Event Handout - CMSA Long Island
advertisement
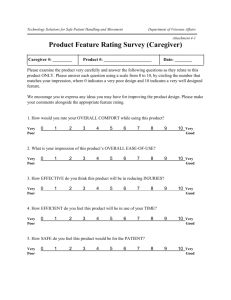
Pre-Activity Assessment Please take a moment to complete the pre-activity assessment prior to the start of the activity. The pre-activity assessment is inside the front of the workbook. Evaluation Form Please take a moment at the conclusion of the activity to complete the evaluation form in the back of the workbook. On-site staff will collect all forms at the conclusion of the activity. Wednesday, April 8, 2015 5:00pm 6:00pm 6:15pm Registration Briefing/Dinner CE Presentation Bristal Assisted Living The Bistro Room 40 Merrik Ave East Meadow, NY 11554 Patricia K. Coyle, MD, FAAN, FANA Professor and Vice Chair Clinical Affairs Director, MS Comprehensive Care Center Professor of Neurology SUNY at Stony Brook Stony Brook, NY Amber Casteel, RN, CCM Chattanooga Chapter CMSA President Chattanooga, TN I Review updated data on the burden of MS, including patients, families, employers, and the health care system II Discussion of new and emerging therapies for the treatment and symptom management of MS III Case Scenarios: Patient-centered treatment and management approaches from a neurologist’s perspective IV Review of effective management strategies for improving overall outcomes from the case manager’s perspective based on evolving interventions and total cost of care V Summary and Q&A Purpose Statement The purpose of this activity is to enhance competence of nurses and case managers concerning the treatment of MS. Target Audience This educational activity is directed toward case managers practicing in the management of Multiple Sclerosis. Sponsor This activity is sponsored by Medical Learning Institute Inc. Commercial Support Acknowledgment This activity is supported by educational grants from Acorda Therapeutics, Inc and Genzyme, a Sanofi company. Registered Nurse Designation Medical Learning Institute Inc Provider approved by the California Board of Registered Nursing, Provider Number 15106, for 1.0 contact hour. Case Manager Designation This program has been pre-approved by The Commission for Case Manager Certification to provide continuing education credit to CCM® board certified case managers. The course is approved for 1.0 CE contact hour. Activity code: C00011511 Approval Number: 140001527 To claim these CEs, log into your CE Center account at www.ccmcertification.org. Upon completion of this activity, the participant will be able to: • Define how the decline in QoL in MS patients impacts productivity • Determine the issues that complicate and interrupt early diagnosis, treatment, and medication adherence • Review current understanding of the treatment and symptom management of MS through case scenarios • Formulate effective, personalized management strategies for improving outcomes and QoL for patients with MS Before the activity, all faculty and anyone who is in a position to have control over the content of this activity and their spouse/life partner will disclose the existence of any financial interest and/or relationship(s) they might have with any commercial interest producing healthcare goods/services to be discussed during their presentation(s): honoraria, expenses, grants, consulting roles, speakers bureau membership, stock ownership, or other special relationships. Presenters will inform participants of any off-label discussions. All identified conflicts of interest are thoroughly vetted by Medical Learning Institute Inc for fair balance, scientific objectivity of studies mentioned in the materials or used as the basis for content, and appropriateness of patient care recommendations. The associates of Medical Learning Institute Inc, the accredited provider for this activity do not have any financial relationships or relationships to products or devices with any commercial interest related to the content of this CE activity for any amount during the past 12 months. Name of Meeting Planner/Manager Company Reported Financial Relationship William Wong, MD Medical Learning Institute Inc Has nothing to disclose. Patricia Coyle, MD, FAAN, FANA is a Consultant for Accordant, Acorda, Bayer, Biogen, Genentech/Roche, Genzyme/Sanofi, Mylan, Novartis, Serono, and Teva. She also received Research Grants for Actelion, Genzyme/Sanofi, Novartis, and Opex. She does not intend to discuss any non-FDA-approved investigational use of any products/devices. Amber Casteel, RN, CCM has nothing to disclose. She does not intend to discuss any non-FDA-approved or investigational use of any products/devices. The information provided at this CE activity is for continuing education purposes only and is not meant to substitute for the independent medical judgment of a healthcare provider relative to diagnostic and treatment options of a specific patient’s medical condition. Recommendations for the use of particular therapeutic agents are based on the best available scientific evidence and current clinical guidelines. No bias towards or promotion for any agent discussed in this program should be inferred. There is no fee for this activity. To receive credit for this CE activity, please take a few minutes to complete the pre-activity assessment and evaluation form and return it to the on-site coordinator. Your confirmation of reported participation will be e-mailed to you within 4 weeks. If you choose to complete this evaluation form off-site, return it by mail or fax to: Medical Learning Institute Inc 203 Main Street, Suite 249 Flemington, NJ 08822 609.333.1694 (fax) For questions regarding the accreditation of this activity, please contact Medical Learning Institute Inc at 609.333.1693 or cgusack@mlicme.org. To claim CEs for Case Managers, log into your CE Center account at www.ccmcertification.org. Patricia Coyle, MD, FAAN, FANA Professor and Vice Chair Clinical Affairs Director, MS Comprehensive Care Center Professor of Neurology SUNY at Stony Brook Stony Brook, NY • Background • Impact features • Cost • Multiple sclerosis (MS) is the most common acquired neurologic disease in young adults1 • At least 400,000 affected in the US2 and 2.3 million worldwide3 • MS is on the rise (among women) • MS affects people who are relatively young (majority are diagnosed between the ages of 20-50 years)3 1] NINDS. MS: hope through research. Accessed Dec 18, 2013. 2] National MS Society. Take action. Accessed Dec 18, 2013. 3] National MS Society. Fact sheet: MS. Accessed Dec 18, 2013. • There is a distinct need for more accurate data on the prevalence of MS in the United States – This information is vital to new drug development, clinical studies, and the funding of resources, programs, and services for patients with MS • Female predominant1 • Two major clinical patterns1 – Relapsing – Progressive • Untreated MS results in disability in the majority of patients over time (cognitive, motor, vocational) • All progressive MS patients become disabled 1] National MS Society. Fact sheet: MS. Accessed Dec 19, 2013. • Disease directly disrupts patient’s daily life • Impact on family and friends (caregiver burden) • Impact on health system/society 1] Wundes A, et al. J Med Econ. 2010;13(4):626-632. • Economic burden – Direct, indirect, and intangible costs – Intangible costs accounted for 17.5%–47.8% of total costs1 – Intangible costs were correlated with worsening disability1 – Productivity loss – Cost of therapies and care • Symptoms and quality-of-life (QoL) issues 1] Wundes A, et al. J Med Econ. 2010;13(4):626-632. • Early diagnosis is important – Paves the way for early counseling and treatment • No single diagnostic test is currently available • Early therapy is likely ideal – Therapy is aimed at reducing future injury/issues – The importance of early treatment must be explained carefully to patients in order to maximize treatment adherence • • • • • • • • • • Depression Fatigue Cognitive issues Spasticity Ambulation difficulties Neurogenic bladder Bowel dysfunction Pain Speech, swallowing, vision issues Sexual dysfunction • Costs increase with disease severity • Mean annual cost to treat MS in US (2009) was $23,434 – DMTs account for 69% of total costs • MS was third highest cost per patient for brain disorders in 2010 Switzerland ($32,412) 1] Naci H, et al. Pharmacoeconomics. 2010;28(5):363-369. 2] Owens GM, et al. J Manag Care Pharm. 2013;19:S42-S53. 3] Maercker A, et al. Swiss Med Wkly. 2013;143:w13751. • Medicare (2006) costs for MS were $23,630 for progressive MS; $5,887 for relapsing MS • Newly diagnosed MS show significantly higher rates of hospitalization/radiology services/ER/OPD visits vs. controls 1] Gilden DM, et al. Value Health. 2011;14(1):61-69. 2] Asche CV, et al. J Manag Care Pharm. 2010;16(9):703-712. • First-line parenterals • Second/third-line parenterals • First-line oral agents • Three interferon β (IFNβ) 1a (IM 30 mcg weekly; SC 44 mcg 3x weekly; SC PEG 125 mcg Q 2 weeks) • Two IFNβ1b (SC 250 mcg every other day) • Glatiramer acetate (20 mg SC daily or 40mg SC 3x weekly) Pros • Tried and true, known entities • Long-term data • Established safety profile Cons • Injectables • Generics are looming, along with more competition 1]Jeffrey S. Medscape News. January 29, 2014. • Natalizumab (300 mg IV monthly) • Mitoxantrone (12 mg/m2 IV every 3 months; lifetime max 140 mg/m2) • Alemtuzumab (12 mg IV daily x 5 days year one; daily x 3 days year two) Pros • High efficacy • Assured compliance • Well tolerated Cons • Increased risk for progressive multifocal leukoencephalopathy (PML) Pros • High efficacy • Assured compliance • Prolonged efficacy (induction agent) Cons • No longer used for MS (in US) • Associated with cardiomyopathy and treatment-related leukemia – FDA recommends that patients who ever received mitoxantrone receive a yearly quantitative LVEF evaluation to detect late-occurring cardiac toxicity. AML indicates acute myeloid leukemia; LVEF, left ventricular ejection fraction. • Humanized IgG1 kappa anti – CD52 monoclonal antibody • Cytolytic antibody depletes T cells (CD4 more than CD8), and to a lesser extent B cells; NK cells; monocytes and dendritic cells •Treatment cycle involves five days of 12 mg/day IV in first year; three days of 12 mg/day IV in year two (given with IV methylprednisolone) •This is induction strategy (effects last ≥ 5 yrs)1 1] Coles AJ, et al. Neurology. 2012;78:1069-1078. Pros • Assured compliance • Therapy over two years involves only 8 days • Long lasting effects/induction therapy • High efficacy Cons • Risks for autoimmune disorders (thyroid 36%, ITP 2%, kidney <1%) • Monthly monitoring for 4 years after last treatment • Prolonged antiviral prophylaxis • 0.5 mg PO daily (0.25 mg dose is being tested) • Sphingosine 1-phosphate receptor modulator (binds to receptor 1, and 3, 4, 5) • Phosphorylated product blocks ability of naïve and central memory T-cells to exit lymph nodes; CCR7- effector memory T-cells are not affected • Also enters CNS to potentially have direct effects • Cardiac, pulmonary, ocular concerns • 14 mg PO daily (7 mg also available) • Cytostatic rapidly dividing (activated) B and T lymphocytes • No affect on resting or slowly dividing lymphocytes • Active ingredient of leflunomide (treatment for RA and psoriatic arthritis) • Pregnancy, hair thinning concerns • 240 mg PO twice a day • Fumaric acid (citric acid energy cycle) ester • Affects Nrf2 oxidative stress, direct effects on lymphocytes and dendritic cells • One of two key components of psoriasis product in Germany • Gastrointestinal, flushing concerns Pros • Oral convenience • Very good efficacy • Well tolerated (for the most part) Cons • Limited experience • Limited safety or efficacy data • Each oral has its own unique adverse events and tolerability issues • Pathogenesis not fully established • No proven therapies for progressive MS (slow worsening) • No CNS restorative therapies • No cure • Every agent shows variable therapeutic response • No biomarkers to select optimal agent, or to determine therapeutic response quickly (personalized medicine) • Current clinical trial outcomes have limitations • Anti-B-cell strategies • Other agents • Anti – CD20s – Rituximab (chimeric) – Ocrelizumab (humanized) – Ofatumumab (human) • Daclizumab – Humanized anti-CD25 monoclonal antibody – Targets activated T- and B-cells – Expands CD56 bright NK cells (may predict treatment response) – Given IV or SC – Completed Phase III trial • Second generation S1P receptor modulators (BAF312; ONO-46414; ponesimod) • Vaccine therapies (Tovaxin, BHT-3009, Neurovax) – Transdermal (myelin peptide) skin patch1 1] Walczak A, et al. JAMA Neurol . 2013;Sept 1;70(9):1105-1109. • Dalfampridine – Potassium channel blocker – Extended release product – 10 mg PO twice daily – Improves ability to walk (in 35 - 43% of patients with all 4 types of MS disease course)1 – Can improve nerve conduction – Contraindicated with seizures or renal impairment 1] Ampyra (dalfampridine) prescribing information. 2013. • Onabotulinumtoxin A – For overactive bladder – Injection into bladder muscles – May need to catheterize • Dextromethorphan (20mg)/Quinidine (10mg) – Pseudobulbar affect1 – Acts on sigma-1, NMDA receptors • Tetrahydrocannabinol / Cannabinoids – Pain/spasticity 1] Nuedexta (dextromethorphan hydrobromide and quinidine sulfate) [prescribing information]. 2010. • MS is in the era of DMTs • Choices are expanding, making therapeutic decisions more complex • We should expect key advances to move us into the next stage – personalized medicine • A.S. is a 25-year-old female recently diagnosed with relapsing MS • She had the disease for three years, with two attacks and complete recovery • She was started on dimethyl fumarate 3 months ago • She is also on vitamin D3, 4000 units daily and vitamin B12, 2000 mcg daily, because her vitamin D25 hydroxy level was 19, and her B12 level was 310 In speaking to the patient, she has been having problems with nausea and vomiting since starting the dimethyl fumarate, and is actually only taking it once a day because she tolerates it much better. She is also only taking her vitamin supplements sporadically. When asked if she has discussed this with her doctor, she states that she has not. On her most recent visit, she didn’t bring any of this up because she didn’t want to interfere with her doctor’s examination. What are the issues in this case? • Non-adherence • Poor knowledge base • Poor side effect management • Poor communication • B.L. is a 36-year-old man with a 5-year history of relapsing MS • He has been on daily injection of SC Glatiramer Acetate • He indicates that he missed a week of work last month when he had bronchitis • He also developed paresthesias of his right leg, and his right knee gave out several times • He is still limping slightly/favoring that leg He never informed his doctor that he usually develops neurologic issues whenever he has significant infections. When asked about his last brain MRI, he conveyed his last MRI was 5 years ago at the time of diagnosis. What are the issues in this case? • Poor knowledge • Poor communication • Unrecognized relapses • Monitoring/surveillance MRI • Suboptimal responder/treatment failure • R.M. is a 54-year-old woman with an 18-year history of MS • She uses a cane or walker to get around – Tends to trip over her toes – Falls frequently • She appears apathetic and sad – Overwhelming fatigue in the afternoon • Patient R.M. rarely leaves the house because of bladder accidents • She complains of painful spasms at night with poor sleep; during the day, her right leg suddenly stiffens painfully for <1 minute; this limits her mobility What are the issues in this case? • Moderate / severe disability • Multiple symptoms poorly managed, if at all – Ambulation / foot drop – Depression – Fatigue – Neurogenic bladder – Spasticity – Pain • Poor sleep hygiene • Social isolation • Fall risk • Unsafe environment Effective Patient Support Strategies The Case Manager’s Perspective Amber Casteel, RN, CCM Chattanooga Chapter CMSA President Chattanooga, TN • Effective care coordination initiatives could result in a staggering $240 billion savings in annual US healthcare costs, according to the Institute of Medicine (IOM)1 • Use of a case manager is a key strategy toward improving patient-centered care coordination – Leads to improved outcomes and reduced costs 1] IOM. 2010. Washington, CD: The National Academic Press. • Facilitate cohesive, patient-centered planning • Communicate: Assist in building strong communication (patient, PCP, neurologist, nutritionist, physical therapist, nurse, speech therapist, social worker) • Advocate for options • Educate • Address Barriers • Implement Interventions • • • • • • • • • • • Clinic models / outpatient settings Managed care organizations/health plans Accountable care organizations, joint ventures Acute care settings Specialty-based settings PCP-based settings Independent case management Rehab-focused settings Vendors Home health care Other settings PCP indicates primary care physician • All case managers use the following domains to assess an individual’s needs and/or barriers to their prescribed plan of care: – – – – – – – Psycho-social function Cultural factors Health literacy and linguistics Financial factors Spiritual and religious functioning Physical and environmental safety Family and community support, or other source of support • It is important for case managers to become well-versed/knowledgeable about the management of MS – This is particularly relevant with respect to treatment-related adverse events and comorbid conditions – Consider adapting approaches from other effective educational models, ie, diabetes, congestive heart failure, other chronic illnesses • Symptoms – Mild or severe • Numbness, tingling or pain • Long duration or short • Other brain and nerve symptoms • Various combination • Sexual symptoms • Muscle • Speech and swallowing • Bowel & bladder • Fatigue • Eye • Each individual has specific needs: – Primary Progressive MS • Disease progression from onset, with occasional plateaus and/or temporary minor improvements • May have one or more superimposed relapses – Secondary Progressive MS • Initial relapsing remitting course followed by progressive; with or without occasional relapse, minimal remission or plateaus • Education is vital to improving outcomes • Symptoms vary • There is no cure, but treatment may help lessen MS attacks, manage symptoms, and reduce disease progression • Be prepared for your visit • Write down any symptoms • Write down important personal info (stress in your life, any recent major changes) • List of medications • Take a family or friend with you • Make a list of questions for the physician • Guidelines as to how to communicate with the physician (succinct, frame questions appropriately) and when to contact the specialist in-between visits • Case managers need resources/tools to coach MS patients on the optimal visit with the neurologist • Case manager’s role in preparing the patient for the face-to-face specialist visit – Develop a 1-page “Top-10” checklist for the patient, to include: • Any new medical or surgical issues; symptom occurrence • All current prescription drugs – Patient can take close-up cell-phone photo of med. bottles • Questions the patient should ask/how to frame the questions • How to communicate with the physician clearly and succinctly • When to contact the physician—not to wait until a crisis arises – Use a template letter; customize variables – Place reminder call/text to patients a day or two before specialist visit to help reduce no-shows • Case managers need resources/tools to help prepare the neurologist for the optimal visit with the patient • Case manager’s role in helping to prepare the neurologist for the MS patient’s visit – Identifying the patient’s key concerns – Listing and prioritizing complex, multiple symptoms, comorbid conditions (tailored to the individual patient) – Generating relevant checklist, process, and tools • Cognitive and depression questionnaire, walking test, others • Create/use a template letter; customize variables – Integration of recommendations for the individual ‘s plan of care should be shared with all members of the team – Placing reminder call to patient a day or two before the appointment—helps reduce no-shows • Additional tests that will be necessary • Progression possibilities • What treatments are available • Treatment options • Side effects of each treatment • How to manage any other health conditions along with MS • Restrictions, if any • Literature, websites, other resources available • Spasticity • Weakness • Trouble with walking • Optic Symptoms • Fatigue – physical and psychological factors – Avoid excessive activity and heat • Depression – treat with meds as appropriate • Pain • Bladder malfunction • Sexual dysfunction Based upon the individual assessment and needs, the case manager will target interventions to reduce and/or remove barriers to care: • Physical therapy, speech • A healthy lifestyle, with good therapy, occupational nutrition, enough rest and therapy, and support relaxation groups • Avoid fatigue, stress, temperature extremes, and illness • Assistive devices, such as wheelchairs, bed lifts, • Suggest changes in what an shower chairs, walkers, individual eats or drinks if there are and wall bars swallowing issues • A planned exercise program early in the course of the disorder • Make changes around the home to prevent falls/home evaluations • Slow Progression: Beta Interferons – Side effects include injection site reaction – Liver damage is a possibility – Requires CBC, liver enzyme, and thyroid monitoring • • • Glatiramer acetate – Side effects are uncommon but may include injection site reactions, flushing, chest pain or heart palpitations Fingolimod – Monitor heart rate for six hours after the first dose because of potential for bradycardia. Need to be immune to the chickenpox virus and vaccinated against the varicella zoster virus. Other side effects may include diarrhea, cough and headache Natalizumab – Increases the risk of progressive multifocal leukoencephalopathy (PML). Requires a blood test that helps detect exposure to the JC virus that causes PML DMT indicates disease-modifying therapy; LFT, liver function test. • • • Mitoxantrone ‒ Can be harmful to the heart; may cause cardiomyopathy and treatment-related leukemia. Maximum lifetime use of 140 mg (m2). No longer used in the US to treat MS. Teriflunomide ‒ This oral medication reduces attacks and lesions in people with MS. LFTs to monitor serious liver damage. Special attention for use during pregnancy! Dimethyl Fumarate • Most common side effects include flushing, abdominal pain, diarrhea, and nausea. May decrease lymphocyte counts, which can increase risk of infection. • Importance of patients and caregivers knowledge of specific types of MS • Patients and caregivers willingness and motivation to “work the plan” (ie, the plan of care) • Need for support of patients and caregivers to continue with health behavior change • Self motivation when symptoms “wax and wane” CMAG indicates Case Management Adherence Guidelines. • • • • • • Identify barriers to following the individual plan of care Help to remove barriers Measure knowledge level Measure willingness to change Assess coping ability Provide linkage to community for support – Patient – Caregiver • Identify/address challenges specific to progressive illness • Assess ability to manage their “normal” lifestyle • Manage routine preventive health issues with chronic diseases • The neurologist and other treatment team members need to ask MS patients whether they have a case manager • If the patient does not have a case manager, the neurologist/treatment team should suggest that patients check with their health plan to determine whether a case manager can be made available to them • There is a need for the neurologist/treatment team to communicate with the PCP about the MS patient’s status and potential red flags (ie, infection triggers MS relapse) • Generate best practices for how to communicate back to the primary care physician and/or medical home – Use a template letter and customize it with key patient information; send it electronically to the PCP – Each venue can develop their own customized tool, ie, form letter or electronic tool, to link/enhance communication • Ask questions • Know when to contact the physician/how to best communicate with the physician • Get plenty of rest • Exercise, as condition allows • Cool down • Eat a balanced diet • Remove stress • Maintain a normal daily lifestyle as much as possible • Stay connected • Enjoy life, pursue hobbies • Identify and address issues affecting access to care and any barriers to treatment adherence • Integrate a holistic approach • Include strategies to enhance health and wellness • Address emotional, social, and vocational challenges • Maximize productivity and independence • Outline approaches for coping with cognitive function • Recommend stress support for the patient and the caregiver • Refer to support group, website, internet, research studies • Equip the caregiver with the knowledge/resources so they are as invested as the MS patient – They should be as knowledgeable as the patient • Check in on the caregiver’s health and well-being – Caregivers often suffer from fatigue, depression, and other health issues • Educate the caregiver – Involve the case manager to help with education/motivational interviewing – Identify whether the caregiver’s health, work, education, routine activities are affected – Develop/offer MS Caregiver workshops at MS Centers, community neurologist office (similar to diabetes workshops held by diabetes educators) • Inform the caregiver about resources available to them: – Respite care – Support groups – Psychological care • Incorporate successful aspects of diabetes, other chronic care models into MS management and communication, with respect to: – Patient/caregiver education and/or workshops – Case manager education – Case manager communication with patient – Case manager communication with physician – Neurologist’s communication with PCP • Templates can be effective, if variables are appropriately customized • • • • • Consortium of MS Centers MS Association of America MS Foundation National Multiple Sclerosis Society: NationalMSSociety.org National Center for Biotechnology Information—MS; Demyelinating Disease: www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001747 • Mayo Clinic--Diseases & Conditions—MS: www.mayoclinic.com/health/multiple-sclerosis/DS00188 • Webmd.com • eMedicine health.com • On-line communities: – Msconnection.org 1. Take steps to determine the accurate prevalence of MS in the United States 2. Determine the full range of MS-associated costs (evident and hidden) 3. Endorse/increase awareness of the availability and value of the case manager among community neurologists and PCPs 4. Involve the case manager proactively, not just in crisis mode, but also when the patient is doing well 5. Case managers need more education/knowledge about MS management, including AEs and comorbid conditions, symptom management 6. Case managers need resources/tools to coach MS patients on the optimal visit with the neurologist 7. Case managers need resources/tools to help prepare the neurologist for the optimal visit with the patient 8. The neurologist and other treatment team members need to ask MS patients whether they have a case manager; if not, patients should be directed to check with their health plan 9. The neurologist/treatment team needs to communicate with the PCP about the MS patient’s status/potential red flags; best practices on how to communicate effectively with the PCP are needed 10. Support the caregiver; provide them with knowledge and resources; check in on them 11. Incorporate successful aspects of diabetes, other chronic care models into MS management and communication