • The second capillary system of the hypophyseal portal system delivers the hypothalamic releasing hormones to the anterior pituitary 5 types of anterior pituitary cells secrete seven hormones Anterior Pituitary Hormones Hypothalamus Hormone Growth hormone releasing hormone (GHRH) Thyrotropin releasing hormone (TRH) Prolactin releasing hormone (PRH) Hormone released from Adenohypophysis Major Function/ Target Human Growth Hormone (hGH) Also called somatostatin, stimulates secretion of insulin-like growth factors (IGFs) that promote growth Thyroid Stimulating Hormone (TSH) Stimulates synthesis and secretion of thyroid hormones by the thyroid gland Prolactin (PRL) Stimulates breast growth, and development of the mammary glands Anterior Pituitary Hormones Hypothalamus Hormone Hormone released from Adenohypophysis Major Function/ Target Gonadotropic releasing hormone (GnRH) Follicle Stimulating hormone (FSH) Ovaries initiate development of oocytes; testes initiate development of spermatozoa Gonadotropic releasing hormone (GnRH) Luteinizing hormone (LH) Ovaries stimulate ovulation; testes stimulate testosterone production Anterior Pituitary Hormones Hypothalamus Hormone Corticotropin releasing hormone (CRH) Corticotropin releasing hormone (CRH) Hormone released from Adenohypophysis Major Function/ Target Adrenocorticotropic Hormone (ACTH) Stimulates release of mineralocorticoid, glucocorticoid, and androgen hormones from the adrenal cortex Melanocyte Stimulating hormone (MSH) Stimulate the production and release of melanin by melanocytes in skin and hair. MSH signals to the brain have effects on appetite and sexual arousal ANTERIOR PITUITARY HORMONES (Interactions Animation) hGH Growth and Development • hGH Stimulating Glycogenolysis You must be connected to the internet to run this animation ANTERIOR PITUITARY HORMONES (Interactions Animation) ACTH and Cortisol • Cortisol You must be connected to the internet to run this animation ANTERIOR PITUITARY HORMONES (Interactions Animation) • TRH and TSH You must be connected to the internet to run this animation Anterior Pituitary Hormones • Tropic hormones are hormones produced and secreted by the anterior pituitary that target other endocrine glands All hormones in the previous lists target other endocrine glands (are trophic hormones) except hGH, Prolactin, and MSH, which directly target the end organs The neurohypophysis • The posterior pituitary (neurohypophysis) is embryologically derived from and anatomically connected to the hypothalamus – it releases, but does not synthesize any hormones When stimulated, neurosecretory cells in the hypothalamus release oxytocin and ADH from their axon terminals located in the posterior pituitary The neurohypophysis • Oxytocin targets smooth muscle in the uterus and breasts. In the uterus, oxytocin stimulates uterine contractions, and in response to the sucking from an infant, oxytocin stimulates “milk letdown” in the breasts • ADH targets the collecting ducts in the kidney and sweat glands in the skin to minimize water loss. It also directly causes arterioles to constrict thereby increasing blood pressure The neurohypophysis • This graphic demonstrates the regulation of ADH secretion POSTERIOR PITUITARY HORMONES • Antidiuretic Hormone Animation You must be connected to the internet to run this animation Pituitary Gland Disorders • Acromegaly occurs as a result of excess HGH during adulthood. This disease is marked by enlargement and elongation of the bones of the face, jaw, cheeks, and hands (the long bones of the extremities are unaffected because the growth plates have already closed) Pituitary Gland Disorders • Diabetes Insipidus (DI) is very different from the disease called sugar diabetes (diabetes mellitus) DI is caused by the insufficient release of ADH from the neurohypophysis. Without ADH acting on the collecting ducts in the kidneys, the normal urine output of 1–1.5 liters per day increases to over 2.5 liters per day and dehydration and hypernatremia results The Thyroid Gland • The butterfly-shaped thyroid gland is located inferior to the larynx and anterior to the trachea. It has two laterally placed lobes separated by a bridge-like isthmus The Thyroid Gland • Most of the thyroid gland is composed of spherical groups of follicular cells called thyroid follicles The follicles store a 100-day supply of its two hormones in an inactive gel-like substance called TGB (for thyroglobulin) Thyroid Hormones • TGB is a large glycoprotein made from the oxidation and iodination of molecules of the amino acid. tyrosine • The two hormones released from TGB are: thyroxine or T4 (tetraiodothyronine) and T3 (triiodothyronine) Thyroid Hormones In the blood, T3 and T4 are bound to pre-albumins, albumin, and a specific carrier protein called thyroid-binding globulin (TBG) Most T4 released from the thyroid is converted “peripherally” (by enzymes in the blood) into T3 , which is a more active hormone • Together with hGH and insulin, thyroid hormones accelerate body growth, particularly the growth of the nervous and skeletal systems Thyroid Hormones • Thyroid-stimulating hormone (TSH) is released by the anterior pituitary gland in response to TRH secreted into the portal system The hypothalamus responds to higher circulating levels of T3 and T4 via negative feedback to inhibit TRH secretion 1 Low blood levels of T3 Thyroid Hormone Regulation and T3 or low metabolic rate stimulate release of Hypothalamus TRH 2 TRH, carried by hypophyseal portal veins to anterior pituitary, stimulates release of TSH by thyrotrophs 5 Elevated T3inhibits release of TRH and TSH (negative feedback) TSH 3 TSH released into blood stimulates thyroid follicular cells Anterior pituitary 4 T3 and T4 Thyroid follicle released into blood by follicular cells Actions of Thyroid Hormones: Increase basal metabolic rate Stimulate synthesis of Na+/K+ ATPase Increase body temperature (calorigenic effect) Stimulate protein synthesis Increase the use of glucose and fatty acids for ATP production Stimulate lipolysis Enhance some actions of catecholamines Regulate development and growth of nervous tissue and bones Thyroid Hormones • A goiter is an enlargement of the thyroid gland and may be associated with hyperthyroidism, hypothyroidism, or euthyroidism In many third-word countries dietary iodine intake is inadequate; the resultant low level of thyroid hormone in the blood stimulates secretion of TSH, which causes thyroid gland enlargement The Parathyroid Glands • The parathyroid glands are small, round masses of tissue attached to the posterior surface of the lateral lobes of the thyroid gland There are usually two parathyroid glands attached to each lobe of the thyroid, one superior and one inferior Parathyroid Hormones • Calcitonin (Thyrocalcitonin) is made by the parafollicular (C-cells) of the thyroid gland and when secreted lowers the blood calcium level • An increase in blood calcium will stimulate the C-cells of the thyroid to secrete calcitonin Increased calcitonin will cause a negative feedback inhibition of parathyroid hormone (PTH) which causes a decrease in blood calcium and an increase in blood phosphate levels